J Korean Assoc Oral Maxillofac Surg.
2012 Feb;38(1):55-63. 10.5125/jkaoms.2012.38.1.55.
Clinical study of keratocystic odontogenic tumors
- Affiliations
-
- 1Maxillofacial Surgery, Maxillofacial Reconstruction and Function, Division of Maxillofacial and Neck Reconstruction, Graduate School, Tokyo Medical and Dental University, Japan. tomomatsu.mfs@tmd.ac.jp
- 2Diagnostic Oral Pathology, Oral Restitution, Oral Health Sciences, Graduate School, Tokyo Medical and Dental University, Japan.
- KMID: 1434380
- DOI: http://doi.org/10.5125/jkaoms.2012.38.1.55
Abstract
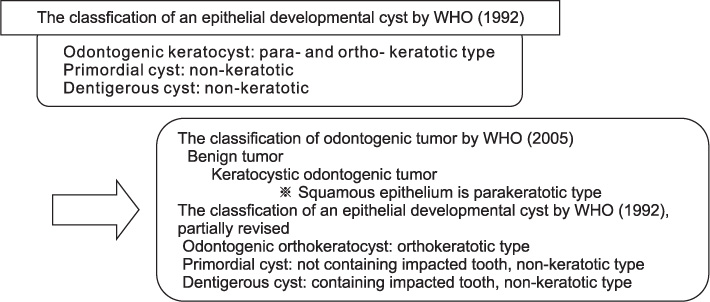
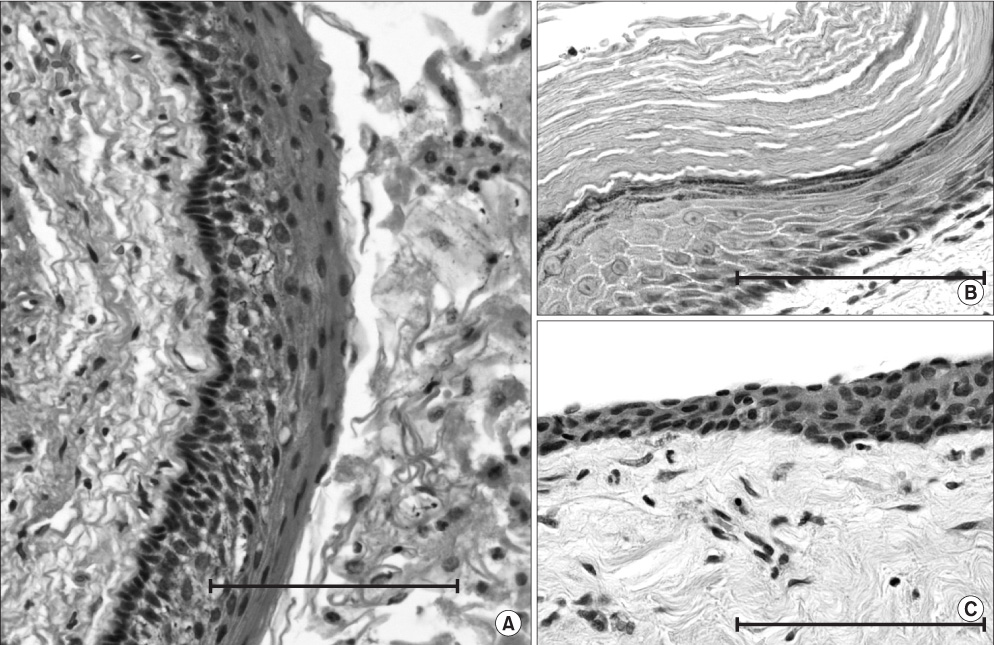
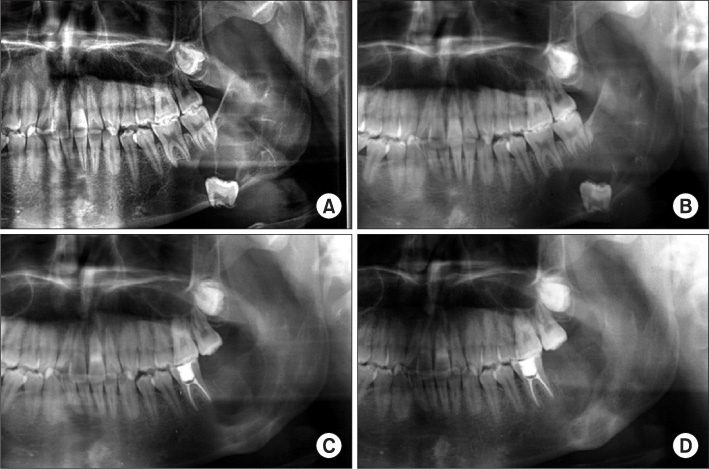
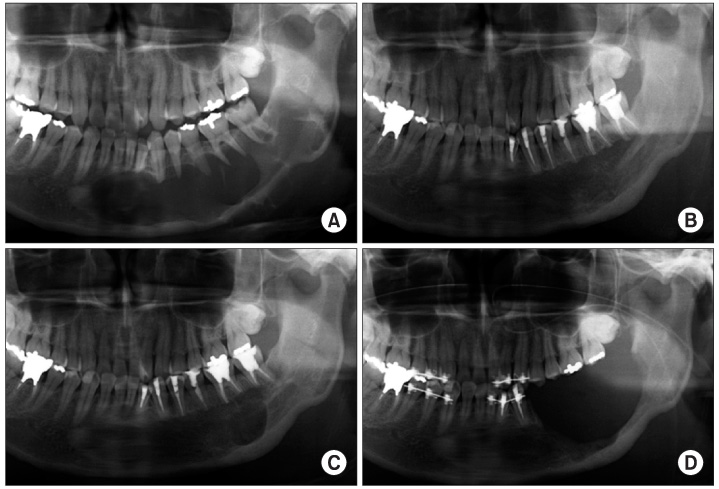
- The odontogenic keratocyst (OKC) was originally classified as a developmental cyst, and OKCs were histologically divided into orthokeratotic (O-OKCs) and parakeratotic (P-OKCs) types. Clinical features differ between O-OKCs and P-OKCs with P-OKCs having a tendency to recur after surgical treatment. According to the revised histopathological classification of odontogenic tumors by the World Health Organization (2005) , the term keratocystic odontogenic tumor (KCOT) has been adopted to describe P-OKCs. In this retrospective study, we examined 186 KCOTs treated at the Maxillofacial Surgery Department of the Tokyo Medical and Dental University Hospital from 1981 through 2005. The patients ranged in age from 7 to 85 years (mean, 32.7) and consisted of 93 males and 93 females. The most frequently treated areas were the mandibular molar region and ramus. The majority of KCOTs in the maxillary region were treated by enucleation and primary closure. The majority of KCOTs in the mandibular region were enucleated, and the wound was left open. Marginal resection was performed in the 4 patients with large lesions arising in the mandible. In patients who were followed for more than a year, recurrences were observed in 19 of 120 lesions (15.8%) . The recurrences