Obstet Gynecol Sci.
2013 Mar;56(2):93-101. 10.5468/OGS.2013.56.2.93.
The ON-Q pain management system in elective gynecology oncologic surgery: Management of postoperative surgical site pain compared to intravenous patient-controlled analgesia
- Affiliations
-
- 1Division of Gynecologic Oncology, Department of Obstetrics and Gynecology, Yonsei University College of Medicine, Seoul, Korea. shkim70@yuhs.ac
- KMID: 1425656
- DOI: http://doi.org/10.5468/OGS.2013.56.2.93
Abstract
OBJECTIVE
The goal of this study was to compare postoperative surgical site pain in gynecologic cancer patients who underwent elective extended lower midline laparotomy and managed their pain with either the ON-Q pain management system (surgical incision site pain relief system, ON-Q pump) or an intravenous patient-controlled analgesia pump (IV PCA).
METHODS
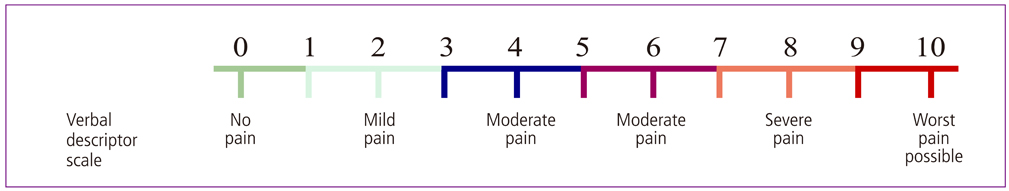
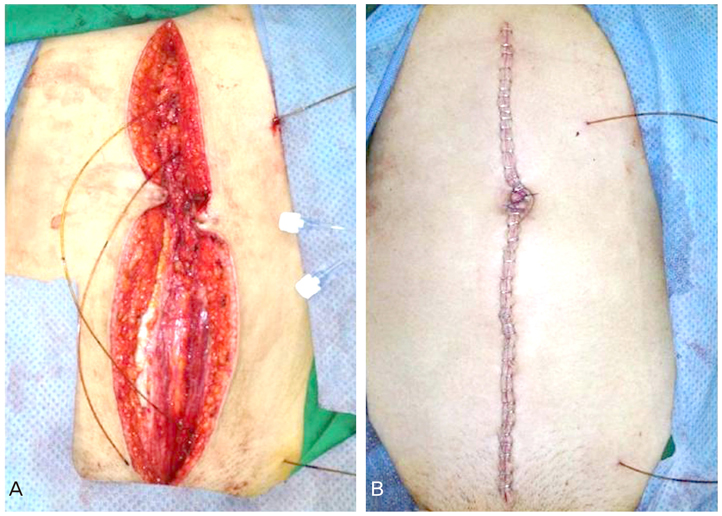
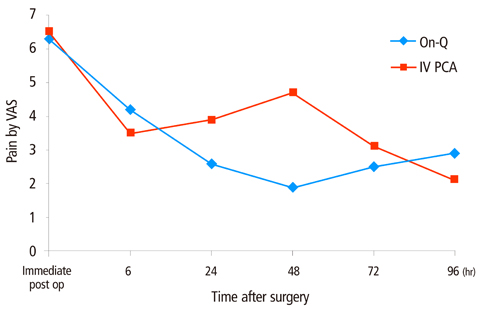
Twenty gynecologic cancer patients who underwent elective extended lower midline laparotomy were divided into two groups. One group received a 72-hour continuous wound perfusion of the local anesthetic ropivacaine (0.5%, study group) into the supraperitoneal layer of the abdominal incision through the ON-Q pump. The other group received intravenous infusion pump of patient-controlled analgesia (fentanyl citrate 20 mg/mL . kg+ondansetron hydrochloride 16 mg/8 mL+normal saline). Postoperative pain was assessed immediately and at 6, 24, 48, 72, and 96 hours after surgery using the visual analogue scale.
RESULTS
Postoperative surgical site pain scores at 24, 48, and 72 hours after surgery were lower in the ON-Q group than the IV PCA group. Pain scores at 24 hours and 48 hours after surgery were significantly different between the two groups (P=0.023, P<0.001). Overall painkiller administration was higher in the ON-Q group but this difference was not statistically significant (5.1 vs. 4.3, P=0.481).
CONCLUSION
This study revealed that the ON-Q pain management system is a more effective approach than IV PCA for acute postoperative surgical site pain relief after extended lower midline laparotomy in gynecologic cancer patients.
