J Korean Soc Spine Surg.
2010 Jun;17(2):104-110. 10.4184/jkss.2010.17.2.104.
Tardy Spinal Cord Compression without Bone Cement Leakage after Kyphoplasty: A Report of 3 Cases
- Affiliations
-
- 1Department of Orthopedic Surgery, Seoul Sacred Heart General Hospital, Seoul, Korea. niceosu@freechal.com
- KMID: 1459275
- DOI: http://doi.org/10.4184/jkss.2010.17.2.104
Abstract
- STUDY DESIGN: This is a case report.
OBJECTIVE
We report here on three cases of late spinal cord compression without bone cement leakage after kyphoplasty from the view point of the common characteristics, the suspected etiologies and the performed treatments, and we propose a technique to prevent this kind of complication. SUMMARY OF THE LITERATURE REVIEW: Kyphoplasty is widely accepted as an effective and safe treatment for osteoporotic vertebral compression fracture (VCF). Complicated compression fractures and even bursting fractures with a compromised spinal canal are currently indicated for kyphoplasty. The wide spread application of kyphoplasty may be mainly due to reducing the complication rates associated with cement leakage and possible restoration, even though partially, of a vertebral kyphotic deformity.
MATERIALS AND METHODS
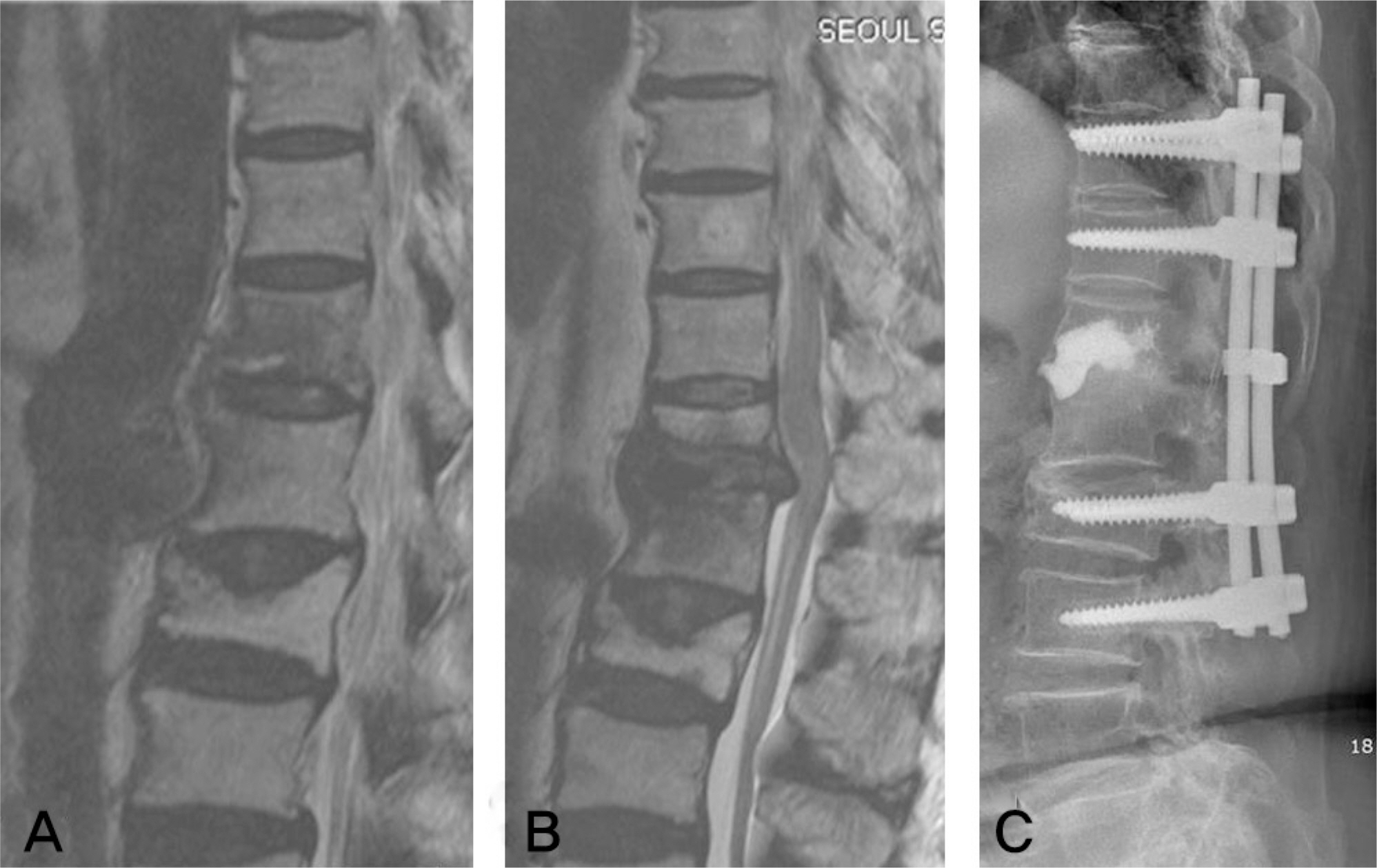
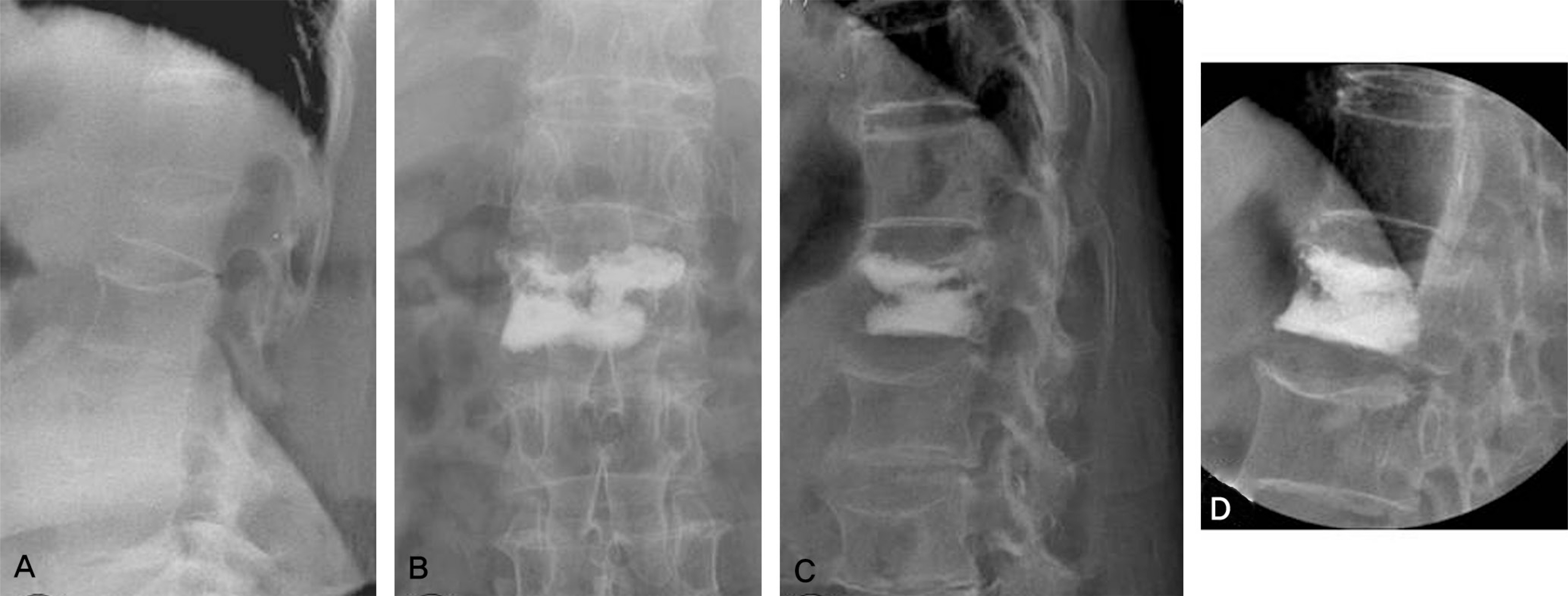
we experienced three cases of newly emerged complications that caused delayed neurologic compromise after uneventful kyphoplasty without any immediate neurologic deficits. MR imaging was done to find the pathologic regions and surgical treatment was performed.
