Korean J Radiol.
2012 Oct;13(5):618-624. 10.3348/kjr.2012.13.5.618.
Uterine Artery Embolization for Symptomatic Fibroids with High Signal Intensity on T2-Weighted MR Imaging
- Affiliations
-
- 1Department of Radiology, Research Institute of Radiological Science, Yonsei University College of Medicine, Severance Hospital, Seoul 120-752, Korea. mdkim@yuhs.ac
- KMID: 1392941
- DOI: http://doi.org/10.3348/kjr.2012.13.5.618
Abstract
OBJECTIVE
To evaluate the effectiveness of uterine artery embolization (UAE) for treating symptomatic fibroids with high signal intensity (SI) on magnetic resonance (MR) T2-weighted imaging (T2WI).
MATERIALS AND METHODS
A total of 537 cases, consisting of 14 patients with high SI fibroids on T2WI (T2 high group), were retrospectively included and compared with 28 randomly selected patients with low SI fibroids on T2WI (control group). High SI of a predominant fibroid on T2WI was defined as having the same or higher SI than the myometrium. Patient ages ranged from 28 to 52 years (mean, 38.1 years). All patients underwent MRI before and after UAE. Predominant fibroid and uterine volumes were calculated with MR images. Symptom status in terms of menorrhagia and dysmenorrhea was scored on a scale of 0-10, with 0 being no symptoms and 10 being the baseline, or initial symptoms.
RESULTS
Of the patients in the T2 high group, 13 out of 14 (92.9%) patients demonstrated complete necrosis of the predominant fibroids. The mean volume reduction rates of the predominant fibroids in the T2 high group was 61.7% at three months after UAE, which was significantly higher than the volume reduction rates of 42.1% noted in the control group (p < 0.05). Changes in symptom scores for menorrhagia and dysmenorrhea after UAE (baseline score minus follow-up score) were 4.9 and 7.5 in T2 high group and they were 5.0 and 7.7 in control group, suggesting a significant resolution of symptoms (p < 0.01) in both groups but no significant difference between the two groups.
