J Korean Soc Hypertens.
2012 Jun;18(2):53-62. 10.5646/jksh.2012.18.2.53.
Salt, Hypertension, and Cardiovascular Diseases
- Affiliations
-
- 1Division of Hypertension and Nephrology, National Cerebral and Cardiovascular Center, Suita, Osaka, Japan. kawano.yuhei.hp@mail.ncvc.go.jp
- KMID: 1436341
- DOI: http://doi.org/10.5646/jksh.2012.18.2.53
Abstract
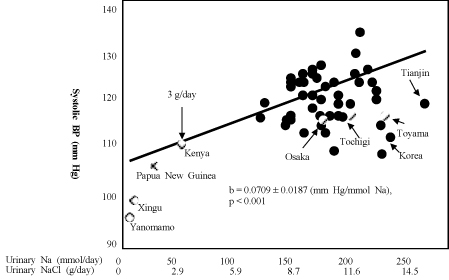
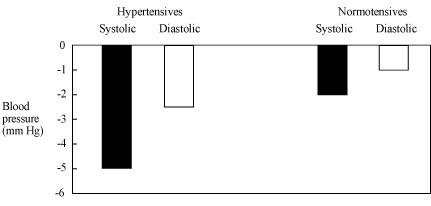
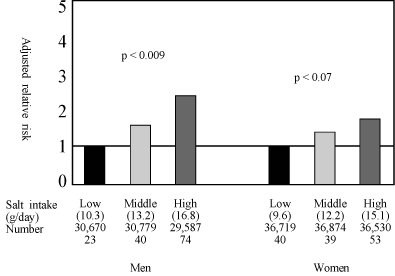
- The relationship between salt and hypertension is well established, and salt restriction is widely recommended in the management of hypertension. However, people living in northeast Asia have consumed large amount of salt, and the prevalence of hypertension and the incidence of stroke have been high in that area. Mechanisms of salt-induced hypertension may be complex, but volume expansion in the presence of impaired natriuretic capacity of the kidney and action on the central nervous system and neurohormoral pathways seem to be important. Salt is also involved in changes in blood pressure (BP) caused by other factors, such as weight gain, stress, exercise, potassium, catecholamines, angiotensin, and aldosterone. The interaction between sodium and aldosterone appears to play a critical role in the development of organ damage. The depressor effect of salt restriction in hypertensive patients is well demonstrated although the response of BP varies widely among individuals. Salt restriction decreases BP throughout 24 hours, and its effect may be greater during night compared to daytime in salt-sensitive nondippers. Although excess salt consumption can cause cardiovascular diseases through its effect on BP, recent studied have shown that the association of salt consumption and cardiovascular diseases, such as stroke and heart failure, is independent of BP. Salt reduction is important in the prevention of cardiovascular diseases, however, the effect and safety of aggressive salt restriction remain to be clarified. It is difficult to accomplish and maintain the salt reduction. Both population strategy and individualized approach are important to reduce salt consumption.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Operation and Process Evaluation of a Community Meal Program for the Elderly in Rural Areas during Agricultural Off-Season Perceived by Cooking Volunteers
Jeong-Sook Bae, Sol-Bee Seong, So-Mang Jang, Chang-Hee Yoo, Young-Suk Lim, Young-Mi Lee, Hae-Ryun Park, Kyung-Eun Lee
Korean J Community Nutr. 2019;24(4):277-289. doi: 10.5720/kjcn.2019.24.4.277.
Reference
-
1. Hamlyn JM, Blaustein MP. Sodium chloride, extracellular fluid volume, and blood pressure regulation. Am J Physiol. 1986. 251(4 Pt 2):F563–F575.
Article2. Folkow B, Ely DL. Dietary sodium effects on cardiovascular and sympathetic neuroeffector functions as studied in various rat models. J Hypertens. 1987. 5:383–395.
Article3. Adrogue HJ, Madias NE. Sodium and potassium in the pathogenesis of hypertension. N Engl J Med. 2007. 356:1966–1978.