MeSH Terms
Figure
Reference
-
1. Kaplan JA, Miller ED Jr, Gallagher EG Jr. Postoperative analgesia for thoracotomy patients. Anesth Analg. 1975. 54:773–777.2. Sinclair R, Cassuto J, Hogstrom S, Linden I, Faxen A, Hedner T, et al. Topical anesthesia with lidocaine aerosol in the control of postoperative pain. Anesthesiology. 1988. 68:895–901.3. Partridge BL, Stabile BE. The effects of incisional bupivacaine on postoperative narcotic requirements, oxygen saturation and length of stay in the post-anesthesia care unit. Acta Anaesthesiol Scand. 1990. 34:486–491.4. Thomas DF, Lambert WG, Williams KL. The direct perfusion of surgical wounds with local anaesthetic solution: an approach to postoperative pain? Ann R Coll Surg Engl. 1983. 65:226–229.5. Chester JF, Ravindranath K, White BD, Shanahan D, Taylor RS, Lloyd-Williams K. Wound perfusion with bupivacaine: objective evidence for efficacy in postoperative pain relief. Ann R Coll Surg Engl. 1989. 71:394–396.6. Suzuki A, Yoshikawa M, Matsuzawa N. The effect of wound perfusion on the relief of postoperative pain. Masui. 1994. 43:96–101.7. Chen TF, Clarke N, Bowman R, Harper NJ, Payne SR. Intermuscular bupivacaine infusion for control of pain after renal surgery: a preliminary report. Br J Urol. 1994. 74:155–159.8. Gibbs P, Purushotham A, Auld C, Cuschieri RJ. Continuous wound perfusion with bupivacaine for postoperative wound pain. Br J Surg. 1988. 75:923–924.9. Patel JM, Lanzafame RJ, Williams JS, Mullen BV, Hinshaw JR. The effect of incisional infiltration of bupivacaine hydrochloride upon pulmonary functions, atelectasis and narcotic need following elective cholecystectomy. Surg Gynecol Obstet. 1983. 157:338–340.10. Levack ID, Holmes JD, Robertson GS. Abdominal wound perfusion for the relief of postoperative pain. Br J Anaesth. 1986. 58:615–619.11. Mecklem DW, Humphrey MD, Hicks RW. Efficacy of bupivacaine delivered by wound catheter for post-Caesarean section analgesia. Aust N Z J Obstet Gynaecol. 1995. 35:416–421.12. Moss G, Regal ME, Lichtig L. Reducing postoperative pain, narcotics, and length of hospitalization. Surgery. 1986. 99:206–210.13. Russell WC, Ramsay AH, Fletcher DR. The effect of incisional infiltration of bupivacaine upon pain and respiratory function following open cholecystectomy. Aust N Z J Surg. 1993. 63:756–759.14. Martin J, Neill RS. Venous plasma (total) bupivacaine concentrations following lower abdominal field block. Br J Anaesth. 1987. 59:1425–1430.15. Kastrissios H, Triggs EJ, Sinclair F, Moran P, Smithers M. Plasma concentrations of bupivacaine after wound infiltration of an 0.5% solution after inguinal herniorrhaphy: a preliminary study. Eur J Clin Pharmacol. 1993. 44:555–557.16. Hebel SK, Burnham TH. Drug facts and comparisons. 1996. St. Louis (MO): Wolters Kluwer Co..17. Fredman B, Shapiro A, Zohar E, Feldman E, Shorer S, Rawal N, et al. The analgesic efficacy of patient-controlled ropivacaine instillation after Cesarean delivery. Anesth Analg. 2000. 91:1436–1440.18. Givens VA, Lipscomb GH, Meyer NL. A randomized trial of postoperative wound irrigation with local anesthetic for pain after cesarean delivery. Am J Obstet Gynecol. 2002. 186:1188–1191.19. Gupta A, Perniola A, Axelsson K, Thorn SE, Crafoord K, Rawal N. Postoperative pain after abdominal hysterectomy: a double-blind comparison between placebo and local anesthetic infused intraperitoneally. Anesth Analg. 2004. 99:1173–1179.20. Tverskoy M, Cozacov C, Ayache M, Bradley EL Jr, Kissin I. Postoperative pain after inguinal herniorrhaphy with different types of anesthesia. Anesth Analg. 1990. 70:29–35.21. Kingsnorth AN, Wijesinha SS, Grixti CJ. Evaluation of dextran with local anaesthesia for short-stay inguinal herniorraphy. Ann R Coll Surg Engl. 1979. 61:456–458.22. Wall PD, Woolf CJ. The brief and the prolonged facilitatory effects of unmyelinated afferent input on the rat spinal cord are independently influenced by peripheral nerve section. Neuroscience. 1986. 17:1199–1205.23. Cook AJ, Woolf CJ, Wall PD, McMahon SB. Dynamic receptive field plasticity in rat spinal cord dorsal horn following C-primary afferent input. Nature. 