J Korean Assoc Oral Maxillofac Surg.
2010 Feb;36(1):28-38. 10.5125/jkaoms.2010.36.1.28.
Clinical analysis of early reoperation cases after orthognathic surgery
- Affiliations
-
- 1Department of Oral and Maxillofacial Surgery, Graduate School, Seoul National University, Korea. seobm@snu.ac.kr
- 2Dental Research Institute, Korea.
- 3BK 21, Korea.
- 4Biotooth Engineering Lab, Korea.
- KMID: 1457816
- DOI: http://doi.org/10.5125/jkaoms.2010.36.1.28
Abstract
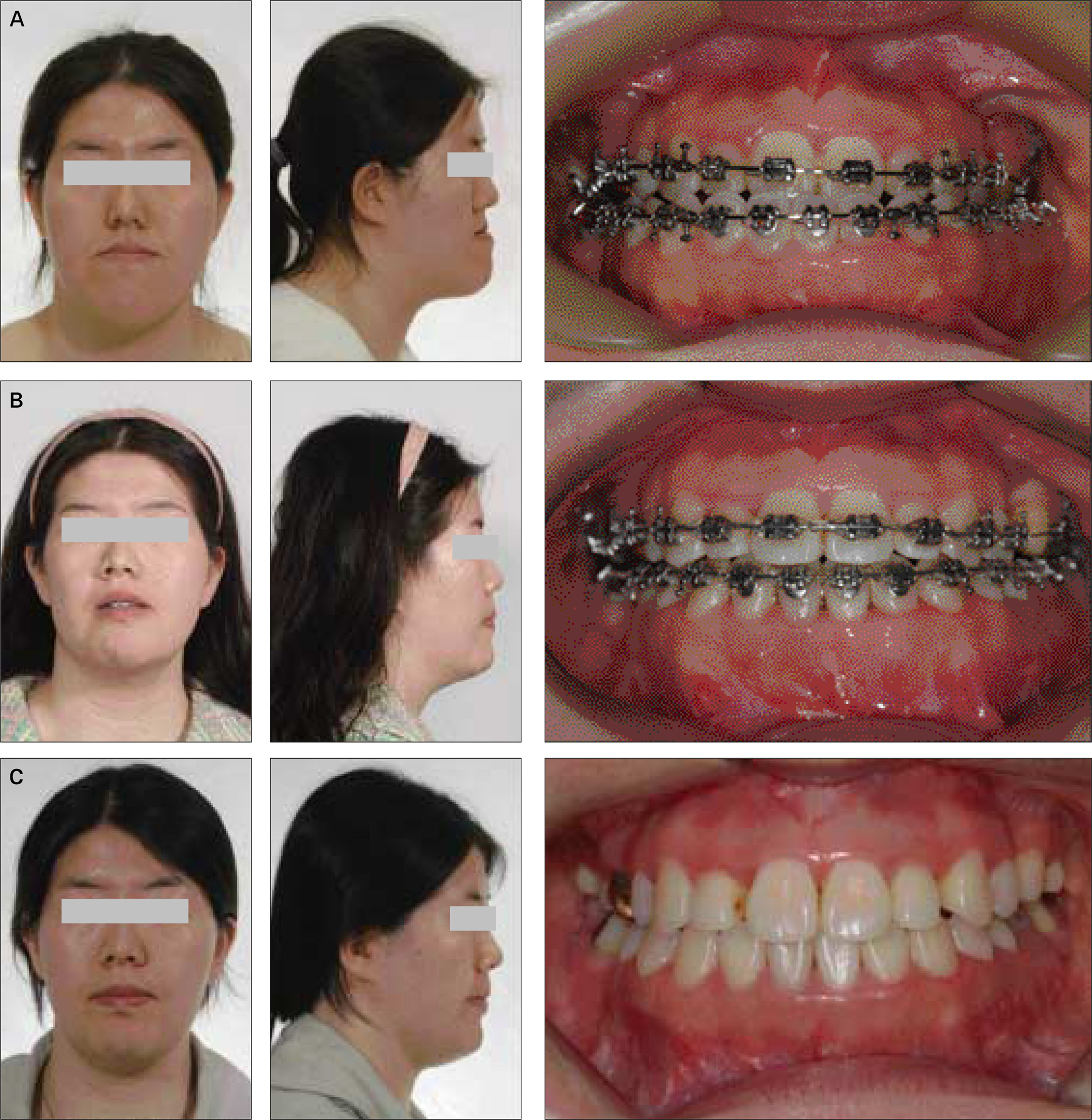
- The factors influencing the relapse and recurrence of skeletal deformity after the orthognathic surgery include various factors such as condylar deviation, the amount of mandibular set-back, stretching force by the soft tissues and muscles around the facial skeleton. The purpose of this report is to recognize and analyze the possible factors of reoperation after orthognathic surgery, due to early relapses. Six patients underwent reoperation after the orthognathic surgeries out of 110 patients from 2006 to 2009 were included in this study. In most cases, clincal signs of the insufficient occlusal stability, anterior open bite, and unilateral shifting of the mandible were founded within 2 weeks postoperatively. Although elastic traction was initiated in every case, inadequate correction made reoperation for these cases inevitable. The chief complaints of five cases were the protruded mandible combined with some degree of asymmetric face and in the other one case, it was asymmetric face only. Various factors were considered as a major cause of post-operative instability such as condylar sagging, counter-clockwise rotation of the mandibular segment, soft tissue tension related with asymmetrical mandibular set-back, preoperatively existing temporomandibular disorder (TMD), poor fabrication of the final wafer, and dual bite tendency of the patients.
MeSH Terms
Figure
Cited by 1 articles
-
Complications associated with orthognathic surgery
Young-Kyun Kim
J Korean Assoc Oral Maxillofac Surg. 2017;43(1):3-15. doi: 10.5125/jkaoms.2017.43.1.3.
