Korean J Perinatol.
2013 Mar;24(1):37-43. 10.14734/kjp.2013.24.1.37.
Fulminant Clinical Course on Listeria Sepsis in Preterm and Late Preterm Neonates
- Affiliations
-
- 1Department of Pediatrics, Wonkwang University School of Medicine, Iksan, Korea. oyk5412@wonkwang.ac.kr
- KMID: 1427074
- DOI: http://doi.org/10.14734/kjp.2013.24.1.37
Abstract
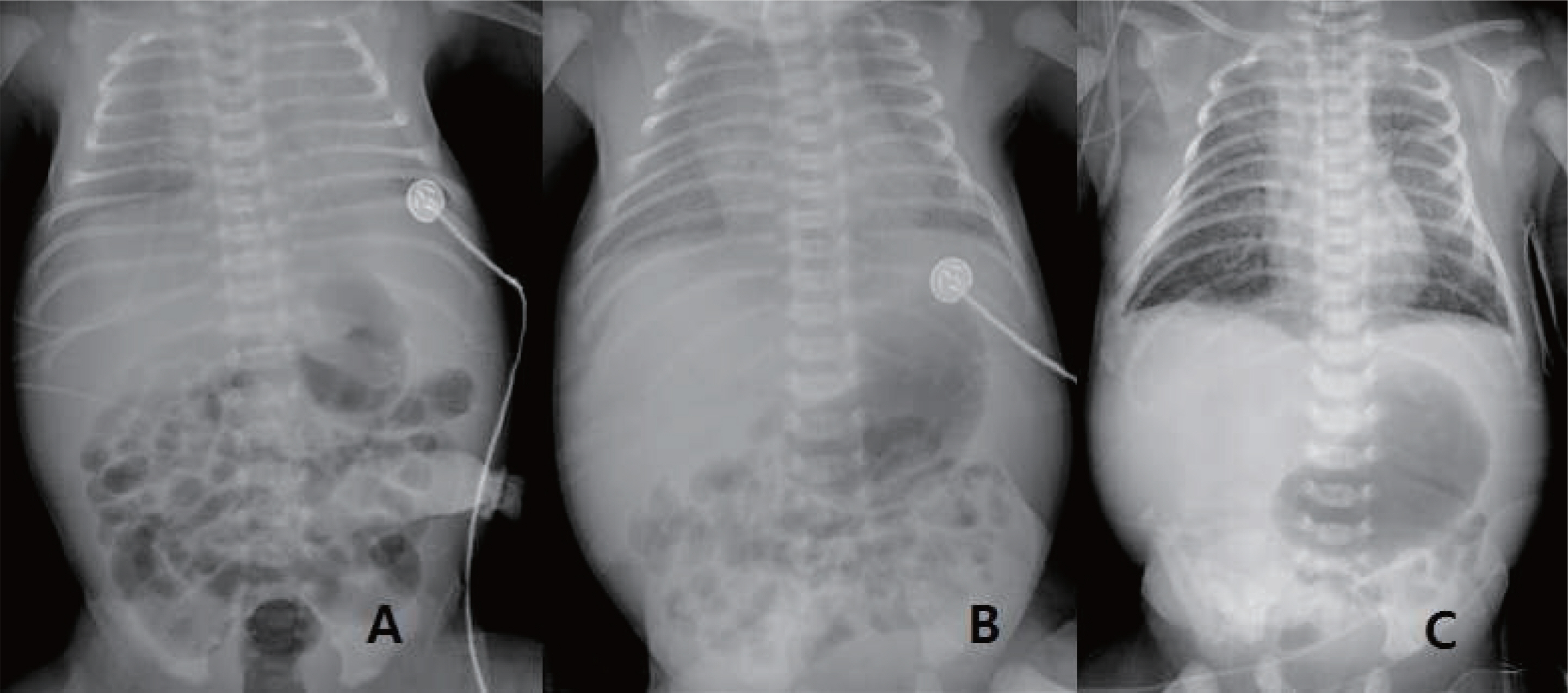
- Listeria monocytogenes is a facultative anaerobic, gram-positive bacillus. Listeria is commonly found in processed and prepared foods and listeriosis is associated with high morbidity and mortality. This bacterium is an important cause of severe infection in neonates and pregnant women. Pregnant women are at high risk for listeriosis, but symptoms are non-specific and diagnosis is difficult. Neonatal Listeriosis is generally a severe and fatal disease. There are two forms of the disease in the neonate, early- and late-onset, suggesting different modes of transmission. Generally, early detection and empirical treatment of listeriosis help to improve survival and prognosis. We explained two cases of L. monocytogenes sepsis with culture-proven in preterm and late preterm newborns from asymptomatic mothers. These neonates had fulminant clinical course even if standard antibiotics treatments were administrated.
