Korean J Orthod.
2010 Dec;40(6):398-410. 10.4041/kjod.2010.40.6.398.
Dentofacial changes of non-orthodontically treated female patients with TMJ disk displacement: a longitudinal cephalometric study
- Affiliations
-
- 1Dental Officer, ROK Army.
- 2Professor, Department of Orthodontics, School of Dentistry, Seoul National University, Korea. taewoo@snu.ac.kr.
- KMID: 1459542
- DOI: http://doi.org/10.4041/kjod.2010.40.6.398
Abstract
OBJECTIVE
The purpose of this study was to investigate the changes in dentofacial morphology of non-orthodontically treated female patients with TMJ disk displacement.
METHODS
The sample consisted of 25 Korean female patients with bilateral TMJ disk displacement who visited the Department of Orthodontics, Seoul National University Dental Hospital from 1996 to 2006. Disk displacements were diagnosed using the magnetic resonance imaging (MRI) of both TMJs. Baseline (T1) and follow-up (T2) lateral cephalograms were analyzed. The mean age of samples at T1 was 18.1 +/- 3.5 years (range 14.2 - 25.8 years) and at T2, 21.1 +/- 3.5 years (range 16.2 - 28.0 years). The mean observation period was 3.0 +/- 1.9 years. Descriptive statistics for each variable were calculated at baseline (T1) and follow-up (T2) stages, and during the observation period (T2-T1).
RESULTS
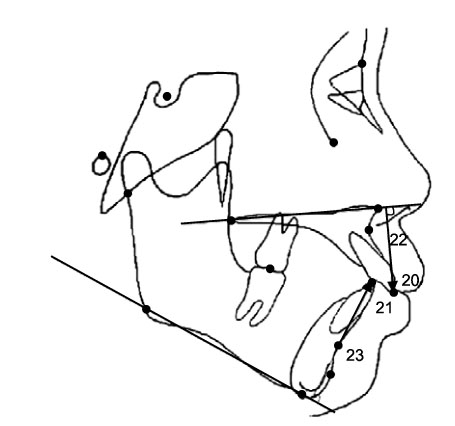
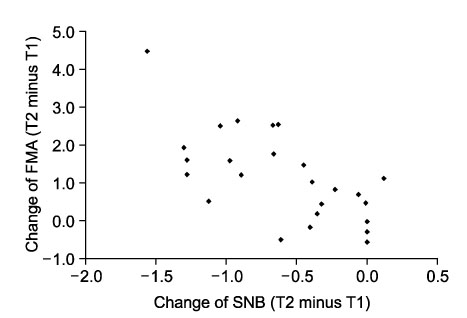
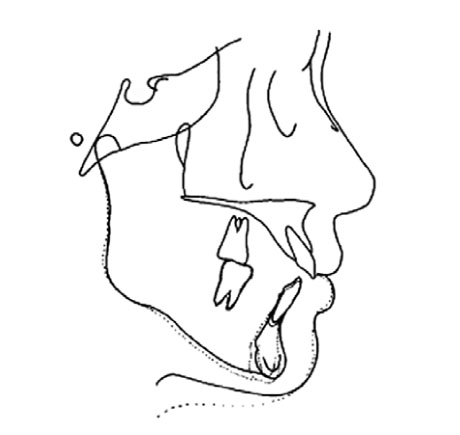
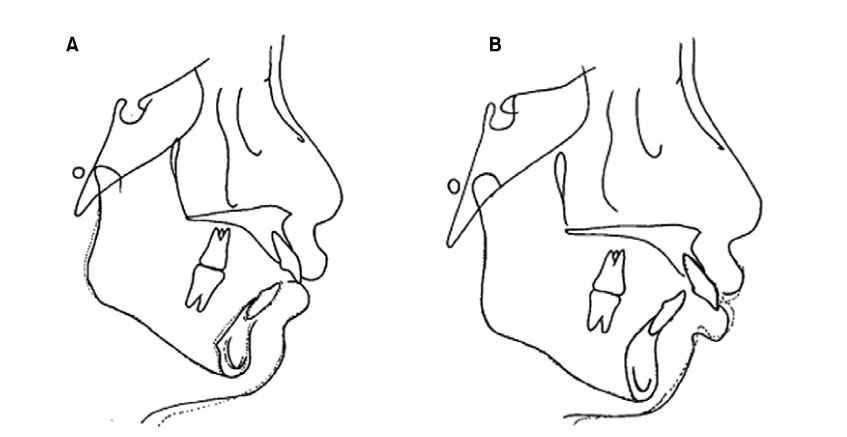
Skeletal changes were found in 64% of the non-orthodontically treated female patients with TMJ disk displacement during the observation period. The L1 to Mandibular plane distance (mm) increased significantly by 0.8 mm (p < 0.01). But there were no significant differences in the other dental relationship variables (overjet, overbite, U1 to palatal plane) during the observation period. Most patients with skeletal changes showed a backward rotation of the mandible. The ratio of the rotation was a decrease of SNB by 0.43degrees for every 1degrees increase of FMA (Spearman rho = -0.660, p < 0.01). A few patients showed a distal shift of the mandible without rotation or significant changes in the vertical dimension.
