Obstet Gynecol Sci.
2013 Mar;56(2):76-83. 10.5468/OGS.2013.56.2.76.
Clinicopathological significance of atypical glandular cells on Pap smear
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Pusan National University College of Medicine, Busan, Korea. dssuh@pusan.ac.kr
- 2Department of Pathology, Pusan National University College of Medicine, Busan, Korea.
- KMID: 1425654
- DOI: http://doi.org/10.5468/OGS.2013.56.2.76
Abstract
OBJECTIVE
To investigate the clinical significance of atypical glandular cells (AGC) by analyzing the prevalence and histologic outcomes of patients with AGC according to Pap smear.
METHODS
The medical records of 83 patients who were diagnosed AGC on Pap tests at the Pusan National University Hospital outpatient department and health care center from January 1998 to March 2006 were reviewed.
RESULTS
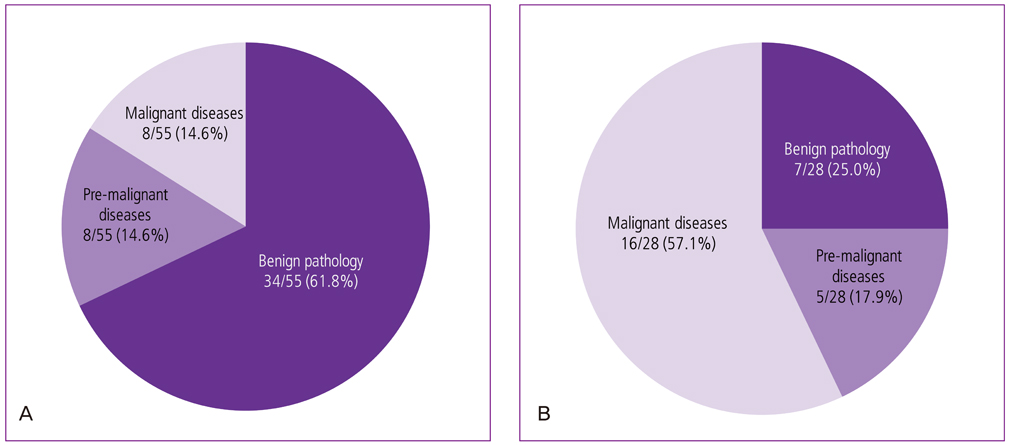
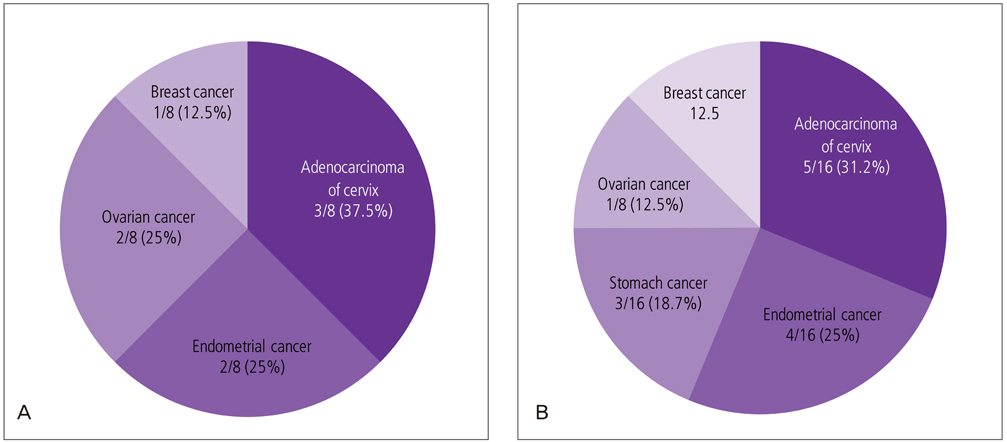
The prevalence of AGC was 55 of 54,160 (0.10%) and 28 of 54,160 (0.05%) for AGC-not otherwise specified (NOS) and neoplastic associated AGC, respectively. The histopathologic results of the AGC-NOS group (n=55) were as follows: low-grade squamous intraepithelial lesion, 7 (12.7%); high-grade squamous intraepithelial lesion, 4 (7.2%); adenocarcinoma of cervix, 3 (5.4%); endometrial carcinoma, 2 (3.6%); and other malignancies including 2 ovarian cancer cases and 1 breast cancer case, 3 (5.4%). The histopathologic results for the AGC-associated neoplastic group (n=28) were as follows: low-grade squamous intraepithelial lesion, 1 (3.5%); high-grade squamous intraepithelial lesion, 3 (10.7%); adenocarcinoma of cervix, 5 (17.8%); endometrial carcinoma, 4 (4.8%); and additional malignancies including 3 stomach cancer cases, 2 ovarian cancer cases, and 2 breast cancer cases; 7 (25%).
CONCLUSION
AGCs may represent a variety of benign and malignant lesions. AGC-associated neoplastic findings may be related to gynecological or extrauterine malignancies. Thus, when AGCs, especially neoplastic AGCs, are encountered, it is best to evaluate the cervix not only for typical maladies, but also for gynecological and non-gynecological malignancies.