CONCLUSION
UAE is effective for uttering fibroids showing high SI on T2WI. The mean volume reduction rate of the predominant fibroids three months after UAE was greater in the T2 high group than in the control group.
Keyword
MeSH Terms
-
Adult
Case-Control Studies
Contrast Media/diagnostic use
Female
Humans
Leiomyoma/*therapy
Magnetic Resonance Imaging, Interventional/*methods
Meglumine/diagnostic use
Middle Aged
Organometallic Compounds/diagnostic use
Questionnaires
Retrospective Studies
Treatment Outcome
Uterine Artery Embolization/*methods
Uterine Neoplasms/*therapy
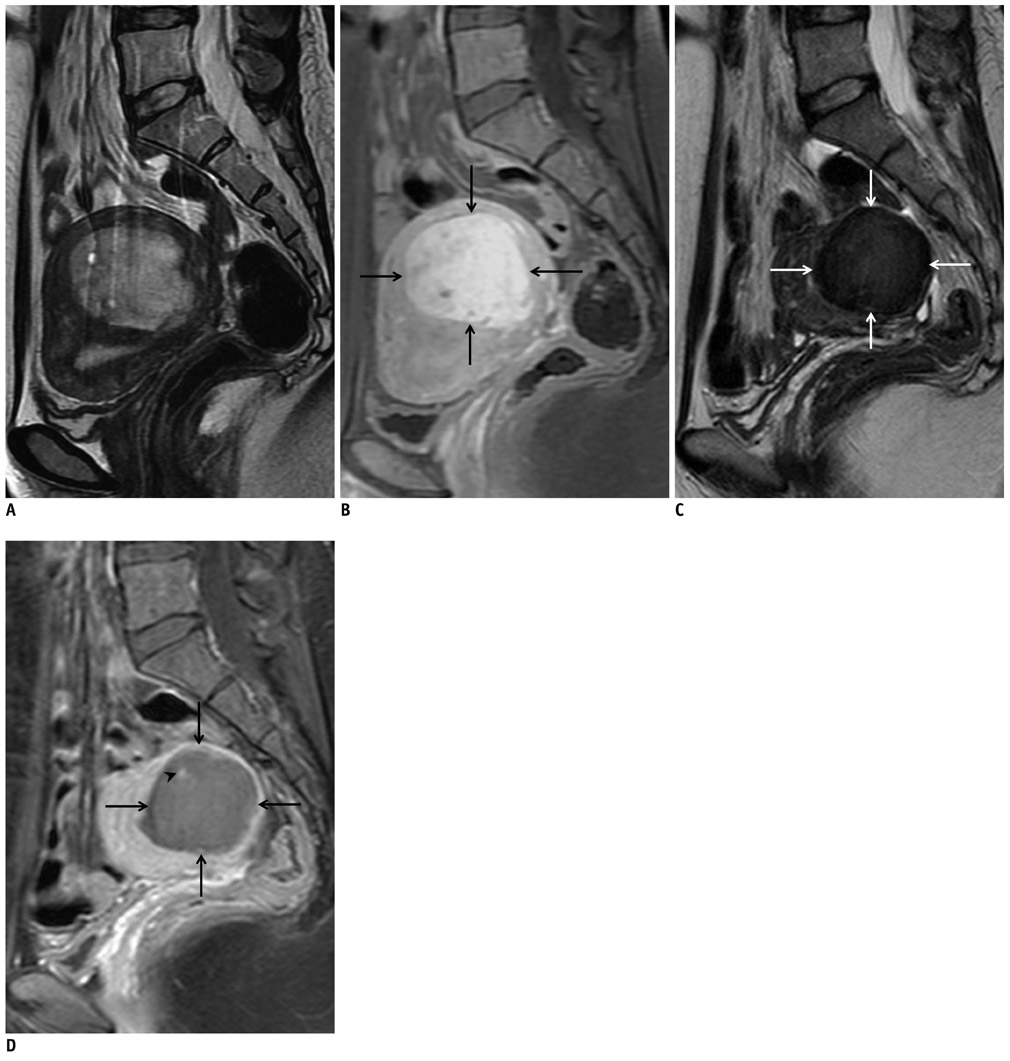
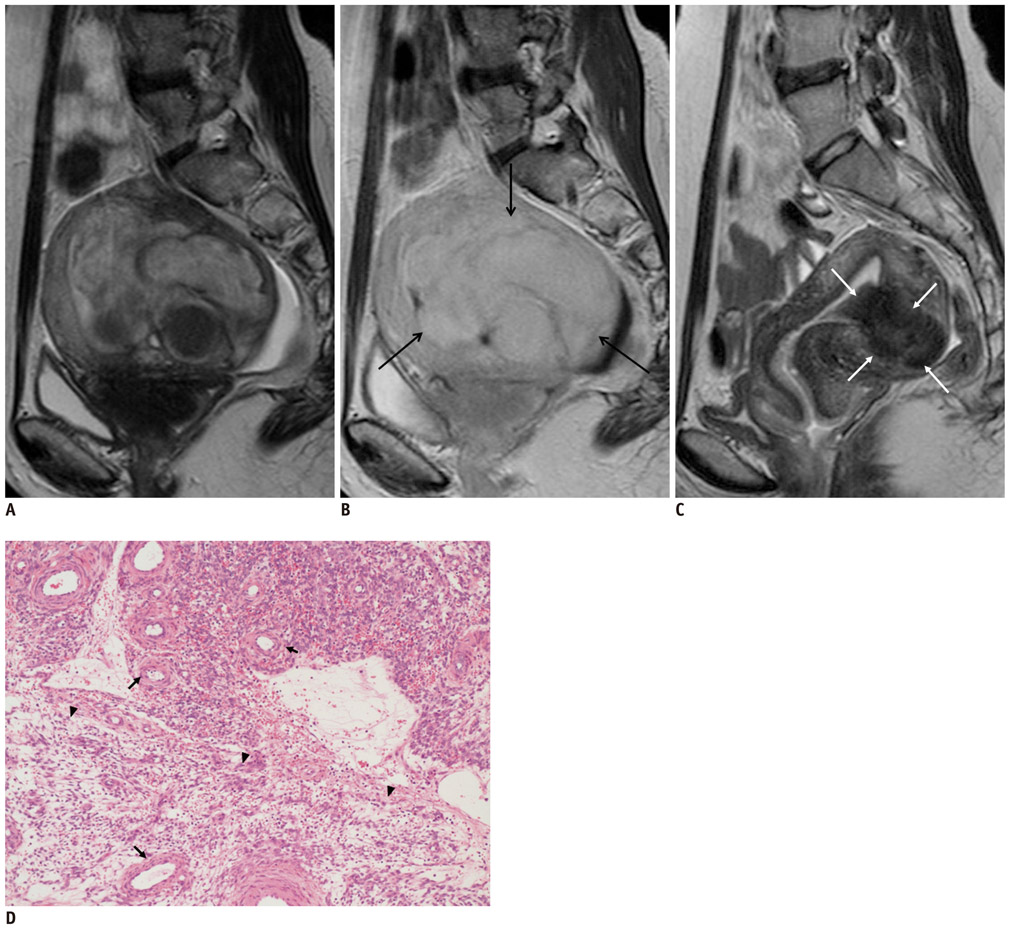
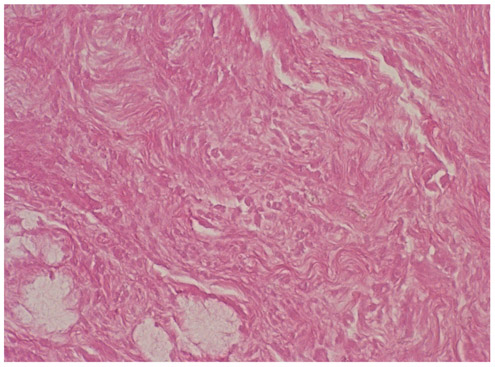
Figure
Cited by 1 articles
-
Uterine Artery Embolization for Leiomyomas and Adenomyosis: A Pictorial Essay Based on Our Experience from 1300 Cases
Man-Deuk Kim
Korean J Radiol. 2019;20(10):1462-1473. doi: 10.3348/kjr.2019.0205.
Reference
-
1. Walker WJ, Pelage JP. Uterine artery embolisation for symptomatic fibroids: clinical results in 400 women with imaging follow up. BJOG. 2002. 109:1262–1272.2. Spies JB, Ascher SA, Roth AR, Kim J, Levy EB, Gomez-Jorge J. Uterine artery embolization for leiomyomata. Obstet Gynecol. 2001. 98:29–34.3. Hovsepian DM, Siskin GP, Bonn J, Cardella JF, Clark TW, Lampmann LE, et al. Quality improvement guidelines for uterine artery embolization for symptomatic leiomyomata. J Vasc Interv Radiol. 2009. 20:7 Suppl. S193–S199.4. Funaki K, Fukunishi H, Sawada K. Clinical outcomes of magnetic resonance-guided focused ultrasound surgery for uterine myomas: 24-month follow-up. Ultrasound Obstet Gynecol. 2009. 