RESULTS
Refracture of an augmented vertebra at the conus medullaris level can cause late occurring spinal cord compression without compromising the spinal canal. Posterior instrumentation and posterior fusion with posterior decompression were effective treatments.
CONCLUSION
The anatomical peculiarity of the conus medullaris and the dynamic irritation of the spinal cord by a bone cement mass after refracture of an augmented vertebral body can be the causes of late spinal cord compression after kyphoplasty. The neurologic symptoms were treated by posterior decompression and fusion. This kind of complication can be prevented by injecting a sufficient amount of bone cement with a shape to support both endplates.
Keyword
MeSH Terms
Figure
Reference
-
1.Kim KT., Suk KS., Kim JM., Park KC. Root injury after percutaneous vertebroplasty in compression fracture: case report. J Korean Soc Spine Surg. 2001. 8:181–5.2.Hiwatashi A., Westesson PL. Vertebroplasty for osteoporotic fractures with spinal canal compromise. Am J Neuroradiol. 2007. 28:690–2.3.Chen JK., Lee HM., Shih JT., Hung ST. Combined extraforaminal and intradiscal cement leakage following percutaneous vertebroplasty. Spine. 2007. 32:358–62.
Article4.Ahn DK., Choi DJ., Lee S., Kim KS., Kim TW., Chun TW. The efficacy of kyphoplasty on osteoporotic vertebral compression fracture: A 1-year follow-up study. J Korean Soc Spine Surg. 2009. 16:79–88.5.Pradhan BB., Bae HW., Kropf MA., Patel VV., Delamarter RB. Kyphoplasty reduction of osteoporotic vertebral compression fractures: correction of local kyphosis versus overall sagittal alignment. Spine. 2006. 31:435–41.
Article6.Lin WC., Lee YC., Lee CH, et al. Refractures in cemented vertebrae after percutaneous vertebroplasty: a retrospective analysis. Eur Spine J. 2008. 17:592–9.
Article7.Shin DA., Kim KN., Shin HC., Kim SH., Yoon DH. Progressive collapse of PMMA-augmented vertebra: a report of three cases. Zentralbl Neurochir. 2008. 69:43–6.
Article8.Huntoon EA., Schmidt CK., Sinaki M. Significantly fewer refractures after vertebroplasty in patients who engage in back-extensor-strengthening exercises. Mayo Clin Proc. 2008. 83:54–7.
Article9.Grey HD., Clemente C. The text book of anatomy of the human body. 13th ed.Philadelphia: Lea & Febiger;p. 960–1. 1985.10.Watanabe K., Lenke LG., Bridwell KH., Kim YJ., Koester L., Hensley M. Proximal junctional vertebral fracture in adults after spinal deformity surgery using pedicle screw constructs: analysis of morphological features. Spine. 2010. 35:138–45.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Benign Cement Leakage after Kyphoplasty: A report of 2 cases
- Acute Paraparesis Caused by Spinal Epidural Fluid After Balloon Kyphoplasty for Traumatic Avascular Necrosis: A Case Report
- Cement Leakage into Disc after Kyphoplasty: Does It Increases the Risk of New Adjacent Vertebral Fractures?
- Minimally Invasive Treatment of Painful Osteoporotic Vertebral Fractures
- Open Surgery for Osteoporotic Compression Fracture Within One Month of Single Level Balloon Kyphoplasty