J Korean Neurosurg Soc.
2012 Dec;52(6):534-540. 10.3340/jkns.2012.52.6.534.
Radiosurgical Techniques and Clinical Outcomes of Gamma Knife Radiosurgery for Brainstem Arteriovenous Malformations
- Affiliations
-
- 1Department of Neurosurgery, Chuncheon Sacred Heart Hospital, Hallym University College of Medicine, Chuncheon, Korea.
- 2Department of Neurosurgery, School of Medicine, Kyung Hee University, Seoul, Korea. youngjinns@yahoo.co.kr
- KMID: 1426263
- DOI: http://doi.org/10.3340/jkns.2012.52.6.534
Abstract
OBJECTIVE
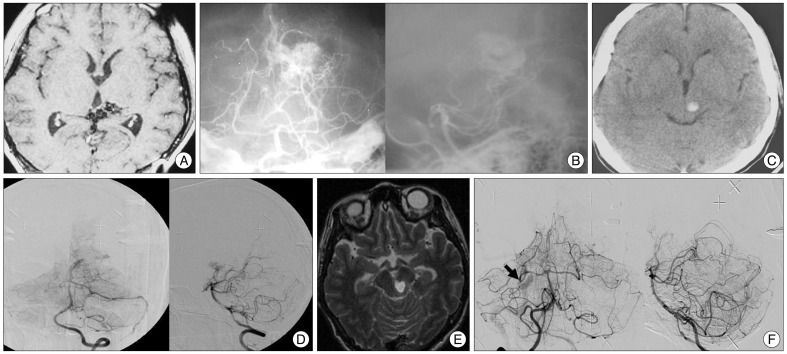
Brainstem arteriovenous malformation (AVM) is rare and radiosurgical management is complicated by the sensitivity of the adjacent neurological structures. Complete obliteration of the nidus is not always possible. We describe over 20 years of radiosurgical procedures for brainstem AVMs, focusing on clinical outcomes and radiosurgical techniques.
METHODS
Between 1992 and 2011, the authors performed gamma knife radiosurgery (GKRS) in 464 cerebral AVMs. Twenty-nine of the 464 patients (6.3%) reviewed had brainstem AVMs. This series included sixteen males and thirteen females with a mean age of 30.7 years (range : 5-71 years). The symptoms that led to diagnoses were as follows : an altered mentality (5 patients, 17.3%), motor weakness (10 patients, 34.5%), cranial nerve symptoms (3 patients, 10.3%), headache (6 patients, 20.7%), dizziness (3 patients, 10.3%), and seizures (2 patients, 6.9%). Two patients had undergone a previous nidus resection, and three patients had undergone a previous embolization. Twenty-four patients underwent only GKRS. With respect to the nidus type and blood flow, the ratio of compact type to diffuse type and high flow to low flow were 17 : 12 and 16 : 13, respectively. In this series, 24 patients (82.8%) had a prior hemorrhage. The mean target volume was 1.7 cm3 (range 0.1-11.3 cm3). The mean maximal and marginal radiation doses were 38.5 Gy (range 28.6-43.6 Gy) and 23.4 Gy (range 18-27 Gy), and the mean isodose profile was 61.3% (range 50-70%).
RESULTS
Twenty-four patients had brainstem AVMs and were followed for more than 3 years. Obliteration of the AVMs was eventually documented in 17 patients (70.8%) over a mean follow-up period of 77.5 months (range 36-216 months). With respect to nidus type and blood flow, the obliteration rate of compact types (75%) was higher than that of diffuse types (66.7%), and the obliteration rate of low flow AVMs (76.9%) was higher than that of high flow AVMs (63.6%) (p<0.05). Two patients (6.9%) with three hemorrhagic events suffered a hemorrhage during the follow-up period. The annual bleeding rate of AVM after GKRS was 1.95% per year. No adverse radiation effects or delayed cystic formations were found.
