J Korean Fract Soc.
2011 Jan;24(1):100-113. 10.12671/jkfs.2011.24.1.100.
Lower Cervical Spine Injury
- KMID: 1449426
- DOI: http://doi.org/10.12671/jkfs.2011.24.1.100
Abstract
- No abstract available.
MeSH Terms
Figure
Reference
-
1. Aebi M, Zuber K, Marchesi D. Treatment of cervical spine injuries with anterior plating. Indications, techniques, and results. Spine (Phila Pa 1976). 1991. 16:3 Suppl. S38–S45.2. Ahn JS, Lee JK, Yang JY, Lee HH. Change of the lordosis on cervical spine after anterior interbody fusion with autogenous iliac strut bone graft. J Korean Soc Spine Surg. 2001. 8:468–474.
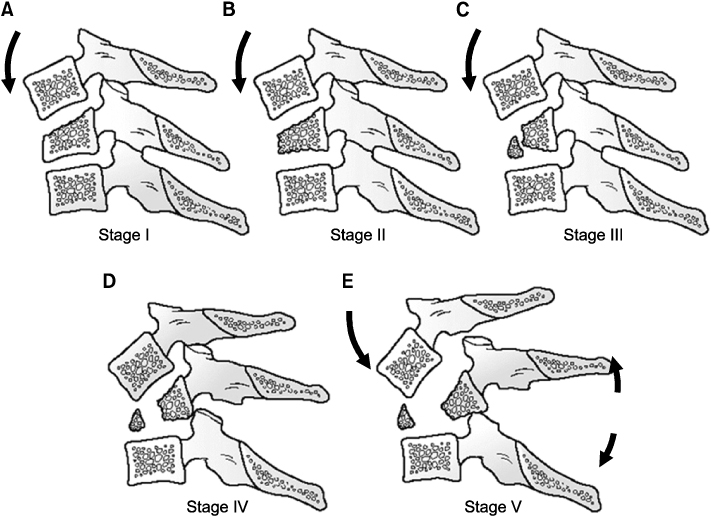
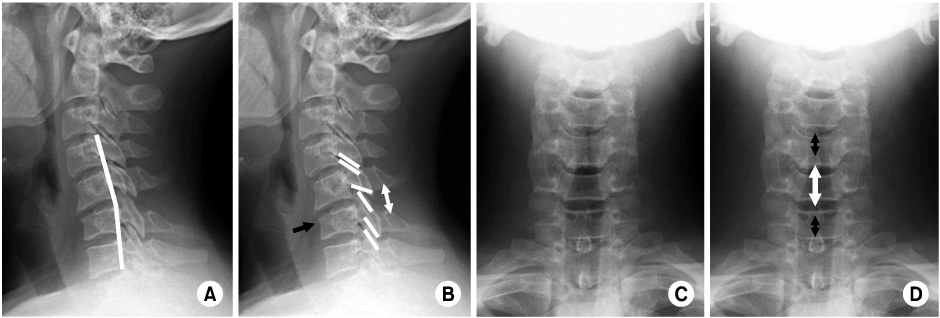
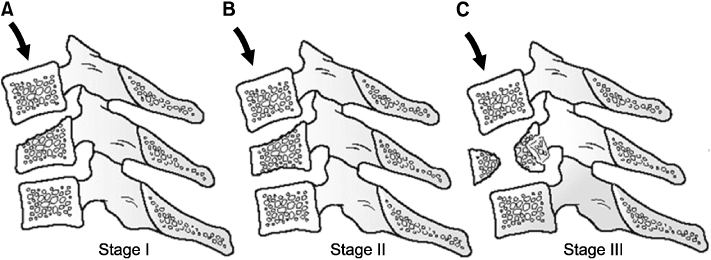
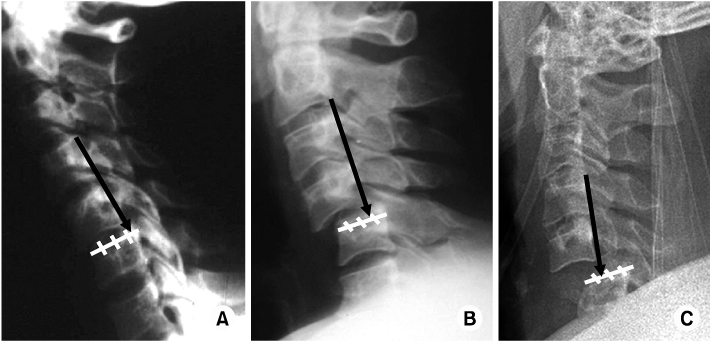
Article3. Allen BL Jr, Ferguson RL, Lehmann TR, O'Brien RP. A mechanistic classification of closed, indirect fractures and dislocations of the lower cervical spine. Spine (Phila Pa 1976). 1982. 7:1–27.