MeSH Terms
Figure
Reference
-
1). Burn CG. Clinical and pathological features of an infection caused by a new pathogen of the genus Listerella. Am J Pathol. 1936. 12:341–8.2). Martin RJ., Fanaroff AA., Walsh MC. Fanaroff and Martin's Neonatal-Perinatal Medicine: Diseases of the Fetus and Infant. 9th ed.Philadelphia: WB Saunders Co;2011. p. 415–6.3). Lorber B. Listeriosis. Clin Infect Dis. 1997. 24:1–9.
Article4). Silver HM. Listeriosis during pregnancy. Obstet Gynecol Surv. 1998. 53:737–40.
Article5). Doganay M. Listeriosis: clinical presentation. FEMS Immunol Med Micobiol. 2003. 35:173–5.
Article6). Okutani A., Okada Y., Yamamoto S., Igimi S. Nationwide survey of humanListeria monocytogenes infection in Japan. Epidemiol Infect. 2004. 132:769–72.7). Cito G., Luisi S., Faldini E., Calonaci G., Sanseverino F., Torricelli M, et al. Listeriosis in pregnancy: a case report. J Matern Fetal Neonatal. 2005. 18:367–8.
Article8). Kim KR., Kim HM., Cho JY., Cha KS. Placetnal findings of septic abortion caused byListeria monocytogenes: a case report. Korean J Pathol. 1991. 25:387–91.9). Kim SC., Lee JT., Jung WK., Park BD., Zoo KR., Kim JW. A case of Listeriosis on third trimester with fetal distress. Korean J Obstet Gynecol. 1999. 42:194–7.10). Jung US., Lee ES., Yi KW., Min JY., Lee KJ. A case of Listeriosis in early third trimester pregnant woman. Korean J Obstet Gynecol. 2005. 48:194–8.11). Park JW., Yoon JM., Sung TJ. Listeria sepsis and pneumonia in a premature neonate. J Korean Soc Neonatol. 2009. 16:94–8.12). Voetsch AC., Angulo FJ., Jones TF., Moore MR., Nadon C., McCarthy P, et al. Reduction in the incidence of invasive listeriosis in foodborne diseases active surveillance network sites, 1996-2003. Clin Infect Dis. 2007. 44:513–20.
Article13). McLauchlin J., Hall SM., Velani SK., Gilbert RJ. Human listeriosis and pate: a possible association. BMJ. 1991. 303:773–5.
Article14). Mylonakis E., Paliou M., Hohmann EL., Calderwood SB., Wing EJ. Listeriosis during pregnancy: a case series and review of 222 cases. Medicine. 2002. 81:260–9.15). Posfay-Barbe KM., Wald ER. Listeriosis. Pediatr Rev. 2004. 25:151–9.
Article16). Tappero JW., Schuchat A., Deaver KA., Mascola L., Wenger JD. Reduction in the incidence of human listeriosis in the United States. JAMA. 1998. 273:1118–22.
Article17). Delgado AR. Listeriosis in pregnancy. J Midwifery Womens Health. 2008. 53:255–9.
Article18). Temple ME., Nahata MC. Treatment of listeriosis. Ann Phar-macother. 2000. 34:656–61.
Article19). Espaze EP., Reynaud AE. Antibiotic susceptibilities of Listeria: in vitro studies. Infection. 1988. 16(Suppl 2):S160–4.
Article20). Heikkinen T., Laine K., Neuvonen PJ., Ekblad U. The transplacental transfer of the macrolide antibiotics erythromycin, roxithromycin and azithromycin. BJOG. 2000. 107:770–5.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Early-Onset Sepsis Due to Listeria Monocytogenes in a Extremely Low Birth Weight Infant
- Clinical Characteristics of Apnea in Full-Term Infants: Compared to Late Preterm Infants
- Evaluation of the serum erythropoietin levels in neonates
- Obstetrical Management of Late Preterm Pregnancy
- Short-term clinical outcomes of late preterm infants