CONCLUSION
GKRS has an important clinical role in treatment of brainstem AVMs, which carry excessive surgical risks. Angiographic features and radiosurgical techniques using a lower maximal dose with higher isodose profiles are important for lesion obliteration and the avoidance of complications.
MeSH Terms
Figure
Reference
-
1. Alexander E 3rd, Loeffler JS. Radiosurgery for intracranial vascular malformations : techniques, results, and complications. Clin Neurosurg. 1992; 39:273–291. PMID: 1458744.2. Andrade-Souza YM, Zadeh G, Scora D, Tsao MN, Schwartz ML. Radiosurgery for basal ganglia, internal capsule, and thalamus arteriovenous malformation : clinical outcome. Neurosurgery. 2005; 56:56–63. discussion 63-64. PMID: 15617586.3. ApSimon HT, Reef H, Phadke RV, Popovic EA. A population-based study of brain arteriovenous malformation : long-term treatment outcomes. Stroke. 2002; 33:2794–2800. PMID: 12468772.
Article4. Batjer H, Samson D. Arteriovenous malformations of the posterior fossa. Clinical presentation, diagnostic evaluation, and surgical treatment. J Neurosurg. 1986; 64:849–856. PMID: 3701436.
Article5. Brown RD Jr, Wiebers DO, Torner JC, O'Fallon WM. Frequency of intracranial hemorrhage as a presenting symptom and subtype analysis : a population-based study of intracranial vascular malformations in Olmsted Country, Minnesota. J Neurosurg. 1996; 85:29–32. PMID: 8683279.
Article6. Chyatte D. Vascular malformations of the brain stem. J Neurosurg. 1989; 70:847–852. PMID: 2715811.
Article7. Drake CG, Friedman AH, Peerless SJ. Posterior fossa arteriovenous malformations. J Neurosurg. 1986; 64:1–10. PMID: 3484518.
Article8. Duma CM, Lunsford LD, Kondziolka D, Bissonette DJ, Somaza S, Flickinger JC. Radiosurgery for vascular malformations of the brain stem. Acta Neurochir Suppl (Wien). 1993; 58:92–97. PMID: 8109313.
Article9. Engenhart R, Wowra B, Debus J, Kimmig BN, Höver KH, Lorenz W, et al. The role of high-dose, single-fraction irradiation in small and large intracranial arteriovenous malformations. Int J Radiat Oncol Biol Phys. 1994; 30:521–529. PMID: 7928482.
Article10. Flickinger JC, Kondziolka D, Maitz AH, Lunsford LD. Analysis of neurological sequelae from radiosurgery of arteriovenous malformations : how location affects outcome. Int J Radiat Oncol Biol Phys. 1998; 40:273–278. PMID: 9457809.
Article11. Hartmann A, Mast H, Mohr JP, Koennecke HC, Osipov A, Pile-Spellman J, et al. Morbidity of intracranial hemorrhage in patients with cerebral arteriovenous malformation. Stroke. 1998; 29:931–934. PMID: 9596237.
Article12. Hosoda K, Fujita S, Kawaguchi T, Yamada H. A transcondylar approach to the arteriovenous malformation at the ventral cervicomedullary junction : report of three cases. Neurosurgery. 1994; 34:748–752. discussion 752-753. PMID: 8008179.
Article13. Kano H, Kondziolka D, Flickinger JC, Yang HC, Flannery TJ, Niranjan A, et al. Stereotactic radiosurgery for arteriovenous malformations, Part 5 : management of brainstem arteriovenous malformations. J Neurosurg. 2012; 116:44–53. PMID: 22077450.
Article14. Kondziolka D, Lunsford LD, Flickinger JC. Intraparenchymal brain stem radiosurgery. Neurosurg Clin N Am. 1993; 4:469–479. PMID: 8353445.
