Korean J Radiol.
2012 Oct;13(5):637-642. 10.3348/kjr.2012.13.5.637.
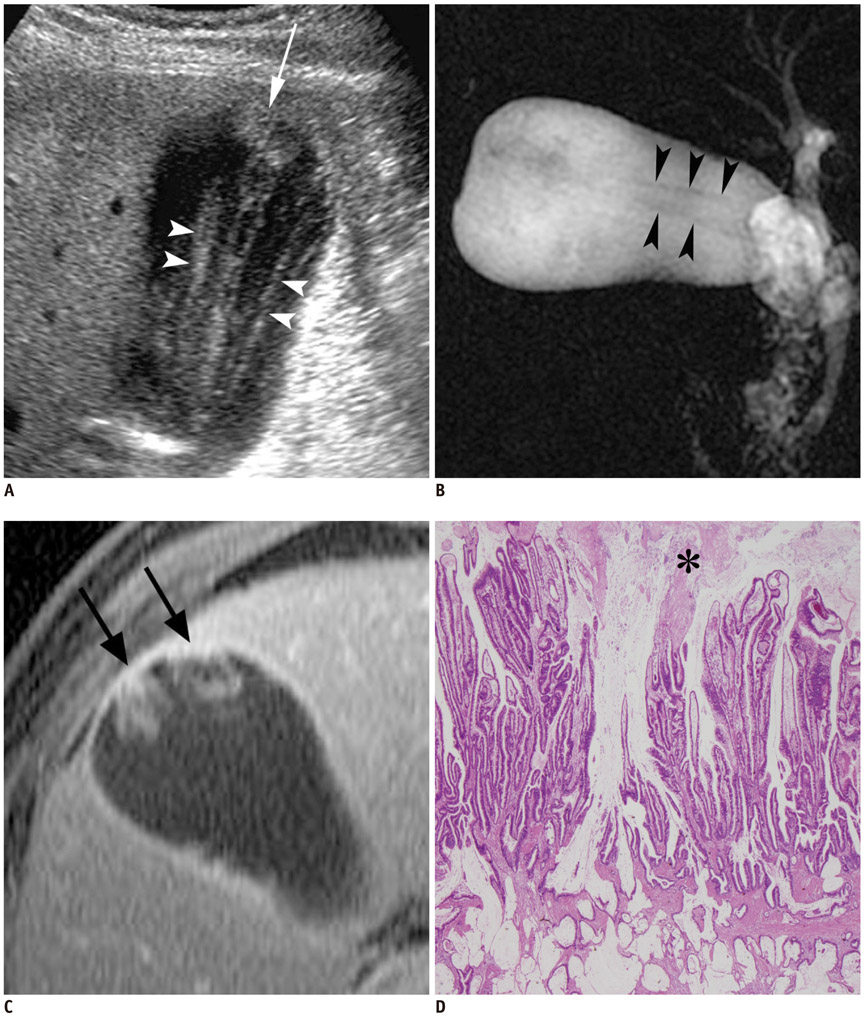
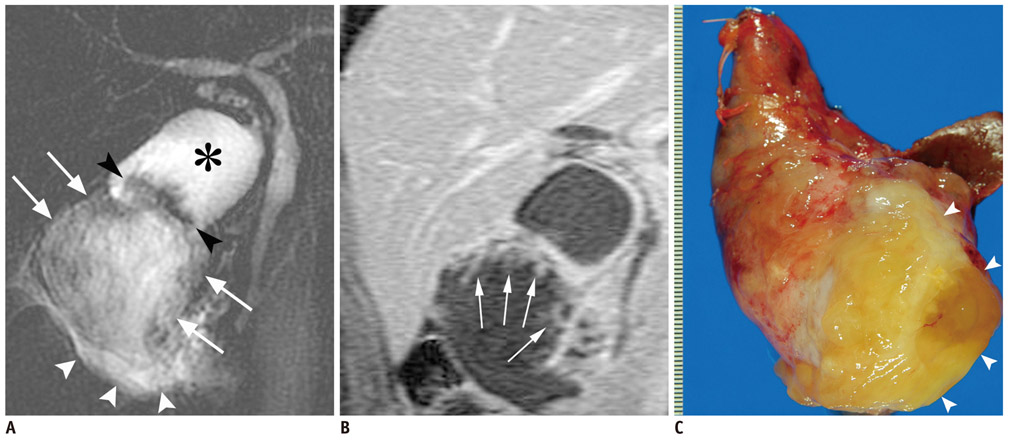
Mucin-Producing Carcinoma of the Gallbladder: Evaluation by Magnetic Resonance Cholangiopancreatography in Three Cases
- Affiliations
-
- 1Hepatobiliary and Pancreatic Surgery Division, National Cancer Center Hospital, Tokyo 104-0045, Japan.