CONCLUSIONS
During observation periods without orthodontic treatment, non-growing patients with TMJ disk displacement showed dentoskeletal changes, mainly backward rotation of the mandible.
MeSH Terms
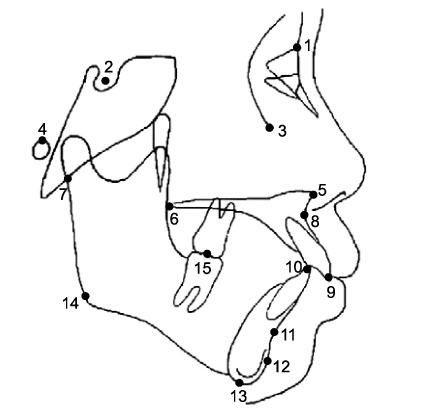
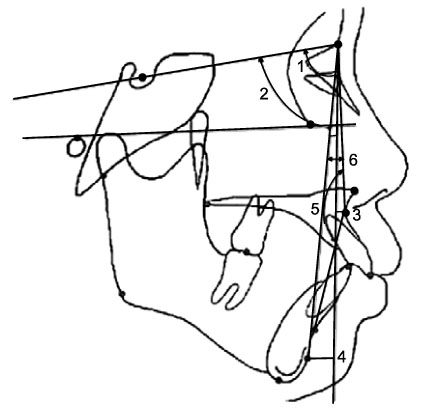
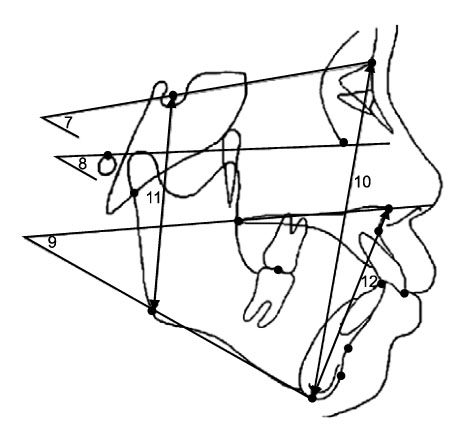
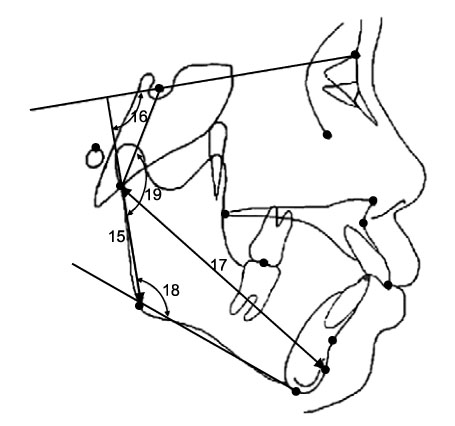
Figure
Reference
-
1. Bowbeer GR. Saving the face and the TMJ. Funct Orthod. 1985. 2:32–44.2. Witzig JW, Yerkes IM. Researchers question dogma of protruded maxilla: findings hint of improper orthodontic treatment. Dentist. 1988. 66:23–49.3. Witzig JW, Yerkes IM. Gelb H, editor. Functional jaw orthopedics: mastering more than technique. Clinical management of head, neck and TMJ pain and dysfunction: a multidisciplinary approach to diagnosis and treatment. 1985. 2nd ed. Philadelphia: WB Saunders;598–618.4. Broadbent JM. Second molar removal, third molar replacement. Funct Orthod. 1986. 3:37–39.5. Spahl TJ, Witzig JW. The clinical management of basic maxillofacial orthopedic appliances. 1987. Littleton (MA): PSG Publishing.6. Spahl TJ. Problems faced by fixed & functional schools of thought in pursuit of orthodontic excellence. Funct Orthod. 1988. 5:28–31.7. Covey EJ. Functional forum: the effects of bicuspid extraction orthodontics on TMJ dysfunction. Funct Orthod. 1990. 7:1–2.8. Sadowsky C, Begole EA. Long-term status of temporomandibular joint function and functional occlusion after orthodontic treatment. Am J Orthod. 1980. 78:201–212.