Keyword
MeSH Terms
Figure
Reference
-
1. Central cancer registry center in Korea. Annual report of Korean central cancer registry (2002.1-2002.12). 2003. Goyang: Korean Central Cancer Registry Center, Ministry of Health & Welfare.2. SOG Gynecologic Oncology Committee. Annual report of gynecologic cancer registry program in Korea for 2004 (Jan. 1st, 2004-Dec. 31st, 2004). Korean J Obstet Gynecol. 2007. 50:28–78.3. Papanicolaou GN, Taut HF. The diagnostic value of vaginal smears in carcinoma of the uterus. Am J Obstet Gynecol. 1941. 42:193–206.4. Fremont-Smith M, Marino J, Griffin B, Spencer L, Bolick D. Comparison of the SurePath liquid-based Papanicolaou smear with the conventional Papanicolaou smear in a multisite direct-to-vial study. Cancer. 2004. 102:269–279.5. Wright TC Jr. Cervical cancer screening in the 21st century: is it time to retire the PAP smear? Clin Obstet Gynecol. 2007. 50:313–323.6. Collins LC, Wang HH, Abu-Jawdeh GM. Qualifiers of atypical squamous cells of undetermined significance help in patient management. Mod Pathol. 1996. 9:677–681.7. The Bethesda System for reporting cervical/vaginal cytologic diagnoses: revised after the second National Cancer Institute Workshop, April 29-30, 1991. Acta Cytol. 1993. 37:115–124.8. Solomon D, Davey D, Kurman R, Moriarty A, O'Connor D, Prey M, et al. The 2001 Bethesda System: terminology for reporting results of cervical cytology. JAMA. 2002. 287:2114–2119.9. Wright TC, Sun XW, Koulos J. Comparison of management algorithms for the evaluation of women with low-grade cytologic abnormalities. Obstet Gynecol. 1995. 85:202–210.10. Lonky NM, Navarre GL, Saunders S, Sadeghi M, Wolde-Tsadik G. Low-grade Papanicolaou smears and the Bethesda system: a prospective cytohistopathologic analysis. Obstet Gynecol. 1995. 85:716–720.11. Kinney WK, Manos MM, Hurley LB, Ransley JE. Where's the high-grade cervical neoplasia? The importance of minimally abnormal Papanicolaou diagnoses. Obstet Gynecol. 1998. 91:973–976.12. Cox JT. Management of atypical squamous cells of undetermined significance and low-grade squamous intra-epithelial lesion by human papillomavirus testing. Best Pract Res Clin Obstet Gynaecol. 2001. 15:715–741.13. Melnikow J, Nuovo J, Willan AR, Chan BK, Howell LP. Natural history of cervical squamous intraepithelial lesions: a meta-analysis. Obstet Gynecol. 1998. 92:727–735.14. Meath AJ, Carley ME, Wilson TO. Atypical glandular cells of undetermined significance. Review of final histologic diagnoses. J Reprod Med. 2002. 47:249–252.15. Bulk S, Berkhof J, Bulkmans NW, Zielinski GD, Rozendaal L, van Kemenade FJ, et al. Preferential risk of HPV16 for squamous cell carcinoma and of HPV18 for adenocarcinoma of the cervix compared to women with normal cytology in The Netherlands. Br J Cancer. 2006. 94:171–175.16. Chhieng DC, Elgert P, Cohen JM, Cangiarella JF. Clinical implications of atypical glandular cells of undetermined significance, favor endometrial origin. Cancer. 2001. 93:351–356.17. Seok WI, Lee KB, Lee JM, Nam UG, Yoon SJ, Choi SL, et al. Clinical analysis of atypical glandular cells of undetermined significance (AGUS) on Pap smear according to menopausal status. Korean J Obstet Gynecol. 2002. 45:967–971.18. Schnatz PF, Guile M, O'Sullivan DM, Sorosky JI. Clinical significance of atypical glandular cells on cervical cytology. Obstet Gynecol. 2006. 107:701–708.19. Schnatz PF, Pattison K, Mandavilli S, Fiel-Gan M, Elsaccar OA, O'Sullivan DM, et al. Atypical glandular cells on cervical cytology and breast disease: what is the association? J Low Genit Tract Dis. 2011. 15:189–194.20. Sharpless KE, Schnatz PF, Mandavilli S, Greene JF, Sorosky JI. Lack of adherence to practice guidelines for women with atypical glandular cells on cervical cytology. Obstet Gynecol. 2005. 105:501–506.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical significance of atypical glandular cells on Pap smear
- The Clinical Significance of Cervical ASCUS(Atypical Squamous Cells of Undetermined Significance) and Its Relationship with Eating Habits in Asymptommatic Women
- The correlation of result in Cervicography, Human papilloma virus test and cervical cytology as the screening tests of cervical neoplasia
- Diagnostic role of HPV DNA chip test in patient with atypical glandular cell cytology
- Comparison of papanicolaou smear and human papillomavirus (HPV) test as cervical screening tools: can we rely on HPV test alone as a screening method? An 11-year retrospective experience at a single institution