Reference
-
References
1. Paulus GW, Steinhauser EW. A comparative study of wire osteosynthesis versus bone screws in the treatment of mandibular prognathism. Oral Surg Oral Med Oral Pathol. 1982; 54:2–6.
Article2. Phillips C, Zaytoun HS, Thomas PM, Terry BC. Skeletal alterations following TOVRO or BSSO procedures. Int J Adult Orthodon Orthognath Surg. 1986; 1:203–13.3. Komori E, Aigase K, Sugisaki M, Tanabe H. Cause of early skeletal relapse after mandibular setback. Am J Orthod Dentofacial Orthop. 1989; 95:29–36.
Article4. Kobayashi T, Watanabe I, Ueda K, Nakajima T. Stability of the mandible after sagittal ramus osteotomy for correction of prognathism. J Oral Maxillofac Surg. 1986; 44:693–7.
Article5. Will LA, Joondeph DR, Hohl TH, West RA. Condylar position following mandibular advancement: its relationship to relapse. J Oral Maxillofac Surg. 1984; 42:578–88.
Article6. Van Sickels JE, Larsen AJ, Thrash WJ. Relapse after rigid fixation of mandibular advancement. J Oral Maxillofac Surg. 1986; 44:698–702.
Article7. Epker BN, Wessberg GA. Mechanisms of early skeletal release following surgical advancement of the mandible. Br J Oral Surg. 1982; 20:175–82.8. Reyneke JP, Ferretti C. Intraoperative diagnosis of condylar sag after bilateral sagittal split ramus osteotomy. Br J Oral Maxillofac Surg. 2002; 40:285–92.
Article9. Stella JP, Astrand P, Epker BN. Patterns and etiology of relapse after correction of Class III open bite via subcondylar ramus osteotomy. Int J Adult Orthodon Orthognath Surg. 1986; 1:91–9.10. Leonard MS, Ziman P, Bevis R, Cavanaugh G, Speidel MT, Worms F. The sagittal split osteotomy of the mandible. Oral Surg Oral Med Oral Pathol. 1985; 60:459–66.
Article11. Yellich GM, McNamara JA, Ungerleider JC. Muscular and mandibular adaptation after lengthening, detachment, and reattachment of the masseter muscle. J Oral Surg. 1981; 39:656–65.12. Ellis E 3rd, Carlson DS. Stability two years after mandibular advancement with and without suprahyoid myotomy: an experimental study. J Oral Maxillofac Surg. 1983; 41:426–37.