Article9. Sadowsky C, Polson AM. Temporomandibular disorders and functional occlusion after orthodontic treatment: results of two long-term studies. Am J Orthod. 1984. 86:386–390.
Article10. Pancherz H. The Herbst appliance-its biologic effects and clinical use. Am J Orthod. 1985. 87:1–20.
Article11. Dibbets JM, van der. Orthodontic treatment in relation to symptoms attributed to dysfunction of the temporomandibular joint. A 10-year report of the University of Groningen study. Am J Orthod Dentofacial Orthop. 1987. 91:193–199.
Article12. Dahl BL, Krogstad BS, Ogaard B, Eckersberg T. Signs and symptoms of craniomandibular disorders in two groups of 19-year-old individuals, one treated orthodontically and the other not. Acta Odontol Scand. 1988. 46:89–93.
Article13. Smith A, Freer TJ. Post-orthodontic occlusal function. Aust Dent J. 1989. 34:301–309.
Article14. Sadowsky C, Theisen TA, Sakols EI. Orthodontic treatment and temporomandibular joint sounds-a longitudinal study. Am J Orthod Dentofacial Orthop. 1991. 99:441–447.
Article15. Dibbets JM, van der Weele LT. Extraction, orthodontic treatment, and craniomandibular dysfunction. Am J Orthod Dentofacial Orthop. 1991. 99:210–219.
Article16. Kundinger KK, Austin BP, Christensen LV, Donegan SJ, Ferguson DJ. An evaluation of temporomandibular joints and jaw muscles after orthodontic treatment involving premolar extractions. Am J Orthod Dentofacial Orthop. 1991. 100:110–115.
Article17. Luecke PE 3rd, Johnston LE Jr. The effect of maxillary first premolar extraction and incisor retraction on mandibular position: testing the central dogma of "functional orthodontics". Am J Orthod Dentofacial Orthop. 1992. 101:4–12.
Article18. Artun J, Hollender LG, Truelove EL. Relationship between orthodontic treatment, condylar position, and internal derangement in the temporomandibular joint. Am J Orthod Dentofacial Orthop. 1992. 101:48–53.
Article19. Kremenak CR, Kinser DD, Harman HA, Menard CC, Jakobsen JR. Orthodontic risk factors for temporomandibular disorders (TMD). I: Premolar extractions. Am J Orthod Dentofacial Orthop. 1992. 101:13–20.
Article20. Kremenak CR, Kinser DD, Meicher TJ, Wright GR, Harrison SD, Ziaja RR, et al. Orthodontics as a risk factor for temporomandibular disorders (TMD). II. Am J Orthod Dentofacial Orthop. 1992. 101:21–27.
Article21. Rendell JK, Norton LA, Gay T. Orthodontic treatment and temporomandibular joint disorders. Am J Orthod Dentofacial Orthop. 1992. 101:84–87.
Article22. Hirata RH, Heft MW, Hernandez B, King GJ. Longitudinal study of signs of temporomandibular disorders (TMD) in orthodontically treated and nontreated groups. Am J Orthod Dentofacial Orthop. 1992. 101:35–40.
Article23. Wadhwa L, Utreja A, Tewari A. A study of clinical signs and symptoms of temporomandibular dysfunction in subjects with normal occlusion, untreated, and treated malocclusions. Am J Orthod Dentofacial Orthop. 1993. 103:54–61.
