J Korean Neurosurg Soc.
2012 Feb;51(2):75-80. 10.3340/jkns.2012.51.2.75.
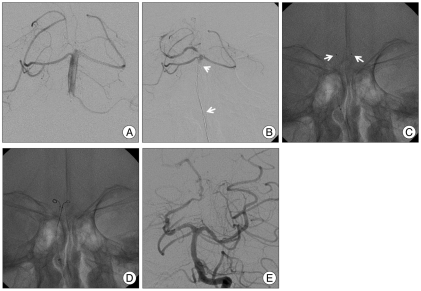
Intra-Arterial Thrombolysis Using Double Devices: Mechanicomechanical or Chemicomechanical Techniques
- Affiliations
-
- 1Department of Neurosurgery, Jeju National University Hospital, Jeju National University School of Medicine, Jeju, Korea.
- 2Department of Neurosurgery, Chuncheon Sacred Heart Hospital, Hallym University and Graduate School of Kangwon University, Chuncheon, Korea.
- 3Department of Neurosurgery, Cerebrovascular Center, Inje University College of Medicine, Haeundae Paik Hospital, Busan, Korea.
- 4Department of Neurosurgery, Seoul National University Bundang Hospital, Seongnam, Korea. kwonoki@snubh.org
- KMID: 1441413
- DOI: http://doi.org/10.3340/jkns.2012.51.2.75
Abstract
OBJECTIVE
To optimize the recanalization of acute cerebral stroke that were not effectively resolved by conventional intraarterial thrombolysis (IAT), we designed a double device technique to allow for rapid and effective reopening. In this article, we describe the feasibility and efficacy of this technique.
METHODS
From January 2008 to September 2009, twenty patients with acute cerebral arterial occlusion (middle cerebral artery : n=12; internal carotid artery terminus : n=5; basilar artery : n=3) were treated by the double device technique. This technique was applied when conventional thrombolytic methods using drug, microwires, microcatheters and balloons did not result in recanalization. In the double device technique, two devices are simultaneously placed at the lesion (for example, one microcatheter and one balloon or two microcatheters). Chemicomechanical or mechanicomechanical thrombolysis was performed simultaneously using various combinations of two devices. Recanalization rates, procedural time, complications, and clinical outcomes were analyzed.
RESULTS
The initial median National Institute of Health Stroke Scale (NIHSS) was 16 (range 5-26). The double device technique was applied after conventional IAT methods failed. Recanalization was achieved in 18 patients (90%). Among them, 55% (11 cases) were complete (thrombolysis in cerebral infarction 2B, 3). The median thrombolytic procedural time including the conventional technique was 135+/-83.7 minutes (range 75-427). Major symptomatic hemorrhages (neurological deterioration > or =4 points in NIHSS) developed in two patients (10%). Good long term outcomes (modified Rankin Scale < or =2 at 90 days) occurred in 25% (n=5) of the cases. Mortality within 90 days developed in two cases (10%).
CONCLUSION
The double device technique is a feasible and effective technical option for large vessel occlusion refractory to conventional thrombolysis.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
Improper Use of Thrombolytic Agents in Acute Hemiparesis Following Misdiagnosis of Acute Ischemic Stroke
Min Chan Kim, Seok Won Kim
Korean J Neurotrauma. 2018;14(1):20-23. doi: 10.13004/kjnt.2018.14.1.20.Inadvertent Self-Detachment of Solitaire AB Stent during the Mechanical Thrombectomy for Recanalization of Acute Ischemic Stroke: Lessons Learned from the Removal of Stent via Surgical Embolectomy
Dong-Hun Kang, Jaechan Park, Yang-Ha Hwang, Yong-Sun Kim
J Korean Neurosurg Soc. 2013;53(6):360-363. doi: 10.3340/jkns.2013.53.6.360.
Reference
-
1. Abou-Chebl A, Bajzer CT, Krieger DW, Furlan AJ, Yadav JS. Multimodal therapy for the treatment of severe ischemic stroke combining GPIIb/IIIa antagonists and angioplasty after failure of thrombolysis. Stroke. 2005; 36:2286–2288. PMID: 16179581.