Article4. Argenson C, Lovet J, Sanouiller JL, de Peretti F. Traumatic rotatory displacement of the lower cervical spine. Spine (Phila Pa 1976). 1988. 13:767–773.
Article5. Bohlman HH. Acute fractures and dislocations of the cervical spine. An analysis of three hundred hospitalized patients and review of the literature. J Bone Joint Surg Am. 1979. 61:1119–1142.
Article6. Born JD, Albert A, Hans P, Bonnal J. Relative prognostic value of best motor response and brain stem reflexes in patients with severe head injury. Neurosurgery. 1985. 16:595–601.
Article7. Braakman R, Vinken PJ. Unilateral facet interlocking in the lower cervical spine. J Bone Joint Surg Br. 1967. 49:249–257.
Article8. Calenoff L, Chessare JW, Rogers LF, Toerge J, Rosen JS. Multiple level spinal injuries: importance of early recognition. AJR Am J Roentgenol. 1978. 130:665–669.
Article9. Chung JY, Heo JP, Yi KT. Anterior plate fixation of the cervical spine fractures in ankylosing spondylitis. J Korean Soc Spine Surg. 1997. 4:106–113.10. Clark CR, Wessels WE. Unilateral cervical facet fracture-dislocation. Surg Rounds Orthop. 1987. 45:15–19.11. Cybulski GR, Douglas RA, Meyer PR Jr, Rovin RA. Complications in three-column cervical spine injuries requiring anterior-posterior stabilization. Spine (Phila Pa 1976). 1992. 17:253–256.
Article12. de Oliveira JC. Anterior reduction of interlocking facets in the lower cervical spine. Spine (Phila Pa 1976). 1979. 4:195–202.
Article13. Denis F. The three column spine and its significance in the classification of acute thoracolumbar spinal injuries. Spine (Phila Pa 1976). 1983. 8:817–831.
Article14. Ducker TB, Bellegarrigue R, Salcman M, Walleck C. Timing of operative care in cervical spinal cord injury. Spine (Phila Pa 1976). 1984. 9:525–531.
Article15. Eismont FJ, Arena MJ, Green BA. Extrusion of an intervertebral disc associated with traumatic subluxation or dislocation of cervical facets. Case report. J Bone Joint Surg Am. 1991. 73:1555–1560.
Article16. Garfin SR, Botte MJ, Waters RL, Nickel VL. Complications in the use of the halo fixation device. J Bone Joint Surg Am. 1986. 68:320–325.
Article17. Harris WH, Hamblen DL, Ojemann RG. Traumatic disruption of cervical intervertebral disk from hyperextension injury. Clin Orthop Relat Res. 1968. 60:163–167.
Article18. Hwang BY, Song KJ, Ji JH. Disc extrusion on lower cervical facet joint fracture - dislocation. J Korean Orthop Assoc. 1997. 32:1078–1084.
Article19. Kornberg M. The computed tomographic appearance of a unilateral jumped cervical facet (the "false" facet joint sign). Spine (Phila Pa 1976). 1986. 11:1038–1040.
Article20. Kostuik JP. Indications for the use of the halo immobilization. Clin Orthop Relat Res. 1981. 154:46–50.
