Clin Orthop Surg.
2013 Mar;5(1):19-25. 10.4055/cios.2013.5.1.19.
Prediction of Chronicity of Anterior Cruciate Ligament Tear Using MRI Findings
- Affiliations
-
- 1Department of Orthopaedic Surgery, Kyungpook National University Hospital, Daegu, Korea.
- 2Department of Orthopaedic Surgery, Sky Hospital, Seoul, Korea.
- 3Joint Reconstruction Center, Seoul National University Bundang Hospital, Seongnam, Korea. osktk@snubh.org
- 4Department of Statistics, Korea University, Seoul, Korea.
- 5Department of Radiology, Seoul National University Hospital, Seoul, Korea.
- 6Department of Radiology, Kyungpook National University Hospital, Daegu, Korea.
- KMID: 1402322
- DOI: http://doi.org/10.4055/cios.2013.5.1.19
Abstract
- BACKGROUND
The estimation of anterior cruciate ligament (ACL) tear is required in certain cases involving legal and financial administration, such as the worker's compensation and/or insurance. The aim of this study is to propose and evaluate a quantitative evaluation instrument to estimate the chronicity of the ACL tear, based on the four magnetic resonance imaging (MRI) findings.
METHODS
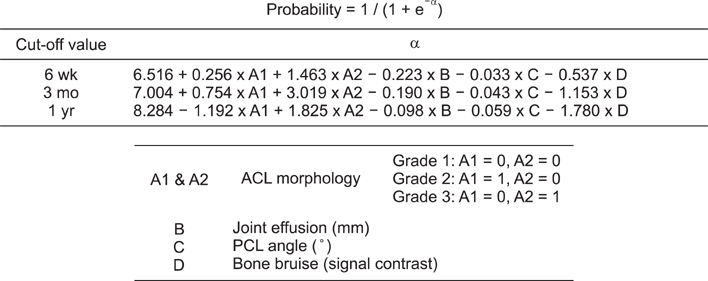
One hundred and fifty one cases of complete ACL tear confirmed by arthroscopy were divided into 4 groups according to the time from ACL injury to MRI acquisition: acute (< 6 weeks), subacute (6 weeks to 3 months), intermediate (3 months to 1 year), and chronic (> 1 year). The four MRI findings including ACL morphology, joint effusion, posterior cruciate ligament angle, and bone bruise were analyzed for temporal changes among the 4 groups. Binary logistic regression equations were formulated using the MRI findings to estimate the chronicity of ACL tear in a quantitative manner, and the accuracy of the formulated regression equations was evaluated.
RESULTS
The four MRI findings showed substantial temporal correlation with the time-limits of ACL injury to be included in the estimation model. Three predictive binary logistic equations estimated the probability of the ACL injury for the three cutoff time-limits of 6 weeks, 3 months, and 1 year with accuracies of 82.1%, 89.4%, and 89.4%, respectively.
CONCLUSIONS
A series of predictive logistic equations were formulated to estimate the chronicity of ACL tear using 4 MRI findings with chronological significance.
MeSH Terms
Figure
Reference
-
1. Dimond PM, Fadale PD, Hulstyn MJ, Tung GA, Greisberg J. A comparison of MRI findings in patients with acute and chronic ACL tears. Am J Knee Surg. 1998. 11(3):153–159.2. Johnson MW. Acute knee effusions: a systematic approach to diagnosis. Am Fam Physician. 2000. 61(8):2391–2400.3. Gentili A, Seeger LL, Yao L, Do HM. Anterior cruciate ligament tear: indirect signs at MR imaging. Radiology. 1994. 193(3):835–840.
Article4. Vahey TN, Broome DR, Kayes KJ, Shelbourne KD. Acute and chronic tears of the anterior cruciate ligament: differential features at MR imaging. Radiology. 1991. 181(1):251–253.
Article5. Vahey TN, Hunt JE, Shelbourne KD. Anterior translocation of the tibia at MR imaging: a secondary sign of anterior cruciate ligament tear. Radiology. 1993. 187(3):817–819.
Article6. Yoon JP, Chang CB, Yoo JH, et al. Correlation of magnetic resonance imaging findings with the chronicity of an anterior cruciate ligament tear. J Bone Joint Surg Am. 2010. 92(2):353–360.
Article7. McCauley TR, Moses M, Kier R, Lynch JK, Barton JW, Jokl P. MR diagnosis of tears of anterior cruciate ligament of the knee: importance of ancillary findings. AJR Am J Roentgenol. 1994. 162(1):115–119.