- 2Diagnostic Radiology Division, National Cancer Center Hospital, Tokyo 104-0045, Japan. honaya@ncc.go.jp
- 3Pathology Division, National Cancer Center Hospital, Tokyo 104-0045, Japan.
- KMID: 1392944
- DOI: http://doi.org/10.3348/kjr.2012.13.5.637
Abstract
- We report three cases of mucin-producing carcinoma of the gallbladder, along with the magnetic resonance (MR) findings, especially the findings on a MR cholangiopancreatography. In our cases, linear or curvilinear streaks were detected running along the long axis of an enlarged gallbladder (mucus thread sign). When such findings were seen, a mucin-producing carcinoma of the gallbladder should be included as a differential diagnosis. Thus, gadolinium-enhanced MR imaging is mandatory for the precise diagnosis of the mucin-producing carcinoma of the gallbladder.
Keyword
MeSH Terms
Figure
Reference
-
1. Levy AD, Murakata LA, Rohrmann CA Jr. Gallbladder carcinoma: radiologic-pathologic correlation. Radiographics. 2001. 21:295–314. questionnaire 549-555.2. Lim JH, Yi CA, Lim HK, Lee WJ, Lee SJ, Kim SH. Radiological spectrum of intraductal papillary tumors of the bile ducts. Korean J Radiol. 2002. 3:57–63.3. Ishibashi H, Hachisuka K, Yamaguchi A, Isogai M, Fukada S, Kato S, et al. Mucin-producing gallbladder carcinoma: report of a case. Tan to Sui. 1986. 7:1173–1178.4. Tian H, Matsumoto S, Takaki H, Kiyosue H, Komatsu E, Okino Y, et al. Mucin-producing carcinoma of the gallbladder: imaging demonstration in four cases. J Comput Assist Tomogr. 2003. 27:150–154.5. Ozeki Y, Matsubara N, Saiga T, Homma M, Koyama A, Ichikawa T, et al. Mucus-producing cancer of the gallbladder: report of a case. Gastroenterol Endosc. 1991. 33:2439–2444.6. Huang CP, Chiou YY, Chou YH, Chiang JH, Chang CY. Imaging findings in mucin-producing carcinoma of the gallbladder. J Formos Med Assoc. 2006. 105:427–430.7. Lim JH, Yoon KH, Kim SH, Kim HY, Lim HK, Song SY, et al. Intraductal papillary mucinous tumor of the bile ducts. Radiographics. 2004. 24:53–66. discussion 66-67.8. Miyazaki T, Yamashita Y, Tsuchigame T, Yamamoto H, Urata J, Takahashi M. MR cholangiopancreatography using HASTE (half-Fourier acquisition single-shot turbo spin-echo) sequences. AJR Am J Roentgenol. 1996. 166:1297–1303.9. Irie H, Honda H, Tajima T, Kuroiwa T, Yoshimitsu K, Makisumi K, et al. Optimal MR cholangiopancreatographic sequence and its clinical application. Radiology. 1998. 206:379–387.10. Nobusawa H, Hashimoto T, Munechika H, Soejima K, Seino N, Kurashita Y, et al. [US and CT findings of mucinous carcinomas of the gallbladder]. Nihon Igaku Hoshasen Gakkai Zasshi. 1994. 54:1359–1367.11. Miyake H, Hori Y, Dono S, Mori H. Low attenuation intratumoral matrix: CT and pathologic correlation. J Comput Assist Tomogr. 2000. 24:761–772.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Incidentally detected gallbladder agenesis in a child: the importance of identifying anatomic structure
- Radiologic Evaluation and Differential Diagnosis of Gallbladder Cancer
- Synchronous Undifferentiated Carcinoma of Gallbladder in a Patient with Intrahepatic Intraductal Papillary Mucinous Neoplasia (b-IPMN)
- Clinical Significance of Anomalous Pancreaticobiliary Ductal Union Diagnosed by Endoscopic Retrograde Cholangiopancreatography
- Alpha-Fetoprotein-Producing Carcinoma of the Gallbladder