Article4. Mancia G, De Backer G, Dominiczak A, Cifkova R, Fagard R, Germano G, et al. 2007 Guidelines for the Management of Arterial Hypertension: The Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens. 2007. 25:1105–1187.5. Ogihara T, Kikuchi K, Matsuoka H, Fujita T, Higaki J, Horiuchi M, et al. The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2009). Hypertens Res. 2009. 32:3–107.6. Intersalt Cooperative Research Group. Intersalt: an international study of electrolyte excretion and blood pressure. Results for 24 hour urinary sodium and potassium excretion. BMJ. 1988. 297:319–328.7. Zhou BF, Stamler J, Dennis B, Moag-Stahlberg A, Okuda N, Robertson C, et al. Nutrient intakes of middle-aged men and women in China, Japan, United Kingdom, and United States in the late 1990s: the INTERMAP study. J Hum Hypertens. 2003. 17:623–630.
Article8. He FJ, MacGregor GA. Effect of modest salt reduction on blood pressure: a meta-analysis of randomized trials: implications for public health. J Hum Hypertens. 2002. 16:761–770.
Article9. Kawano Y, Ando K, Matsuura H, Tsuchihashi T, Fujita T, Ueshima H, et al. Report of the Working Group for Dietary Salt Reduction of the Japanese Society of Hypertension: (1) Rationale for salt restriction and salt-restriction target level for the management of hypertension. Hypertens Res. 2007. 30:879–886.
Article10. Ohta Y, Tsuchihashi T, Ueno M, Kajioka T, Onaka U, Tominaga M, et al. Relationship between the awareness of salt restriction and the actual salt intake in hypertensive patients. Hypertens Res. 2004. 27:243–246.
Article11. Strazzullo P, D'Elia L, Kandala NB, Cappuccio FP. Salt intake, stroke, and cardiovascular disease: meta-analysis of prospective studies. BMJ. 2009. 339:b4567.
Article12. He FJ, MacGregor GA. A comprehensive review on salt and health and current experience of worldwide salt reduction programmes. J Hum Hypertens. 2009. 23:363–384.
Article13. Cook NR, Cutler JA, Obarzanek E, Buring JE, Rexrode KM, Kumanyika SK, et al. Long term effects of dietary sodium reduction on cardiovascular disease outcomes: observational follow-up of the trials of hypertension prevention (TOHP). BMJ. 2007. 334:885–888.
Article14. Bibbins-Domingo K, Chertow GM, Coxson PG, Moran A, Lightwood JM, Pletcher MJ, et al. Projected effect of dietary salt reductions on future cardiovascular disease. N Engl J Med. 2010. 362:590–599.
Article15. Alderman MH, Cohen H, Madhavan S. Dietary sodium intake and mortality: the National Health and Nutrition Examination Survey (NHANES I). Lancet. 1998. 351:781–785.
Article16. Stolarz-Skrzypek K, Kuznetsova T, Thijs L, Tikhonoff V, Seidlerova J, Richart T, et al. Fatal and nonfatal outcomes, incidence of hypertension, and blood pressure changes in relation to urinary sodium excretion. JAMA. 2011. 305:1777–1785.
Article17. Kawasaki T, Delea CS, Bartter FC, Smith H. The effect of high-sodium and low-sodium intakes on blood pressure and other related variables in human subjects with idiopathic hypertension. Am J Med. 1978. 64:193–198.
Article18. Anderson CA, Appel LJ, Okuda N, Brown IJ, Chan Q, Zhao L, et al. Dietary sources of sodium in China, Japan, the United Kingdom, and the United States, women and men aged 40 to 59 years: the INTERMAP study. J Am Diet Assoc. 2010. 110:736–745.
Article19. Ministry of Health, Labor, and Welfare. Summary of the national survey of health and nutrition in 2010 [Internet]. 2012. cited 2012 Jun 4. Tokyo: Ministry of Health, Labor, and Welfare;Available from: http://www.mhlw.go.jp/stf/houdou/2r98520000020qbb-att/2r98520000021c0o.pdf.20. Tanaka T, Okamura T, Miura K, Kadowaki T, Ueshima H, Nakagawa H, et al. A simple method to estimate populational 24-h urinary sodium and potassium excretion using a casual urine specimen. J Hum Hypertens. 2002. 16:97–103.
Article21. Kawano Y, Tsuchihashi T, Matsuura H, Ando K, Fujita T, Ueshima H, et al. Report of the Working Group for Dietary Salt Reduction of the Japanese Society of Hypertension: (2) Assessment of salt intake in the management of hypertension. Hypertens Res. 2007. 30:887–893.
Article22. Guyton AC. Arterial pressure and hypertension. Circulatory physiology, 3. 1980. Philadelphia: Saunders.23. Kawano Y, Ferrario CM. Neurohormonal characteristics of cardiovascular response due to intraventricular hypertonic NaCl. Am J Physiol. 1984. 247(3 Pt 2):H422–H428.
