Korean J Orthod.
2012 Aug;42(4):190-200. 10.4041/kjod.2012.42.4.190.
Relationship between Class III malocclusion and hyoid bone displacement during swallowing: a cine-magnetic resonance imaging study
- Affiliations
-
- 1Department of Orthodontics, Dental Science Center, Gulhane Military Medical Academy, Ankara, Turkey. silagokce@yahoo.com
- 2Dental Service, Beytepe Military Hospital, Beytepe, Ankara, Turkey.
- 3Department of Orthodontics, Haydarpasa Training Center, Gulhane Military Medical Academy, Istanbul, Turkey.
- 4Dental Service, Golcuk Military Hospital, Golcuk, Kocaeli, Turkey.
- KMID: 1435413
- DOI: http://doi.org/10.4041/kjod.2012.42.4.190
Abstract
OBJECTIVE
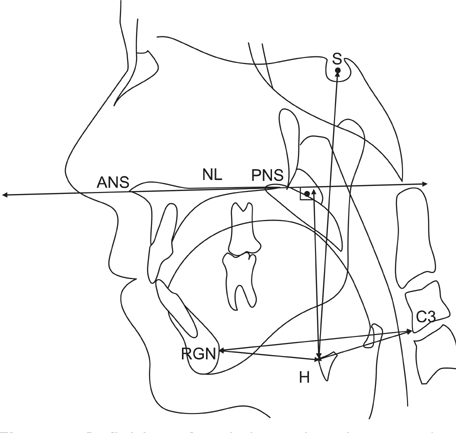
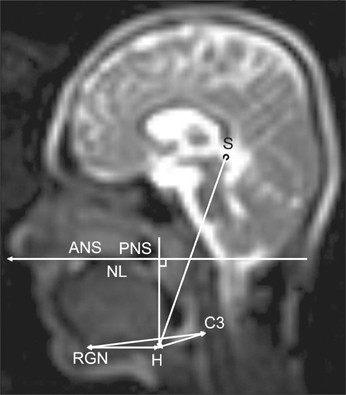
The displacement of the hyoid bone (HB) is a critical biomechanical component of the swallowing function. The aim of this study was to evaluate the swallowing-induced vertical and horizontal displacements of the HB in subjects with 2 different magnitudes of skeletal Class III malocclusion, by means of real-time, balanced turbo-field-echo (B-TFE) cine-magnetic resonance imaging.
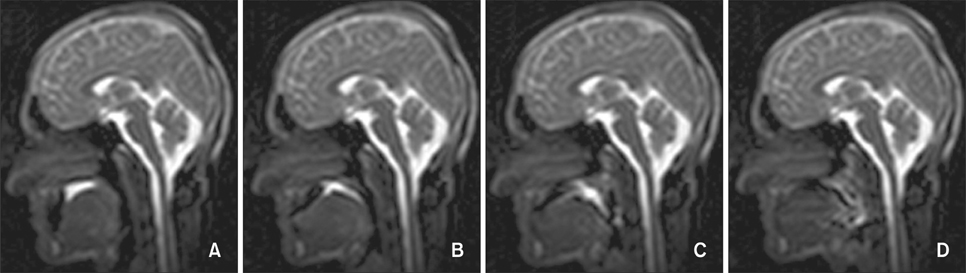
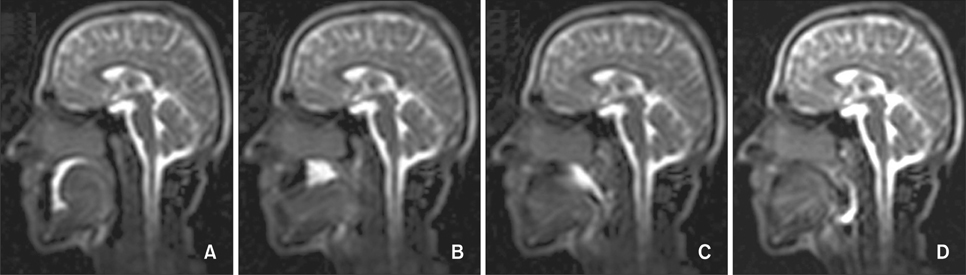
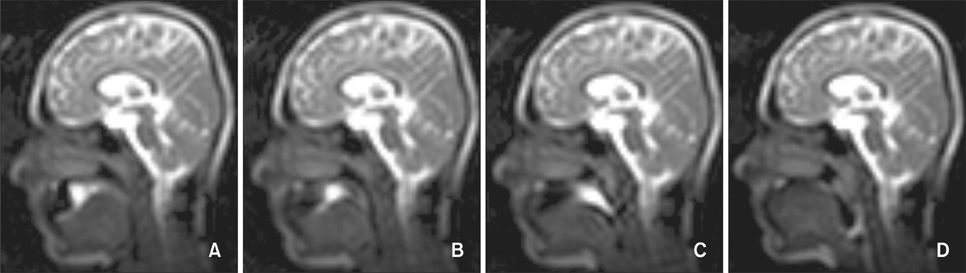
METHODS
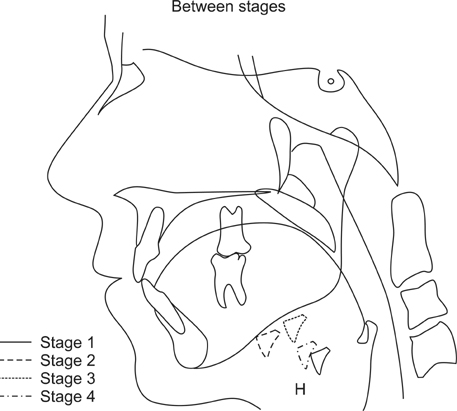
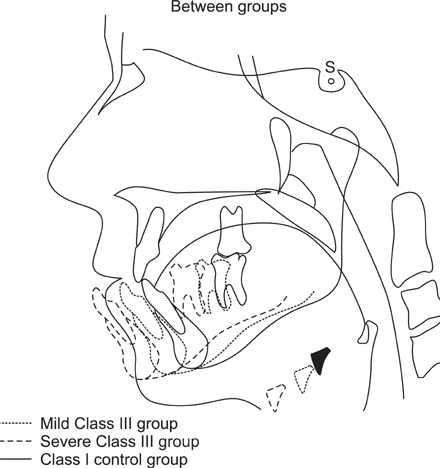
The study population comprised 19 patients with mild skeletal Class III malocclusion, 16 with severe skeletal Class III malocclusion, and 20 with a skeletal Class I relationship. Before the commencement of the study, all subjects underwent cephalometric analysis to identify the nature of skeletal malformations. B-TFE images were obtained for the 4 consecutive stages of deglutition as each patient swallowed 10 mL of water, and the vertical and horizontal displacements of the HB were measured at each stage.
RESULTS
At all stages of swallowing, the vertical position of the HB in the severe Class III malocclusion group was significantly lower than those in the mild Class III and Class I malocclusion groups. Similarly, the horizontal displacement of the HB was found to be significantly associated with the severity of malocclusion, i.e., the degree of Class III malocclusion, while the amount of anterior displacement of the HB decreased with an increase in the severity of the Class III deformity.