Article2. Arnold M, Nedeltchev K, Mattle HP, Loher TJ, Stepper F, Schroth G, et al. Intra-arterial thrombolysis in 24 consecutive patients with internal carotid artery T occlusions. J Neurol Neurosurg Psychiatry. 2003; 74:739–742. PMID: 12754342.
Article3. Bose A, Henkes H, Alfke K, Reith W, Mayer TE, Berlis A, et al. The Penumbra System: a mechanical device for the treatment of acute stroke due to thromboembolism. AJNR Am J Neuroradiol. 2008; 29:1409–1413. PMID: 18499798.
Article4. Furlan A, Higashida R, Wechsler L, Gent M, Rowley H, Kase C, et al. Prolyse in Acute Cerebral Thromboembolism. Intra-arterial prourokinase for acute ischemic stroke. The PROACT II study: a randomized controlled trial. JAMA. 1999; 282:2003–2011. PMID: 10591382.
Article5. Higashida RT, Furlan AJ, Roberts H, Tomsick T, Connors B, Barr J, et al. Trial design and reporting standards for intra-arterial cerebral thrombolysis for acute ischemic stroke. Stroke. 2003; 34:e109–e137. PMID: 12869717.
Article6. Kim DJ, Kim DI, Byun JS, Jung JY, Suh SH, Kim EY, et al. Simple microwire and microcatheter mechanical thrombolysis with adjuvant intraarterial urokinase for treatment of hyperacute ischemic stroke patients. Acta Radiol. 2008; 49:351–357. PMID: 18365826.
Article7. Levy EI, Mehta R, Gupta R, Hanel RA, Chamczuk AJ, Fiorella D, et al. Self-expanding stents for recanalization of acute cerebrovascular occlusions. AJNR Am J Neuroradiol. 2007; 28:816–822. PMID: 17494649.8. Lin R, Vora N, Zaidi S, Aleu A, Jankowitz B, Thomas A, et al. Mechanical approaches combined with intra-arterial pharmacological therapy are associated with higher recanalization rates than either intervention alone in revascularization of acute carotid terminus occlusion. Stroke. 2009; 40:2092–2097. PMID: 19390066.
Article9. Linfante I, Llinas RH, Selim M, Chaves C, Kumar S, Parker RA, et al. Clinical and vascular outcome in internal carotid artery versus middle cerebral artery occlusions after intravenous tissue plasminogen activator. Stroke. 2002; 33:2066–2071. PMID: 12154264.
Article10. Nakano S, Iseda T, Yoneyama T, Kawano H, Wakisaka S. Direct percutaneous transluminal angioplasty for acute middle cerebral artery trunk occlusion : an alternative option to intra-arterial thrombolysis. Stroke. 2002; 33:2872–2876. PMID: 12468784.
Article11. Nogueira RG, Schwamm LH, Buonanno FS, Koroshetz WJ, Yoo AJ, Rabinov JD, et al. Low-pressure balloon angioplasty with adjuvant pharmacological therapy in patients with acute ischemic stroke caused by intracranial arterial occlusions. Neuroradiology. 2008; 50:331–340. PMID: 18172631.
Article12. Qureshi AI, Siddiqui AM, Suri MF, Kim SH, Ali Z, Yahia AM, et al. Aggressive mechanical clot disruption and low-dose intra-arterial third-generation thrombolytic agent for ischemic stroke: a prospective study. Neurosurgery. 2002; 51:1319–1327. discussion 1327-1329. PMID: 12383381.
Article13. Smith WS, Sung G, Saver J, Budzik R, Duckwiler G, Liebeskind DS, et al. Mechanical thrombectomy for acute ischemic stroke : final results of the Multi MERCI trial. Stroke. 2008; 39:1205–1212. PMID: 18309168.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Evolution of Endovascular Therapy in Acute Stroke: Implications of Device Development
- The Effect of Intra-arterial Thrombolysis in Retinal Artery Occlusion: Case Series and Literature Review
- Intra-Arterial Thrombolysis for Deep Vein Thrombosis of the Lower Extremity: Case Report
- Intra-arterial Thrombolysis for Central Retinal Artery Occlusion after the Coil Embolization of Paraclinoid Aneurysm
- Recent advances in thrombolysis of acute ischemic stroke