Article21. Maiman DJ, Barolat G, Larson SJ. Management of bilateral locked facets of the cervical spine. Neurosurgery. 1986. 18:542–547.
Article22. Marar BC. Hyperextension injuries of the cervical spine. The pathogenesis of damage to the spinal cord. J Bone Joint Surg Am. 1974. 56:1655–1662.23. Moon MS, Kim I, Kim OB. Anterior interbody fusion in unstable fracture and fracture-dislocation of the cervical spine. J Korean Orthop Assoc. 1981. 16:265–276.
Article24. Park HJ, Jeon JS, Lee PE. Range of motion of cervical spine in normal Korean people. J Korean Soc Spine Surg. 2004. 11:83–89.
Article25. Park HJ, Kim IG, Kim WK. Changes of adjacent segment in anterior cervical fusion. J Korean Soc Spine Surg. 2003. 10:269–276.
Article26. Plunkett PK, Redmond AD, Billsborough SH. Cervical subluxation: a deceptive soft tissue injury. J R Soc Med. 1987. 80:46–47.
Article27. Pratt ES, Green DA, Spengler DM. Herniated intervertebral discs associated with unstable spinal injuries. Spine (Phila Pa 1976). 1990. 15:662–666.
Article28. Richman JD, Daniel TE, Anderson DD, Miller PL, Douglas RA. Biomechanical evaluation of cervical spine stabilization methods using a porcine model. Spine (Phila Pa 1976). 1995. 20:2192–2197.
Article29. Rifkinson-Mann S, Mormino J, Sachdev VP. Subacute cervical spine instability. Surg Neurol. 1986. 26:413–416.
Article30. Rizzolo SJ, Piazza MR, Cotler JM, Balderston RA, Schaefer D, Flanders A. Intervertebral disc injury complicating cervical spine trauma. Spine (Phila Pa 1976). 1991. 16:6 Suppl. S187–S189.
Article31. Robertson PA, Ryan MD. Neurological deterioration after reduction of cervical subluxation. Mechanical compression by disc tissue. J Bone Joint Surg Br. 1992. 74:224–227.
Article32. Rorabeck CH, Rock MG, Hawkins RJ, Bourne RB. Unilateral facet dislocation of the cervical spine An analysis of the results of treatment in 26 patients. Spine (Phila Pa 1976). 1987. 12:23–27.33. Roy-Camille R, Saillant G, Mazel C. Internal fixation of the unstable cervical spine by a posterior osteosynthesis with plates and screws. The cervical spine. 1989. 2nd ed. Philadelphia: JB Lippincott;390–403.34. Song KJ, Lee KB. The prognosis of the acute cervical spinal cord injury. J Korean Orthop Assoc. 1998. 33:794–801.
Article35. Song KJ, Lee KR. The significance of space available for the spinal cord at the injured level in the lower cervical spine fractures and dislocations. J Korean Orthop Assoc. 1997. 32:1070–1077.
Article36. Song KJ, Shin PS. Surgical treatment of lower cervical spine injury. J Korean Orthop Assoc. 1999. 34:117–126.
Article37. Stauffer ES, Kelly EG. Fracture-dislocations of the cervical spine. Instability and recurrent deformity following treatment by anterior interbody fusion. J Bone Joint Surg Am. 1977. 59:45–48.
Article38. Vaccaro AR, Cook CM, McCullen G, Garfin SR. Cervical trauma: rationale for selecting the appropriate fusion technique. Orthop Clin North Am. 1998. 29:745–754.39. Webb JK, Broughton RB, McSweeney T, Park WM. Hidden flexion injury of the cervical spine. J Bone Joint Surg Br. 1976. 58:322–327.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pattern of Cervical Spine Injury in Patients with a Facial Fracture
- Missed Traumatic Cervical Spine Injury
- Posterior Cervical Plate Fixation in Cervical Injuries
- Clinical Analysis of Lower Cervical Spine-Injuried Patients
- Delayed or Missed Diagnosis of Cervical Instability after Traumatic Injury: Usefulness of Dynamic Flexion and Extension Radiographs