J Korean Soc Radiol.
2013 Apr;68(4):333-341. 10.3348/jksr.2013.68.4.333.
Radiology Residents' Performance in Screening Mammography Interpretation
- Affiliations
-
- 1Department of Radiology, Soonchunhyang University Bucheon Hospital, Soonchunhyang University College of Medicine, Bucheon, Korea. grace@schmc.ac.kr
- 2Department of Radiology, Seoul National University Bundang Hospital, Seongnam, Korea.
- KMID: 1425150
- DOI: http://doi.org/10.3348/jksr.2013.68.4.333
Abstract
- PURPOSE
To evaluate radiology residents' performance in screening mammography interpretation and to analyze the factors affecting performance.
MATERIALS AND METHODS
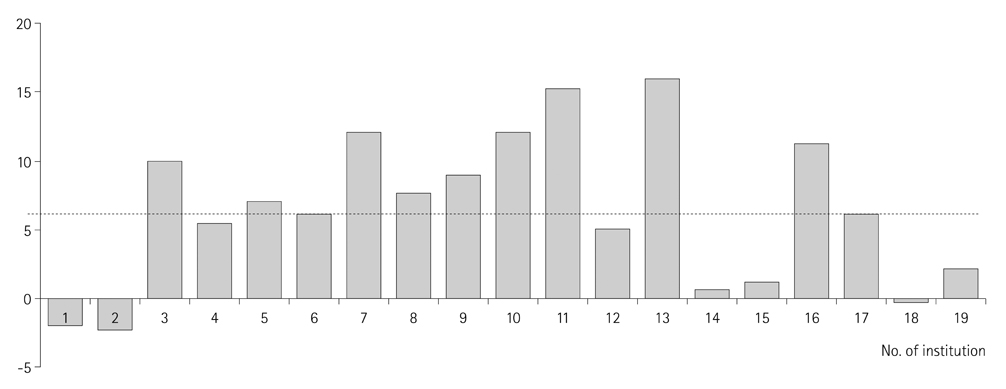
We enrolled 203 residents from 21 institutions and performed mammography interpretation tests. Between the trainee and non-trainee groups, we compared the interpretation score, recall rate, sensitivity, positive predictive value (PPV) and false-positive rate (FPR). We estimated the training effect using the score differences between trainee and non-trainee groups. We analyzed the factors affecting performance between training-effective and non-effective groups.
RESULTS
Trainees were superior to non-trainees regarding interpretation score (43.1 vs. 37.1), recall rate (11.0 vs. 15.5%), sensitivity (83.6 vs. 72.0%), PPV (53.0 vs. 32.4%) and FPR (13.5 vs. 25.5). The longer the training period, the better were the interpretation score, recall rate, sensitivity, PPV and FPR (rho = 0.486, -0.375, 0.343, 0.504, -0.446, respectively). The training affected an increase by an average of 6 points; however, 31.6% of institutions showed no effect. A difference was noted in the volume of mammography interpretation during a month (594.0 vs. 476.9) and dedication of breast staff (61.5 vs. 0%) between training-effective and non-effective groups.
CONCLUSION
Trainees showed better performance in mammography interpretation compared to non-trainees. Moreover, performance was correlated with the training period. The factors affecting performance were the volume of mammography interpretation and the dedication of the breast staff.
MeSH Terms
Figure
Cited by 1 articles
-
Radiology Residents’ Comprehension of the Breast Imaging Reporting and Data System: The Ultrasound Lexicon and Final Assessment Category
Sun Hye Jeong, Yun Ho Roh, Jung Hyun Yoon, Eun Hye Lee, Sung Hun Kim, Ji Hyun Youk, You Me Kim, Min Jung Kim
J Korean Soc Radiol. 2017;77(1):19-26. doi: 10.3348/jksr.2017.77.1.19.
Reference
-
1. Park EC. Extending an early cancer screening program: a study for construction of infra-structure and quality control. 2005. National cancer center:2. Paik SH. A study for correlation of assessment of special medical equipments and compensation of medical cost. 2012. Health insurance review and assessment service:3. Kim BS. Introduction of resident training system in Korean society of radiology. Orientation for new radiology residents. 2011.4. Shin HR. Assessment of outcome of early cancer screening program and setup of quality control system. 2002. National Cancer Center:5. Jun JK. The past, present and future of national cancer screening program. Workshop for quality control in mammography interpretation for national cancer screening program. 2011.6. Mammography Quality Standards Act (MQSA). Accessed 02 March 2011. Available at: http://www.fda.gov/Radiation-EmittingProducts/MammographyQualityStandardsActProgram.7. Year-specific details for residents training and teaching program. A notice from Ministry of Health 2011-174_Revised_2011.12.29.8. Resident training program. Workshop for members of committee of resident training in Korean society of radiology. 2010.9. Miglioretti DL, Gard CC, Carney PA, Onega TL, Buist DS, Sickles EA, et al. When radiologists perform best: the learning curve in screening mammogram interpretation. Radiology. 2009. 253:632–640.10. D'Orsi CJ, Bassett LW, Berg WA, Feig SA, Jackson VP, Kopan DB, et al. D'Orsi CJ, Mendelson EB, Ikeda DM, editors. BI-RADS: mammography. Breast Imaging Reporting and Data System: ACR-BIRADS-breast imaging atlas. 2003. 4th ed. Reston, VA: American College of Radiology.11. Bassett LW, Monsees BS, Smith RA, Wang L, Hooshi P, Farria DM, et al. Survey of radiology residents: breast imaging training and attitudes. Radiology. 2003. 227:862–869.12. Bassett LW, Bent C, Sayre JW, Marzan R, Verma A, Porter C. Breast imaging training and attitudes: update survey of senior radiology residents. AJR Am J Roentgenol. 2011. 197:263–269.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Interpreting Performance of Mammograms by Radiology Residents Trained in Breast Imaging: Comparison with Radiologists Who Attended Mammography Boot Camp
- Deep Learning-Based Artificial Intelligence for Mammography
- Breast Cancer Screening with MRI
- Medical auditing of whole-breast screening ultrasonography
- Benefits and Harms of Breast Screening: Focused on Updated Korean Guideline for Breast Cancer Screening