1987. 325:151–153.24. Woolf CJ. Evidence for a central component of post-injury pain hypersensitivity. Nature. 1983. 306:686–688.25. Wall PD. The prevention of postoperative pain. Pain. 1988. 33:289–290.26. Capelle W. Die Bedentung deswundschmerzes und seiner ausschaltung fur dan ablauf der atmung bei laparotomierte. Dtsch Z Chir. 1935. 246:466–485.27. Blades B, Ford WB. A method for control of postoperative pain. Surg Gynecol Obstet. 1950. 91:524–526.28. Samarji WN. Rectus sheath analgesia in the control of postoperative abdominal pain and its influence on pulmonary function and complication. Proceedings of the 5th Congress Anaesthesiology. 1973. 1972; Kyoto, Japan. New York: Elsevier.29. Gerwig WH Jr, Thompson CW, Blades B. Pain control following upper abdominal operations. AMA Arch Surg. 1951. 62:678–682.30. Lewis DL, Thompson WA. Reduction of post-operative pain. Br Med J. 1953. 1:973–974.31. LeBlanc KA, Bellanger D, Rhynes VK, Hausmann M. Evaluation of continuous infusion of 0.5% bupivacaine by elastomeric pump for postoperative pain management after open inguinal hernia repair. J Am Coll Surg. 2005. 200:198–202.32. Schell SR. Patient outcomes after axillary lymph node dissection for breast cancer: use of postoperative continuous local anesthesia infusion. J Surg Res. 2006. 134:124–132.33. Lau H, Patil NG, Lee F. Randomized clinical trial of postoperative subfascial infusion with bupivacaine following ambulatory open mesh repair of inguinal hernia. Dig Surg. 2003. 20:285–289.34. Cheong WK, Seow-Choen F, Eu KW, Tang CL, Heah SM. Randomized clinical trial of local bupivacaine perfusion versus parenteral morphine infusion for pain relief after laparotomy. Br J Surg. 2001. 88:357–359.35. Polglase AL, McMurrick PJ, Simpson PJ, Wale RJ, Carne PW, Johnson W, et al. Continuous wound infusion of local anesthetic for the control of pain after elective abdominal colorectal surgery. Dis Colon Rectum. 2007. 50:2158–2167.36. Morrison JE Jr, Jacobs VR. Reduction or elimination of postoperative pain medication after mastectomy through use of a temporarily placed local anesthetic pump vs. control group. Zentralbl Gynakol. 2003. 125:17–22.37. White PF, Rawal S, Latham P, Markowitz S, Issioui T, Chi L, et al. Use of a continuous local anesthetic infusion for pain management after median sternotomy. Anesthesiology. 2003. 99:918–923.38. Schell SR. Patient analgesia after axillary lymph node dissection (ALND): outcomes in pain management using long-term continuous local anesthesia delivery. J Surg Res. 2003. 114:243–244.39. Sanchez B, Waxman K, Tatevossian R, Gamberdella M, Read B. Local anesthetic infusion pumps improve postoperative pain after inguinal hernia repair: a randomized trial. Am Surg. 2004. 70:1002–1006.40. Zimberg S, Guillermo D, Seiler J, Neimark M. ON-Q pain relief system in elective abdominal hysterectomy surgery, a pilot clinical outcomes study evaluating length of stay, postoperative pain, narcotic analgesia use and impact on costs and adverse effects. Presented at the 50th Annual Clinical Meeting of American Congress of Obstetricians and Gynecologists. 2002. 2002 May 4-8; Los Angeles, LA. Philadelphia: Lippincott Williams & Wilkins.41. Fujii S, Takakura K, Matsumura N, Higuchi T, Yura S, Mandai M, et al. Anatomic identification and functional outcomes of the nerve sparing Okabayashi radical hysterectomy. Gynecol Oncol. 2007. 107:4–13.42. Quinn MJ, Kirk N. Differences in uterine innervation at hysterectomy. Am J Obstet Gynecol. 2002. 187:1515–1519.43. Finder RL, Moore PA. Adverse drug reactions to local anesthesia. Dent Clin North Am. 2002. 46:747–757.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Postoperative Analgesia
- Comparison of Postoperative Analgesia and Side Effects by Patient-Controlled Epidural and Intravenous Analgesia after Cesarean Section
- Perioperative Pain Management in the Patient with Complex Regional Pain Syndrome: A case report
- Comparison of oxycodone and fentanyl for postoperative patient-controlled analgesia after laparoscopic gynecological surgery
- Postoperative pain management