CONCLUSIONS
Our findings indicate the existence of a relationship between the magnitude of Class III malocclusion and HB displacement during swallowing.
MeSH Terms
Figure
Reference
-
1. Anagnostara A, Stoeckli S, Weber OM, Kollias SS. Evaluation of the anatomical and functional properties of deglutition with various kinetic high-speed MRI sequences. J Magn Reson Imaging. 2001. 14:194–199.
Article2. Hartl DM, Albiter M, Kolb F, Luboinski B, Sigal R. Morphologic parameters of normal swallowing events using single-shot fast spin echo dynamic MRI. Dysphagia. 2003. 18:255–262.
Article3. Kim Y, McCullough GH. Maximum hyoid displacement in normal swallowing. Dysphagia. 2008. 23:274–279.
Article4. Robbins J, Hamilton JW, Lof GL, Kempster GB. Oropharyngeal swallowing in normal adults of different ages. Gastroenterology. 1992. 103:823–829.
Article5. Lundy DS, Smith C, Colangelo L, Sullivan PA, Logemann JA, Lazarus CL, et al. Aspiration: cause and implications. Otolaryngol Head Neck Surg. 1999. 120:474–478.
Article6. Humbert IA, Poletto CJ, Saxon KG, Kearney PR, Crujido L, Wright-Harp W, et al. The effect of surface electrical stimulation on hyolaryngeal movement in normal individuals at rest and during swallowing. J Appl Physiol. 2006. 101:1657–1663.
Article7. Mays KA, Palmer JB, Kuhlemeier KV. Influence of craniofacial morphology on hyoid movement: a preliminary correlational study. Dysphagia. 2009. 24:71–76.
Article8. Sivarao DV, Goyal RK. Functional anatomy and physiology of the upper esophageal sphincter. Am J Med. 2000. 108:Suppl 4a. 27S–37S.
Article9. Yamaoka M, Furusawa K, Uematsu T, Okafuji N, Kayamoto D, Kurihara S. Relationship of the hyoid bone and posterior surface of the tongue in prognathism and micrognathia. J Oral Rehabil. 2003. 30:914–920.
Article10. Logemann JA, Pauloski BR, Rademaker AW, Kahrilas PJ. Oropharyngeal swallow in younger and older women: videofluoroscopic analysis. J Speech Lang Hear Res. 2002. 45:434–445.11. Gay T, Rendell JK, Spiro J, Mosier K, Lurie AG. Coordination of oral cavity and laryngeal movements during swallowing. J Appl Physiol. 1994. 77:357–365.