Article24. Kawano Y, Sudo RT, Ferrario CM. Effects of chronic intraventricular sodium on blood pressure and fluid balance. Hypertension. 1991. 17:28–35.
Article25. de Wardener HE, MacGregor GA. Dahl's hypothesis that a salureic substance may be responsible for a sustained rise in arterial pressure: its possible role in essential hypertension. Kidney Int. 1980. 18:1–9.26. Kawano Y, Yoshida K, Kawamura M, Yoshimi H, Ashida T, Abe H, et al. Sodium and noradrenaline in cerebrospinal fluid and blood in salt-sensitive and non-salt-sensitive essential hypertension. Clin Exp Pharmacol Physiol. 1992. 19:235–241.
Article27. Hall JE. Control of sodium excretion by angiotensin II: intrarenal mechanisms and blood pressure regulation. Am J Physiol. 1986. 250(6 Pt 2):R960–R972.
Article28. Briet M, Schiffrin EL. Aldosterone: effects on the kidney and cardiovascular system. Nat Rev Nephrol. 2010. 6:261–273.
Article29. DiBona GF. Sympathetic nervous system influences on the kidney: role in hypertension. Am J Hypertens. 1989. 2(3 Pt 2):119S–124S.30. Hall JE. The kidney, hypertension, and obesity. Hypertension. 2003. 41(3 Pt 2):625–633.
Article31. Arakawa K. Antihypertensive mechanism of exercise. J Hypertens. 1993. 11:223–229.
Article32. Fujita T, Sato Y. Natriuretic and antihypertensive effects of potassium in DOCA-salt hypertensive rats. Kidney Int. 1983. 24:731–739.
Article33. Luft FC. Putative mechanism of blood pressure reduction induced by increases in dietary calcium intake. Am J Hypertens. 1990. 3(8 Pt 2):156S–160S.
Article34. Weinberger MH. Sodium sensitivity of blood pressure. Curr Opin Nephrol Hypertens. 1993. 2:935–939.
Article35. Yamagishi K, Tanigawa T, Cui R, Tabata M, Ikeda A, Yao M, et al. High sodium intake strengthens the association of ACE I/D polymorphism with blood pressure in a community. Am J Hypertens. 2007. 20:751–757.
Article36. Gu D, Kelly TN, Hixson JE, Chen J, Liu D, Chen JC, et al. Genetic variants in the renin-angiotensin-aldosterone system and salt sensitivity of blood pressure. J Hypertens. 2010. 28:1210–1220.
Article37. Iwai N, Kajimoto K, Tomoike H, Takashima N. Polymorphism of CYP11B2 determines salt sensitivity in Japanese. Hypertension. 2007. 49:825–831.38. Eap CB, Bochud M, Elston RC, Bovet P, Maillard MP, Nussberger J, et al. CYP3A5 and ABCB1 genes influence blood pressure and response to treatment, and their effect is modified by salt. Hypertension. 2007. 49:1007–1014.39. Kawano Y, Abe H, Kojima S, Yoshimi H, Sanai T, Kimura G, et al. Different effects of alcohol and salt on 24-hour blood pressure and heart rate in hypertensive patients. Hypertens Res. 1996. 19:255–261.
Article40. Uzu T, Ishikawa K, Fujii T, Nakamura S, Inenaga T, Kimura G. Sodium restriction shifts circadian rhythm of blood pressure from nondipper to dipper in essential hypertension. Circulation. 1997. 96:1859–1862.
Article41. Verdecchia P, Porcellati C, Schillaci G, Borgioni C, Ciucci A, Battistelli M, et al. Ambulatory blood pressure: an independent predictor of prognosis in essential hypertension. Hypertension. 1994. 24:793–801.
Article42. Slagman MC, Waanders F, Hemmelder MH, Woittiez AJ, Janssen WM, Lambers Heerspink HJ, et al. Moderate dietary sodium restriction added to angiotensin converting enzyme inhibition compared with dual blockade in lowering proteinuria and blood pressure: randomised controlled trial. BMJ. 2011. 343:d4366.
Article43. Pimenta E, Gaddam KK, Oparil S, Aban I, Husain S, Dell'Italia LJ, et al. Effects of dietary sodium reduction on blood pressure in subjects with resistant hypertension: results from a randomized trial. Hypertension. 2009. 54:475–481.44. du Cailar G, Ribstein J, Mimran A. Dietary sodium and target organ damage in essential hypertension. Am J Hypertens. 2002. 15:222–229.