34:584–589.5. Oguchi O, Mori A, Kobayashi Y, Horiuchi A, Nikaido T, Fujii S. Prediction of histopathologic features and proliferative activity of uterine leiomyoma by magnetic resonance imaging prior to GnRH analogue therapy: correlation between T2-weighted images and effect of GnRH analogue. J Obstet Gynaecol (Tokyo 1995). 1995. 21:107–117.6. Takahashi K, Okada M, Imaoka I, Sugimura K, Miyazaki K. Value of magnetic resonance imaging in predicting efficacy of GnRH analogue treatment for uterine leiomyoma. Hum Reprod. 2001. 16:1989–1994.7. Harman M, Zeteroğlu S, Arslan H, Sengül M, Etlik O. Predictive value of magnetic resonance imaging signal and contrast-enhancement characteristics on post-embolization volume reduction of uterine fibroids. Acta Radiol. 2006. 47:427–435.8. Swe TT, Onitsuka H, Kawamoto K, Ueyama T, Tsuruchi N, Masuda K. Uterine leiomyoma: correlation between signal intensity on magnetic resonance imaging and pathologic characteristics. Radiat Med. 1992. 10:235–242.9. Murase E, Siegelman ES, Outwater EK, Perez-Jaffe LA, Tureck RW. Uterine leiomyomas: histopathologic features, MR imaging findings, differential diagnosis, and treatment. Radiographics. 1999. 19:1179–1197.10. Burn PR, McCall JM, Chinn RJ, Vashisht A, Smith JR, Healy JC. Uterine fibroleiomyoma: MR imaging appearances before and after embolization of uterine arteries. Radiology. 2000. 214:729–734.11. Orsini LF, Salardi S, Pilu G, Bovicelli L, Cacciari E. Pelvic organs in premenarcheal girls: real-time ultrasonography. Radiology. 1984. 153:113–116.12. Spies JB, Spector A, Roth AR, Baker CM, Mauro L, Murphy-Skrynarz K. Complications after uterine artery embolization for leiomyomas. Obstet Gynecol. 2002. 100(5 Pt 1):873–880.13. Goodwin SC, Bonilla SM, Sacks D, Reed RA, Spies JB, Landow WJ, et al. Reporting standards for uterine artery embolization for the treatment of uterine leiomyomata. J Vasc Interv Radiol. 2001. 