Article8. Vellet AD, Marks PH, Fowler PJ, Munro TG. Occult posttraumatic osteochondral lesions of the knee: prevalence, classification, and short-term sequelae evaluated with MR imaging. Radiology. 1991. 178(1):271–276.
Article9. Boks SS, Vroegindeweij D, Koes BW, Hunink MM, Bierma-Zeinstra SM. Magnetic resonance imaging abnormalities in symptomatic and contralateral knees: prevalence and associations with traumatic history in general practice. Am J Sports Med. 2006. 34(12):1984–1991.
Article10. Lee K, Siegel MJ, Lau DM, Hildebolt CF, Matava MJ. Anterior cruciate ligament tears: MR imaging-based diagnosis in a pediatric population. Radiology. 1999. 213(3):697–704.
Article11. Rosen MA, Jackson DW, Berger PE. Occult osseous lesions documented by magnetic resonance imaging associated with anterior cruciate ligament ruptures. Arthroscopy. 1991. 7(1):45–51.
Article12. Bretlau T, Tuxoe J, Larsen L, Jorgensen U, Thomsen HS, Lausten GS. Bone bruise in the acutely injured knee. Knee Surg Sports Traumatol Arthrosc. 2002. 10(2):96–101.
Article13. Costa-Paz M, Muscolo DL, Ayerza M, Makino A, Aponte-Tinao L. Magnetic resonance imaging follow-up study of bone bruises associated with anterior cruciate ligament ruptures. Arthroscopy. 2001. 17(5):445–449.
Article14. Davies NH, Niall D, King LJ, Lavelle J, Healy JC. Magnetic resonance imaging of bone bruising in the acutely injured knee: short-term outcome. Clin Radiol. 2004. 59(5):439–445.
Article15. Roemer FW, Bohndorf K. Long-term osseous sequelae after acute trauma of the knee joint evaluated by MRI. Skeletal Radiol. 2002. 31(11):615–623.
Article16. Mink JH, Deutsch AL. Magnetic resonance imaging of the knee. Clin Orthop Relat Res. 1989. (244):29–47.
Article17. Chen WT, Shih TT, Tu HY, Chen RC, Shau WY. Partial and complete tear of the anterior cruciate ligament. Acta Radiol. 2002. 43(5):511–516.
Article18. Kolman BH, Daffner RH, Sciulli RL, Soehnlen MW. Correlation of joint fluid and internal derangement on knee MRI. Skeletal Radiol. 2004. 33(2):91–95.
Article19. Schweitzer ME, Falk A, Berthoty D, Mitchell M, Resnick D. Knee effusion: normal distribution of fluid. AJR Am J Roentgenol. 1992. 159(2):361–363.
Article20. Brittberg M, Winalski CS. Evaluation of cartilage injuries and repair. J Bone Joint Surg Am. 2003. 85:Suppl 2. 58–69.
Article21. Schmid MR, Hodler J, Vienne P, Binkert CA, Zanetti M. Bone marrow abnormalities of foot and ankle: STIR versus T1-weighted contrast-enhanced fat-suppressed spin-echo MR imaging. Radiology. 2002. 224(2):463–469.
Article22. Vogl TJ, Schmitt J, Lubrich J, et al. Reconstructed anterior cruciate ligaments using patellar tendon ligament grafts: diagnostic value of contrast-enhanced MRI in a 2-year follow-up regimen. Eur Radiol. 2001. 11(8):1450–1456.
Article23. Robertson PL, Schweitzer ME, Bartolozzi AR, Ugoni A. Anterior cruciate ligament tears: evaluation of multiple signs with MR imaging. Radiology. 1994. 193(3):829–834.
Article24. Mellado JM, Calmet J, Olona M, Gine J, Sauri A. Magnetic resonance imaging of anterior cruciate ligament tears: reevaluation of quantitative parameters and imaging findings including a simplified method for measuring the anterior cruciate ligament angle. Knee Surg Sports Traumatol Arthrosc. 2004. 12(3):217–224.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pitalls in Interpretation of Physical Tests of Knee Ligament Injury
- The Efficacy of MRI in Anterior Cruciate Ligamant Injury
- The Primary Repair of Acute Anterior Cruciate Ligament Injury
- Ganglion Cyst on the Anterior Cruciate Ligament: A Case Report
- MRI Diagnosis of Associated Injuries in Complete Tears of Posterior Cruciate Ligament of the Knee