Korean J Pediatr Gastroenterol Nutr.
2010 Sep;13(2):204-209. 10.5223/kjpgn.2010.13.2.204.
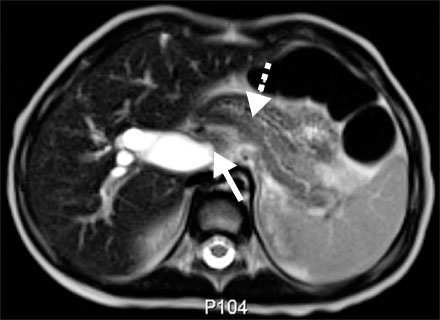
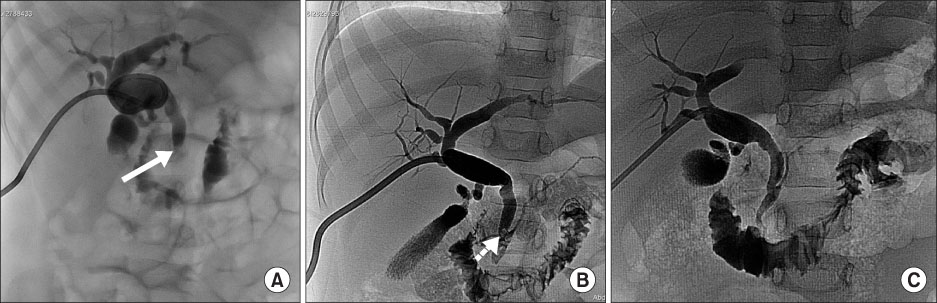
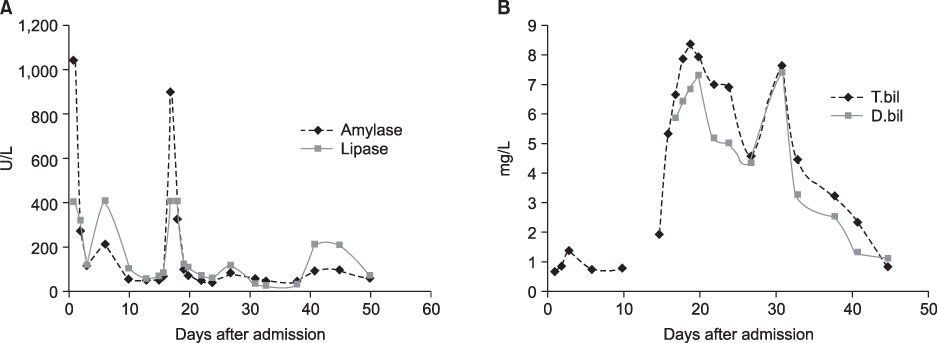
A Case of Obstructive Jaundice Secondary to Traumatic Pancreatitis Treated with Percutaneous Transhepatic Biliary Drainage
- Affiliations
-
- 1Department of Pediatrics, Gyeongsang National University School of Medicine, Gyeongsang Institute of Health Science, Jinju, Korea. hsyoun@gnu.ac.kr
- 2Department of Radiology, Gyeongsang National University School of Medicine, Gyeongsang Institute of Health Science, Jinju, Korea.
- KMID: 1459437
- DOI: http://doi.org/10.5223/kjpgn.2010.13.2.204
Abstract
- Isolated pancreatic trauma and secondary obstructive jaundice in the pediatric population is unusual. Biliary tract obstruction can be a major cause of acute pancreatitis. We report a case of obstructive jaundice secondary to isolated traumatic acute pancreatitis in a previously healthy 32-month-old girl. In our case, secondary obstructive jaundice aggravated the pancreatic inflammation and was successfully treated with percutaneous transhepatic biliary drainage (PTBD).
Keyword
Figure
Cited by 1 articles
-
Percutaneous Transhepatic Biliary Drainage in a Two-Month-Old Infant with Inspissated Bile Syndrome
Sung Hui Chang, Seung-Moon Joo, Choon-Sik Yoon, Kwang-Hun Lee, Soon Min Lee
Yonsei Med J. 2018;59(7):904-907. doi: 10.3349/ymj.2018.59.7.904.
Reference
-
1. Lopez MJ. The changing incidence of acute pancreatitis in children: a single-institution perspective. J Pediatr. 2002. 140:622–624.
Article2. Werlin SL, Kugathasan S, Frautschy BC. Pancreatitis in children. J Pediatr Gastroenterol Nutr. 2003. 37:591–595.
Article3. Moore EE, Cogbill TH, Malangoni MA, Jurkovich GJ, Shackford SR, Champion HR, et al. Organ injury scaling. Surg Clin North Am. 1995. 75:293–303.
Article4. Stringer MD. Pancreatitis and pancreatic trauma. Semin Pediatr Surg. 2005. 14:239–246.
Article5. Mattix KD, Tataria M, Holmes J, Kristoffersen K, Brown R, Groner J, et al. Pediatric pancreatic trauma: predictors of nonoperative management failure and associated outcomes. J Pediatr Surg. 2007. 42:340–344.
Article6. Benifla M, Weizman Z. Acute pancreatitis in childhood analysis of literature data. J Clin Gastroenterol. 2003. 37:169–172.7. Wood JH, Partrick DA, Bruny JL, Sauaia A, Moulton SL. Operative vs nonoperative management of blunt pancreatic trauma in children. J Pediatr Surg. 2010. 45:401–406.
Article8. Dryburgh PR, White JAM. Late obstruction of the intrahepatic common bile duct after seat-belt injury. S Afr Med J. 1980. 58:534–535.9. Choi BH, Lim YJ, Yoon CH, Kim EA, Park YS, Kim KM. Acute pancreatitis associated with biliary disease in children. J Gastroenterol Hepatol. 2003. 18:915–921.
Article10. Ko JS. Fibrosing pancreatitis causing obstructive jaundice. Korean J Gastroenterol. 2008. 52:271–272.11. Yachha SK, Chetri K, Saraswat VA, Baijal SS, Sikora SS, Lal R, et al. Management of childhood pancreatic disorders: a multidisciplinary approach. J Pediatr Gastroenterol Nutr. 2003. 36:206–212.
Article12. Sylvester FA, Shucktt B, Cutz E, Durie PR, Marcon MA. Management of fibrosing pancreatitis in children presenting with obstructive jaundice. Gut. 1998. 43:715–720.
Article13. Wales PW, Shuckett B, Kim PCW. Long-term outcome after nonoperative management of complete traumatic pancreatic transection in children. J Pediatr Surg. 2001. 36:823–827.
Article14. Delcenserie R, Joly JP, Lenne C, Kannoun MM, Sevestre H, Capron JP, et al. Fibrotic stricture of the extrapancreatic biliary tract: a new complication of acute pancreatitis. Two cases. Pancreas. 1995. 10:100–103.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Percutaneous transhepatic biliary drainage
- Percutaneous Transhepatic Transtumoral Biliary Drainage in a Patient with Obstructive Jaundice Due to Klatskin Tumor
- A clinical analysis of percutaneous transhepatic biliary drainage in the patients with obstructive jaundice
- Ultrasonography in obstructive jaundice : a comparison with percutaneous transhepatic cholangiography
- Significance of preoperative percutaneous transhepatic biliary drainage(PTBD) in obstructive jaundice