were found at the margins of the primary lesion in contact with the roots of the teeth or at the upper margins of the mandibular ramus. Clinicians should consider aggressive treatment for KCOTs because the recurrence rate of P-OKCs is higher than that of other cyst types such as O-OKCs, dentigerous cysts, primordial cysts that were non-keratinized, and slightly keratinized stratified squamous epithelium. Although more aggressive treatment is needed for KCOTs as compared to other cystic lesions, it is difficult to make a precise diagnosis preoperatively on the basis of clinical features and X-ray imaging. Therefore, preoperative biopsy is necessary for selecting the appropriate treatment for patients with cystic lesions.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Protocol for management of odontogenic keratocysts considering recurrence according to treatment methods
Fadi Titinchi
J Korean Assoc Oral Maxillofac Surg. 2020;46(5):358-360. doi: 10.5125/jkaoms.2020.46.5.358.
Reference
-
1. Barnes L, Eveson JW, Reichart P. World Health Organization classification of tumours, pathology and genetics of tumours of the head and neck. 2005. Lyon: International Agency for Research on Cancer;306–307.2. Philipsen HP. Keratocysts in the jaws. Tandlaegeblader. 1956. 60:963–980.3. 原田昌和 , 山元 学. 当科における過去18年間の歯原性角化嚢胞 症例の検討. 日口外誌. 1988. 34:657–663.4. Ahlfors E, Larsson A, Sjögren S. The odontogenic keratocyst: a benign cystic tumor? J Oral Maxillofac Surg. 1984. 42:10–19.
Article5. Shear M. The aggressive nature of the odontogenic keratocyst: is it a benign cystic neoplasm? Part 1. Clinical and early experimental evidence of aggressive behaviour. Oral Oncol. 2002. 38:219–226.
Article6. Shear M. The aggressive nature of the odontogenic keratocyst: is it a benign cystic neoplasm? Part 2. Proliferation and genetic studies. Oral Oncol. 2002. 38:323–331.7. Gorlin RJ, Goltz RW. Multiple nevoid basal-cell epithelioma, jaw cysts and bifid rib. A syndrome. N Engl J Med. 1960. 262:908–912.