Article15. Kurita H, Kawamoto S, Sasaki T, Shin M, Tago M, Terahara A, et al. Results of radiosurgery for brain stem arteriovenous malformations. J Neurol Neurosurg Psychiatry. 2000; 68:563–570. PMID: 10766883.
Article16. Lawton MT, Hamilton MG, Spetzler RF. Multimodality treatment of deep arteriovenous malformations : thalamus, basal ganglia, and brain stem. Neurosurgery. 1995; 37:29–35. discussion 35-36. PMID: 8587687.17. Lee SH, Lim YJ, Choi SK, Kim TS, Rhee BA. Radiosurgical considerations in the treatment of large cerebral arteriovenous malformations. J Korean Neurosurg Soc. 2009; 46:378–384. PMID: 19893730.
Article18. Lunsford LD, Kondziolka D, Flickinger JC, Bissonette DJ, Jungreis CA, Maitz AH, et al. Stereotactic radiosurgery for arteriovenous malformations of the brain. J Neurosurg. 1991; 75:512–524. PMID: 1885968.
Article19. Maruyama K, Kondziolka D, Niranjan A, Flickinger JC, Lunsford LD. Stereotactic radiosurgery for brainstem arteriovenous malformations : factors affecting outcome. J Neurosurg. 2004; 100:407–413. PMID: 15035275.
Article20. Massager N, Régis J, Kondziolka D, Njee T, Levivier M. Gamma knife radiosurgery for brainstem arteriovenous malformations : preliminary results. J Neurosurg. 2000; 93(Suppl 3):102–103. PMID: 11143224.
Article21. Mast H, Young WL, Koennecke HC, Sciacca RR, Osipov A, Pile-Spellman J, et al. Risk of spontaneous haemorrhage after diagnosis of cerebral arteriovenous malformation. Lancet. 1997; 350:1065–1068. PMID: 10213548.
Article22. Ondra SL, Troupp H, George ED, Schwab K. The natural history of symptomatic arteriovenous malformations of the brain : a 24-year follow-up assessment. J Neurosurg. 1990; 73:387–391. PMID: 2384776.
Article23. Perret G, Nishioka H. Report on the cooperative study of intracranial aneurysms and subarachnoid hemorrhage. Section VI. Arteriovenous malformations. An analysis of 545 cases of cranio-cerebral arteriovenous malformations and fistulae reported to the cooperative study. J Neurosurg. 1966; 25:467–490. PMID: 5925721.24. Sasaki T, Kurita H, Saito I, Kawamoto S, Nemoto S, Terahara A, et al. Arteriovenous malformations in the basal ganglia and thalamus : management and results in 101 cases. J Neurosurg. 1998; 88:285–292. PMID: 9452237.
Article25. Solomon RA, Stein BM. Management of arteriovenous malformations of the brain stem. J Neurosurg. 1986; 64:857–864. PMID: 3701437.
Article26. Stefani MA, Porter PJ, terBrugge KG, Montanera W, Willinsky RA, Wallace MC. Angioarchitectural factors present in brain arteriovenous malformations associated with hemorrhagic presentation. Stroke. 2002; 33:920–924. PMID: 11935037.
Article27. Steiner L, Lindquist C, Adler JR, Torner JC, Alves W, Steiner M. Clinical outcome of radiosurgery for cerebral arteriovenous malformations. J Neurosurg. 1992; 77:1–8. PMID: 1607950.
Article28. Steiner L, Lindquist C, Cail W, Karlsson B, Steiner M. Microsurgery and radiosurgery in brain arteriovenous malformations. J Neurosurg. 1993; 79:647–652. PMID: 8410242.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- How to use Leksell GammaPlan
- Recurrence of pediatric cerebral arteriovenous malformation after obliteration by radiosurgery: a case report
- Factors Related to the Success of Gamma Knife Radiosurgery for Arteriovenous Malformations
- Gamma Knife Radiosurgery for Arteriovenous Malformations: Past Hope and Present Reality
- Radiosurgical Treatment of Cerebrovascular Malformations