J Korean Neurotraumatol Soc.
2009 Dec;5(2):68-73. 10.13004/jknts.2009.5.2.68.
Spinal Epidural Abscess: Result of 39 Patients and Evaluation of Prognostic Factors
- Affiliations
-
- 1Department of Neurosurgery, Pusan National University School of Medicine, Yangsan, Korea. theworkholic@naver.com
- KMID: 1427360
- DOI: http://doi.org/10.13004/jknts.2009.5.2.68
Abstract
OBJECTIVE
Despite advances in neuroimaging and neurosurgical care, spinal abscess remains a challenging problem with high morbidity rate. So we conducted a retrospective study to define its clinical feature and to evaluate its prognostic factors.
METHODS
The charts of 39 patients with spinal epidural abscess over a 6-year period (from January 2001 to December 2006) were reviewed and analyzed.
RESULTS
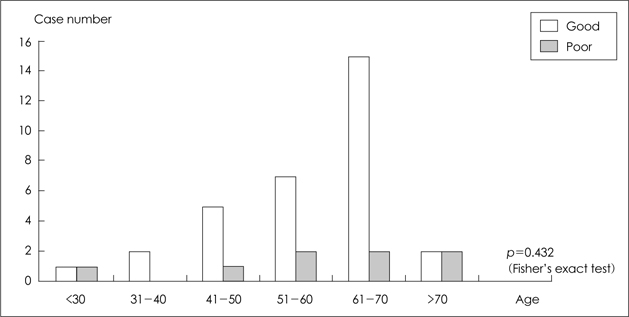
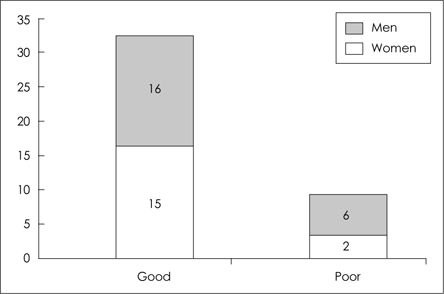
The 39 spinal epidural abscess included 22 men and 17 women with a mean age of 58 years. Localized spinal pain, paralysis, fever/chilling were the common manifestations. The most common pathogens were Mycobacterium tuberculosis, but we could not found pathogen in 19 cases. Decreased initial level of consciousness (drowsy-stupor) may predicted a poor prognosis, but no statistic significance.
CONCLUSION
Localized back pain in a febrile patient with significant risk of epidural abscess warrants an immediate evaluation. Good neurological recovery can be obtained despite severe neurologic deficit when treated by early diagnosis and prompt surgical intervention.
Keyword
MeSH Terms
Figure
Reference
-
1. Ahl T, Hedström M, von Heijne A, Hammers Stiernstedt S. Acute spinal epidural abscess without concurrent spondylodiscitis. Successful closed treatment in 10 cases. Acta Orthop Scand. 1999; 70:199–202.
Article2. Baker AS, Ojemann RG, Swartz MN, Richardson EP Jr. Spinal epidural abscess. N Engl J Med. 1975; 293:463–468.
Article3. Curling OD Jr, Gower DJ, McWhorter JM. Changing conce-pts in spinal epidural abscess: a report of 29 cases. Neurosurgery. 1990; 27:185–192.4. Danner RL, Hartman BJ. Update of spinal epidural abscess: 35 cases and review of the literature. Rev Infect Dis. 1987; 9:265–274.
Article5. Darouiche RO, Hamill RJ, Greenberg SB, Weathers SW, Musher DM. Bacterial spinal epidural abscess: review of 43 cases and literature survey. Medicine (Baltimore). 1992; 71:369–385.6. Del Curling O Jr, Grower DJ, McWhorter JM. Changing concepts in spinal epidural abscess: a report of 29 cases. Neurosurgery. 1990; 27:185–192.
Article7. Heusner AP. Nontuberculous spinal epidural infections. N Engl J Med. 1948; 239:845–854.