Article8. Pindborg JJ, Hansen J. Studies on odontogenic cyst epithelium. 2. clinical and roentgenologic aspects of odontogenic keratocysts. Acta Pathol Microbiol Scand. 1963. 58:283–294.9. Brannon RB. The odontogenic keratocyst. A clinicopathologic study of 312 cases. Part I. Clinical features. Oral Surg Oral Med Oral Pathol. 1976. 42:54–72.10. Brannon RB. The odontogenic keratocyst. A clinicopathologic study of 312 cases. Part II. Histologic features. Oral Surg Oral Med Oral Pathol. 1977. 43:233–255.11. 横林敏夫 , 横林康夫 . 歯原性角化嚢胞の再発に関する検討. 日口外誌. 1984. 30:1338–1347.12. 岩渕博史 , 矢郷 香. 歯原性角化嚢胞の角化のタイプによる臨 床病理学的相違. 日口外誌. 1996. 42:170–175.13. 鵜澤成一 , 喜代崎郁子 . 歯原性角化嚢胞に関する臨床的研究-再発に関する因子について-. 日口外誌. 2003. 49:93–98.14. 松木謙直 , 市原秀記 . 歯原性角化嚢胞 29 症例の臨床病理学的検討. 日口外誌. 2000. 46:232–234.15. Myoung H, Hong SP, Hong SD, Lee JI, Lim CY, Choung PH, et al. Odontogenic keratocyst: Review of 256 cases for recurrence and clinicopathologic parameters. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001. 91:328–333.
Article16. Morgan TA, Burton CC, Qian F. A retrospective review of treatment of the odontogenic keratocyst. J Oral Maxillofac Surg. 2005. 63:635–639.
Article17. Chirapathomsakul D, Sastravaha P, Jansisyanont P. A review of odontogenic keratocysts and the behavior of recurrences. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006. 101:5–9.
Article18. 飯野光喜 , 松田耕策 . 歯原性角化嚢胞 24 症例の臨床ならびに病理組織学的検討. 日口外誌. 1989. 35:964–973.19. 畑毅 , 細田 超. 歯原性角化嚢胞の臨床病理組織学的検討. 日口外誌. 1988. 34:470–484.20. Crowley TE, Kaugars GE, Gunsolley JC. Odontogenic keratocysts: a clinical and histologic comparison of the parakeratin and orthokeratin variants. J Oral Maxillofac Surg. 1992. 50:22–26.
Article21. 武田泰典 , 高田 隆. WHO による歯原性腫瘍の新たな組織分類とそれに関連する上皮性嚢胞について. 日口外誌. 2006. 52:54–61.22. 重松久夫 , 鈴木正二 . 歯原性角化嚢胞の治療とその再発に関する臨床病理学的検討. 日口外誌. 1998. 44:303–310.23. 永峰浩一郎 , 江場光芳 . 当講座における過去 11 年間の歯原性 角化嚢胞症例の検討. 日口外誌. 1991. 37:1853–1861.24. Browne RM. The odontogenic keratocyst. Clinical aspects. Br Dent J. 1970. 128:225–231.
Article25. 榎本昭二 , 岩佐俊昭 . 原始性嚢胞 (Primordialcysts) の臨床的研究. 日口外誌. 1977. 23:121–128.26. Forssell K, Sorvari TE, Oksala E. An analysis of the recurrence of odontogenic keratocysts. Proc Finn Dent Soc. 1974. 70:135–140.27. Bataineh AB, al Qudah M. Treatment of mandibular odontogenic keratocysts. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998. 86:42–47.
Article28. Brondum N, Jensen VJ. Recurrence of keratocysts and decompression treatment. A long-term follow-up of forty-four cases. Oral Surg Oral Med Oral Pathol. 1991. 72:265–269.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Radiological features of familial Gorlin-Goltz syndrome
- Carnoy's Solution Application for Patient Preliminarily Diagnosed with Keratocystic Odotogenic Tumor: Case Report
- Enucleation of large keratocystic odontogenic tumor at mandible via unilateral sagittal split osteotomy: a report of three cases
- Deep Neck Space Infection Caused by Keratocystic Odontogenic Tumor
- Diffusion-Weighted MR Imaging of Unicystic Odontogenic Tumors for Differentiation of Unicystic Ameloblastomas from Keratocystic Odontogenic Tumors