12:1011–1020.14. Yamashiro T, Gibo M, Utsunomiya T, Murayama S. Huge uterine leiomyoma with adenomyotic cysts mimicking uterine sarcoma on MR imaging. Radiat Med. 2007. 25:127–129.15. Hamlin DJ, Pettersson H, Fitzsimmons J, Morgan LS. MR imaging of uterine leiomyomas and their complications. J Comput Assist Tomogr. 1985. 9:902–907.16. Ueda H, Togashi K, Konishi I, Kataoka ML, Koyama T, Fujiwara T, et al. Unusual appearances of uterine leiomyomas: MR imaging findings and their histopathologic backgrounds. Radiographics. 1999. 19 Spec No:S131–S145.17. Rajan DK, Margau R, Kroll RR, Simons ME, Tan KT, Jaskolka JD, et al. Clinical utility of ultrasound versus magnetic resonance imaging for deciding to proceed with uterine artery embolization for presumed symptomatic fibroids. Clin Radiol. 2011. 66:57–62.18. deSouza NM, Williams AD. Uterine arterial embolization for leiomyomas: perfusion and volume changes at MR imaging and relation to clinical outcome. Radiology. 2002. 222:367–374.19. Hecht EM, Do RK, Kang SK, Bennett GL, Babb JS, Clark TW. Diffusion-weighted imaging for prediction of volumetric response of leiomyomas following uterine artery embolization: a preliminary study. J Magn Reson Imaging. 2011. 33:641–646.20. Jain TP, Srivastava DN, Sahu RP, Thulkar S, Sharma S, Mittal S, et al. Uterine artery embolization for symptomatic fibroids with imaging follow up. Australas Radiol. 2007. 51:246–252.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Uterine Fibroids Necrosis after Transarterial Embolization for Treatment of Uterine Fibroids
- A Case of Vaginal Expulsion of Submucosal Fibroid after Uterine Artery Embolization
- Brodie's Abscess : MR Findings
- Differential Diagnosis of Bicornuate and Septate Uterus : Is Comparison of Septal Signal Intensity on MR Image Useful?
- Usefulness of Breath-hold T2-w d T2-weighted MR Imaging in Patients with Myocardial Infarction: Comparison with Delayed Enhancement