Article13. Chow LK, Singh B, Chiu WK, Samman N. Prevalence of postoperative complications after orthognathic surgery: a 15-year review. J Oral Maxillofac Surg. 2007; 65:984–92.
Article14. MacIntosh RB. Experience with the sagittal osteotomy of the mandibular ramus: a 13-year review. J Maxillofac Surg. 1981; 9:151–65.
Article15. Singer RS, Bays RA. A comparison between superior and inferior border wiring techniques in sagittal split ramus osteotomy. J Oral Maxillofac Surg. 1985; 43:444–9.
Article16. Kundert M, Hadjianghelou O. Condylar displacement after sagittal splitting of the mandibular rami. A short-term radiographic study. J Maxillofac Surg. 1980; 8:278–87.17. Bell WH, Jacobs JD. Tridimensional planning for surgical/ortho-dontic treatment of mandibular excess. Am J Orthod. 1981; 80:263–88.
Article18. Link JJ, Nickerson JW. Temporomandibular joint internal derangements in an orthognathic surgery population. Int J Adult Orthodon Orthognath Surg. 1992; 7:161–9.19. Costa F, Robiony M, Toro C, Sembronio S, Polini F, Politi M. Condylar positioning devices for orthognathic surgery: a literature review. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008; 106:179–90.
Article20. Gateno J, Miloro M, Hendler BH, Horrow M. The use of ultrasound to determine the position of the mandibular condyle. J Oral Maxillofac Surg. 1993; 51:1081–6. discussion 1086-7.
Article21. Bettega G, Cinquin P, Lebeau J, Raphae ¨l B. Computer-assisted orthognathic surgery: clinical evaluation of a mandibular condyle repositioning system. J Oral Maxillofac Surg. 2002; 60:27–34. discussion 34-5.
Article22. Politi M, Toro C, Costa F, Polini F, Robiony M. Intraoperative awakening of the patient during orthognathic surgery: a method to prevent the condylar sag. J Oral Maxillofac Surg. 2007; 65:109–14.
Article23. Reitzik M. Skeletal and dental changes after surgical correction of mandibular prognathism. J Oral Surg. 1980; 38:109–16.24. Rodrl′guez RR, Gonza ′ lez M. Skeletal stability after mandibular setback surgery. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1996; 81:31–3.25. Hunsuck EE. A modified intraoral sagittal splitting technic for correction of mandibular prognathism. J Oral Surg. 1968; 26:250–3.26. Epker BN. Modifications in the sagittal osteotomy of the mandible. J Oral Surg. 1977; 35:157–9.27. Wolford LM, Bennett MA, Rafferty CG. Modification of the mandibular ramus sagittal split osteotomy. Oral Surg Oral Med Oral Pathol. 1987; 64:146–55.
Article28. Kim MJ, Kim SG, Park YW. Positional stability following intentional posterior ostectomy of the distal segment in bilateral sagittal split ramus osteotomy for correction of mandibular prognathism. J Craniomaxillofac Surg. 2002; 30:35–40.
Article29. Ellis E 3rd. A method to passively align the sagittal ramus osteotomy segments. J Oral Maxillofac Surg. 2007; 65:2125–30.
Article30. Koudstaal MJ, Poort LJ, van der Wal KG, Wolvius EB, Prahl-Andersen B, Schulten AJ. Surgically assisted rapid maxillary expansion (SARME): a review of the literature. Int J Oral Maxillofac Surg. 2005; 34:709–14.
Article31. Motohashi N, Kuroda T. A 3D computer-aided design system applied to diagnosis and treatment planning in orthodontics and orthognathic surgery. Eur J Orthod. 1999; 21:263–74.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Complications associated with orthognathic surgery
- Full-mouth rehabilitation by immediate implantation combined with orthognathic surgery: a clinical report
- Cliniclal Analysis of Microsurgical Reoperation after Lumbar Disc Surgery
- Paradigm Shift in Orthognathic Surgery: Surgery First Orthognathic Approach and Aesthetic Two-jaw Surgery
- Two treatment approach to skeletal Class III : A case report on sisters