Article45. Jin Y, Kuznetsova T, Maillard M, Richart T, Thijs L, Bochud M, et al. Independent relations of left ventricular structure with the 24-hour urinary excretion of sodium and aldosterone. Hypertension. 2009. 54:489–495.
Article46. Ahn J, Varagic J, Slama M, Susic D, Frohlich ED. Cardiac structural and functional responses to salt loading in SHR. Am J Physiol Heart Circ Physiol. 2004. 287:H767–H772.
Article47. Bragulat E, de la Sierra A, Antonio MT, Jimenez W, Urbano-Marquez A, Coca A. Effect of salt intake on endothelium-derived factors in a group of patients with essential hypertension. Clin Sci (Lond). 2001. 101:73–78.
Article48. Dickinson KM, Clifton PM, Keogh JB. Endothelial function is impaired after a high-salt meal in healthy subjects. Am J Clin Nutr. 2011. 93:500–505.
Article49. Sanders PW. Salt intake, endothelial cell signaling, and progression of kidney disease. Hypertension. 2004. 43:142–146.
Article50. Njoroge JN, El Khoudary SR, Fried LF, Barinas-Mitchell E, Sutton-Tyrrell K. High urinary sodium is associated with increased carotid intima-media thickness in normotensive overweight and obese adults. Am J Hypertens. 2011. 24:70–76.
Article51. Park S, Park JB, Lakatta EG. Association of central hemodynamics with estimated 24-h urinary sodium in patients with hypertension. J Hypertens. 2011. 29:1502–1507.
Article52. Blasi ER, Rocha R, Rudolph AE, Blomme EA, Polly ML, McMahon EG. Aldosterone/salt induces renal inflammation and fibrosis in hypertensive rats. Kidney Int. 2003. 63:1791–1800.
Article53. Takeda Y, Yoneda T, Demura M, Furukawa K, Miyamori I, Mabuchi H. Effects of high sodium intake on cardiovascular aldosterone synthesis in stroke-prone spontaneously hypertensive rats. J Hypertens. 2001. 19(3 Pt 2):635–639.
Article54. Tuomilehto J, Jousilahti P, Rastenyte D, Moltchanov V, Tanskanen A, Pietinen P, et al. Urinary sodium excretion and cardiovascular mortality in Finland: a prospective study. Lancet. 2001. 357:848–851.
Article55. He J, Ogden LG, Bazzano LA, Vupputuri S, Loria C, Whelton PK. Dietary sodium intake and incidence of congestive heart failure in overweight US men and women: first National Health and Nutrition Examination Survey Epidemiologic Follow-up Study. Arch Intern Med. 2002. 162:1619–1624.56. Nagata C, Takatsuka N, Shimizu N, Shimizu H. Sodium intake and risk of death from stroke in Japanese men and women. Stroke. 2004. 35:1543–1547.
Article57. Alderman MH, Madhavan S, Cohen H, Sealey JE, Laragh JH. Low urinary sodium is associated with greater risk of myocardial infarction among treated hypertensive men. Hypertension. 1995. 25:1144–1152.
Article58. O'Donnell MJ, Yusuf S, Mente A, Gao P, Mann JF, Teo K, et al. Urinary sodium and potassium excretion and risk of cardiovascular events. JAMA. 2011. 306:2229–2238.59. Taylor RS, Ashton KE, Moxham T, Hooper L, Ebrahim S. Reduced dietary salt for the prevention of cardiovascular disease: a meta-analysis of randomized controlled trials (Cochrane review). Am J Hypertens. 2011. 24:843–853.
Article60. He FJ, MacGregor GA. Salt reduction lowers cardiovascular risk: meta-analysis of outcome trials. Lancet. 2011. 378:380–382.
Article61. He FJ, Jenner KH, Macgregor GA. WASH-world action on salt and health. Kidney Int. 2010. 78:745–753.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Barriers in Salt Reduction Strategies: Time to Acting for the Future
- Dietary Salt Intake and Hypertension
- Self-monitoring urinary salt excretion device can be used for controlling hypertension for developing countries
- Altered Vascular Expression of Nitric Oxide Synthase Isozymes in Hypertension
- Salt Sensitivity and Hypertension: A Paradigm Shift from Kidney Malfunction to Vascular Endothelial Dysfunction