Article12. Haralabakis NB, Toutountzakis NM, Yiagtzis SC. The hyoid bone position in adult individuals with open bite and normal occlusion. Eur J Orthod. 1993. 15:265–271.
Article13. Cook IJ, Dodds WJ, Dantas RO, Massey B, Kern MK, Lang IM, et al. Opening mechanisms of the human upper esophageal sphincter. Am J Physiol. 1989. 257:G748–G759.
Article14. Dodds WJ, Man KM, Cook IJ, Kahrilas PJ, Stewart ET, Kern MK. Influence of bolus volume on swallow-induced hyoid movement in normal subjects. AJR Am J Roentgenol. 1988. 150:1307–1309.
Article15. Perlman AL, VanDaele DJ, Otterbacher MS. Quantitative assessment of hyoid bone displacement from video images during swallowing. J Speech Hear Res. 1995. 38:579–585.
Article16. Ishida R, Palmer JB, Hiiemae KM. Hyoid motion during swallowing: factors affecting forward and upward displacement. Dysphagia. 2002. 17:262–272.
Article17. Paik NJ, Kim SJ, Lee HJ, Jeon JY, Lim JY, Han TR. Movement of the hyoid bone and the epiglottis during swallowing in patients with dysphagia from different etiologies. J Electromyogr Kinesiol. 2008. 18:329–335.
Article18. Zhou Y, Fu M, Wang C. Swallowing pattern in skeletal Class III malocclusion. Zhonghua Kou Qiang Yi Xue Za Zhi. 1995. 30:355–358.19. Cheng CF, Peng CL, Chiou HY, Tsai CY. Dentofacial morphology and tongue function during swallowing. Am J Orthod Dentofacial Orthop. 2002. 122:491–499.
Article20. Cuozzo GS, Bowman DC. Hyoid positioning during deglutition following forced positioning of the tongue. Am J Orthod. 1975. 68:564–570.
Article21. Fujiki T, Inoue M, Miyawaki S, Nagasaki T, Tanimoto K, Takano-Yamamoto T. Relationship between maxillofacial morphology and deglutitive tongue movement in patients with anterior open bite. Am J Orthod Dentofacial Orthop. 2004. 125:160–167.
Article22. Gilbert RJ, Reese TG, Daftary SJ, Smith RN, Weisskoff RM, Wedeen VJ. Determination of lingual myoarchitecture in whole tissue by NMR imaging of anisotropic water diffusion. Am J Physiol. 1998. 275:G363–G369.23. Honda Y, Hata N. Dynamic imaging of swallowing in a seated position using open-configuration MRI. J Magn Reson Imaging. 2007. 26:172–176.
Article24. Karaçay S, Akin E, Sayin MO, Bulakbaşi N. Real time balanced turbo field echo Cine-MRI in the analysis of deglutition events and transit times. J Oral Rehabil. 2006. 33:646–653.
Article25. Hiiemae KM, Palmer JB. Tongue movements in feeding and speech. Crit Rev Oral Biol Med. 2003. 14:413–429.
Article26. Monaco A, Cattaneo R, Spadaro A, Giannoni M. Surface electromyography pattern of human swallowing. BMC Oral Health. 2008. 8:6.
Article27. Mehnert J, Landau H, Mussler A, Reinicke J, Müller-Hartwich R, Orawa H, et al. Comparison between logopedic and MRI findings in evaluating tongue function. J Orofac Orthop. 2009. 70:455–467.
Article28. Panebianco V, Ruoppolo G, Pelle G, Schettino I, Roma R, Bernardo S, et al. Morpho-functional patterns of physiologic oropharyngeal swallowing evaluated with dynamic fast MRI. Eur Arch Otorhinolaryngol. 2010. 267:1461–1466.
Article29. Alves PV, Zhao L, O'Gara M, Patel PK, Bolognese AM. Three-dimensional cephalometric study of upper airway space in skeletal class II and III healthy patients. J Craniofac Surg. 2008. 19:1497–1507.
Article30. Pracharktam N, Nelson S, Hans MG, Broadbent BH, Redline S, Rosenberg C, et al. Cephalometric assessment in obstructive sleep apnea. Am J Orthod Dentofacial Orthop. 1996. 109:410–419.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A study on positional change of the hyoid bone before and after activator therapy in angle's Class III malocclusion patients
- A cinefluoroscopic study of oropharyngeal movement of the Class III malocclusion patients during swallowing
- Evaluation of hyoid bone position and airway size in Class III malocclusion
- A study on the changes of pharyngeal airway, hyoid bone and head posture before and after tonsillectomy in functional Class III malocclusion patients
- A cephalometric study on the airway size according to the types of the malocclusion