Article8. Hlavin ML, Kaminski HJ, Ross JS, Ganz E. Spinal epidural abscess: a ten-year perspective. Neurosurgery. 1990; 27:177–184.
Article9. Kaufman DM, Kaplan JG, Litman N. Infectious agents in spinal epidural abscesses. Neurology. 1980; 30:844–850.
Article10. Khanna RK, Malik GM, Rock JP, Rosenblum ML. Spinal epidural abscess: evaluation of factors influencing outcome. Neurosurgery. 1996; 39:958–964.
Article11. Krisht AF, Colohan ART. Spinal epidural abscess. Contemp Neurosurg. 1991; 13:1–6.
Article12. Lasker BR, Harter DH. Cervical epidural abscess. Neurology. 1987; 37:1747–1753.
Article13. Liem LK, Rigamonti D, Wolf AL, Robinson WL, Edwards CC, DiPatri A. Thoracic epidural abscess. J Spinal Disord. 1994; 7:449–454.
Article14. Mak KH, Au KK, Fung KY, Chan YW. Spinal epidural abscess: a report of nine cases and the use of intra-operative ultrasonography. Aust N Z J Surg. 1996; 66:287–290.
Article15. McGee-Collett M, Johnston IH. Spinal epidural abscess: presentation and treatment-A report of 21 cases. Med J Aust. 1991; 155:14–17.16. Numaguchi Y, Rigamonti D, Rothman MI, Sato S, Mihara F, Sadato N. Spinal epidural abscess evaluation with gadolinium enhanced MR imaging. Radiographics. 1993; 13:545–559.17. Nussbaum ES, Rigamonti D, Standiford H, Numaguchi Y, Wolf AL, Robinson WL. Spinal epidural abscess: a report of 40 cases and review. Surg Neurol. 1992; 38:225–231.
Article18. Okano K, Kondo H, Tsuchiya R, Naruke T, Sato M, Yokoyama R. Spinal epidural abscess associated with epidural catheterization: report of a case and a review of the literature. Jpn J Clin Oncol. 1999; 29:49–52.
Article19. Rea GL, McGregor JM, Miller CA, Miner ME. Surgical treatment of the spontaneous spinal epidural abscess. Surg Neurol. 1992; 37:274–279.
Article20. Sadato N, Numaguchi Y, Rigamonti D, Kodama T, Nussbaum E, Sato S, et al. Spinal epidural abscess with gadolinium-enhanced MRI: serial follow-up studies and clinical correlations. Neuroradiology. 1994; 36:44–48.
Article21. Sampath P, Rigamonti D. Spinal epidural abscess: a review of epidemiology, diagnosis and treatment. J Spinal Disord. 1999; 12:89–93.22. Soehle M, Wallenfang T. Spinal epidural abscesses: clinical manifestations, prognostic factors, and outcomes. Neurosurgery. 2002; 51:79–87.
Article23. Wheeler D, Keiser P, Rigamonti D, Keay S. Medical management of spinal epidural abscesses: case report and review. Clin Infect Dis. 1992; 15:22–27.
Article24. Yoo YS, Lee JC, Son EI, Kim DW, Yim MB, Lee CY, et al. Review of 10 cases of pyogenic epidural abscess of the spine. J Korean Neurosurg Soc. 1996; 25:1270–1276.25. Zeidman SM, Rhines L, Sampath P, Rigamonti D. Spinal epidural abscess. Contemp Neurosurg. 1995; 17:1–6.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Chronic Spinal Epidural Abscess after Epidural Analgesia: Case Report
- Development of Spinal Epidural Abscess during Treatment of Pneumococcal Meningitis
- Lumbar Spinal Epidural Abscess Combined with Cauda Equina Syndrome: A Case Report
- Serratia marcescens Spinal Epidural Abscess Following Caudal Epidural Injection
- Unusual Spinal Epidural Abscess without Predisposing Factors Treated Using a Minimally Invasive Technique