Article24. O'Reilly MT, Rinchuse DJ, Close J. Class II elastics and extractions and temporomandibular disorders: a longitudinal prospective study. Am J Orthod Dentofacial Orthop. 1993. 103:459–463.25. Brooks SL, Brand JW, Gibbs SJ, Hollender L, Lurie AG, Omnell KA, et al. Imaging of the temporomandibular joint: a position paper of the American Academy of Oral and Maxillofacial Radiology. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1997. 83:609–618.26. Cirbus MT, Smilack MS, Beltran J, Simon DC. Magnetic resonance imaging in confirming internal derangement of the temporomandibular joint. J Prosthet Dent. 1987. 57:488–494.
Article27. Rao VM, Farole A, Karasick D. Temporomandibular joint dysfunction: correlation of MR imaging, arthrography, and arthroscopy. Radiology. 1990. 174:663–667.
Article28. Uşümez S, Oz F, Güray E. Comparison of clinical and magnetic resonance imaging diagnoses in patients with TMD history. J Oral Rehabil. 2004. 31:52–56.
Article29. Ahn SJ, Kim TW, Lee DY, Nahm DS. Evaluation of internal derangement of the temporomandibular joint by panoramic radiographs compared with magnetic resonance imaging. Am J Orthod Dentofacial Orthop. 2006. 129:479–485.
Article30. Hassel B, Farman AG. Skeletal maturation evaluation using cervical vertebrae. Am J Orthod Dentofacial Orthop. 1995. 107:58–66.
Article31. Byun ES, Ahn SJ, Kim TW. Relationship between internal derangement of the temporomandibular joint and dentofacial morphology in women with anterior open bite. Am J Orthod Dentofacial Orthop. 2005. 128:87–95.
Article32. Wänman A, Agerberg G. Two-year longitudinal study of signs of mandibular dysfunction in adolescents. Acta Odontol Scand. 1986. 44:333–342.
Article33. Lundh H, Westesson PL, Kopp S. A three-year follow-up of patients with reciprocal temporomandibular joint clicking. Oral Surg Oral Med Oral Pathol. 1987. 63:530–533.
Article34. Greene CS, Laskin DM. Long-term status of TMJ clicking in patients with myofascial pain and dysfunction. J Am Dent Assoc. 1988. 117:461–465.
Article35. Ahn SJ, Lee SJ, Kim TW. Orthodontic effects on dentofacial morphology in women with bilateral TMJ disk displacement. Angle Orthod. 2007. 77:288–295.
Article36. Schellhas KP, Pollei SR, Wilkes CH. Pediatric internal derangements of the temporomandibular joint: effect on facial development. Am J Orthod Dentofacial Orthop. 1993. 104:51–59.
Article37. Wilkes CH. Internal derangements of the temporomandibular joint. Pathological variations. Arch Otolaryngol Head Neck Surg. 1989. 115:469–477.
Article38. Katzberg RW, Keith DA, Guralnick WC, Manzione JV Jr, Ten Eick WR. Internal derangements and arthritis of the temporomandibular joint. Radiology. 1983. 146:107–112.
Article39. Schellhas KP, Wilkes CH, Fritts HM, Omlie MR, Lagrotteria LB. MR of osteochondritis dissecans and avascular necrosis of the mandibular condyle. AJR Am J Roentgenol. 1989. 152:551–560.
Article40. Schellhas KP, Wilkes CH. Temporomandibular joint inflammation: comparison of MR fast scanning with T1- and T2-weighted imaging techniques. AJR Am J Roentgenol. 1989. 153:93–98.
Article41. Schellhas KP. Internal derangement of the temporomandibular joint: radiologic staging with clinical, surgical and pathologic correlation. Magn Reson Imaging. 1989. 7:495–515.
Article42. Schellhas KP, Piper MA, Omlie MR. Facial skeleton remodeling due to temporomandibular joint degeneration: an imaging study of 100 patients. AJNR Am J Neuroradiol. 1990. 11:541–551.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Relationship between disk displacement of temporomandibular joint and dentofacial asymmetry
- Lateral Cephalometric Analysis of Asymptomatic Volunteers and Symptomatic Patients with Temporomandibular Internal Derangement
- The validity of transcranial radiography in diagnosis of internal derangement
- Relationship between rotational disc displacement of the temporomandibular joint and the dentoskeletal morphology
- Analysis of the clinical symptoms and the temporomandibular joint disk by magnetic resonance imaging after conservative treatment with anterior repositioning splint