Korean J Radiol.
2012 Oct;13(5):602-609. 10.3348/kjr.2012.13.5.602.
Determination of Optimal Imaging Mode for Ultrasonographic Detection of Subdermal Contraceptive Rods: Comparison of Spatial Compound, Conventional, and Tissue Harmonic Imaging Methods
- Affiliations
-
- 1Department of Radiology, Gangnam Severance Hospital, Yonsei University College of Medicine, Seoul 135-720, Korea. yooncs58@yuhs.ac
- 2Department of Obstetrics and Gynecology, Gangnam Severance Hospital, Yonsei University College of Medicine, Seoul 135-720, Korea.
- 3Department of Radiology and Research Institute of Radiological Science, Severance Hospital, Yonsei University College of Medicine, Seoul 120-752, Korea.
- 4Department of Radiology, Guri Hospital, Hanyang University College of Medicine, Guri 471-701, Korea.
- 5Department of Radiology, Hanyang University Hospital, Hanyang University College of Medicine, Seoul 133-792, Korea.
- KMID: 1392939
- DOI: http://doi.org/10.3348/kjr.2012.13.5.602
Abstract
OBJECTIVE
To determine which mode of ultrasonography (US), among the conventional, spatial compound, and tissue-harmonic methods, exhibits the best performance for the detection of Implanon(R) with respect to generation of posterior acoustic shadowing (PAS).
MATERIALS AND METHODS
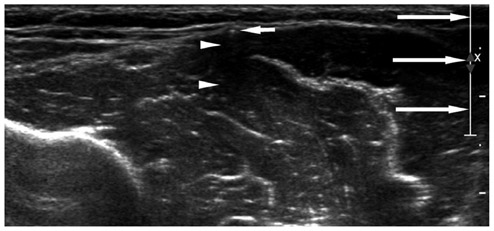
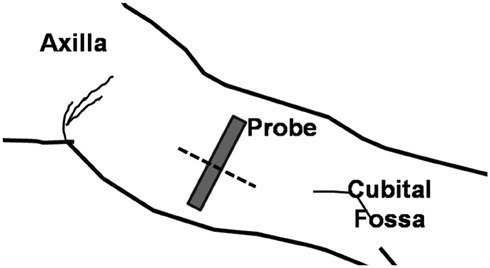
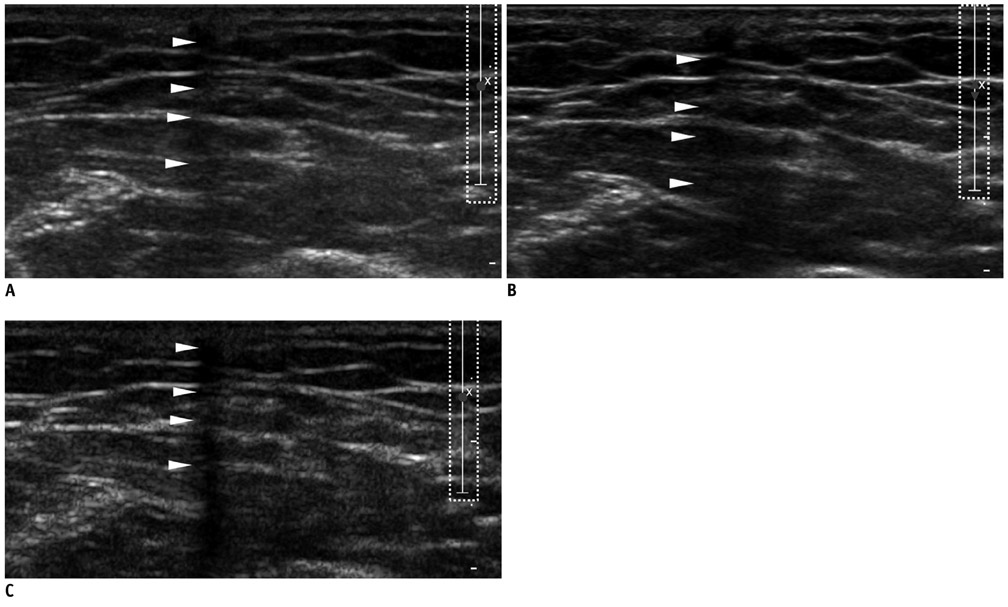
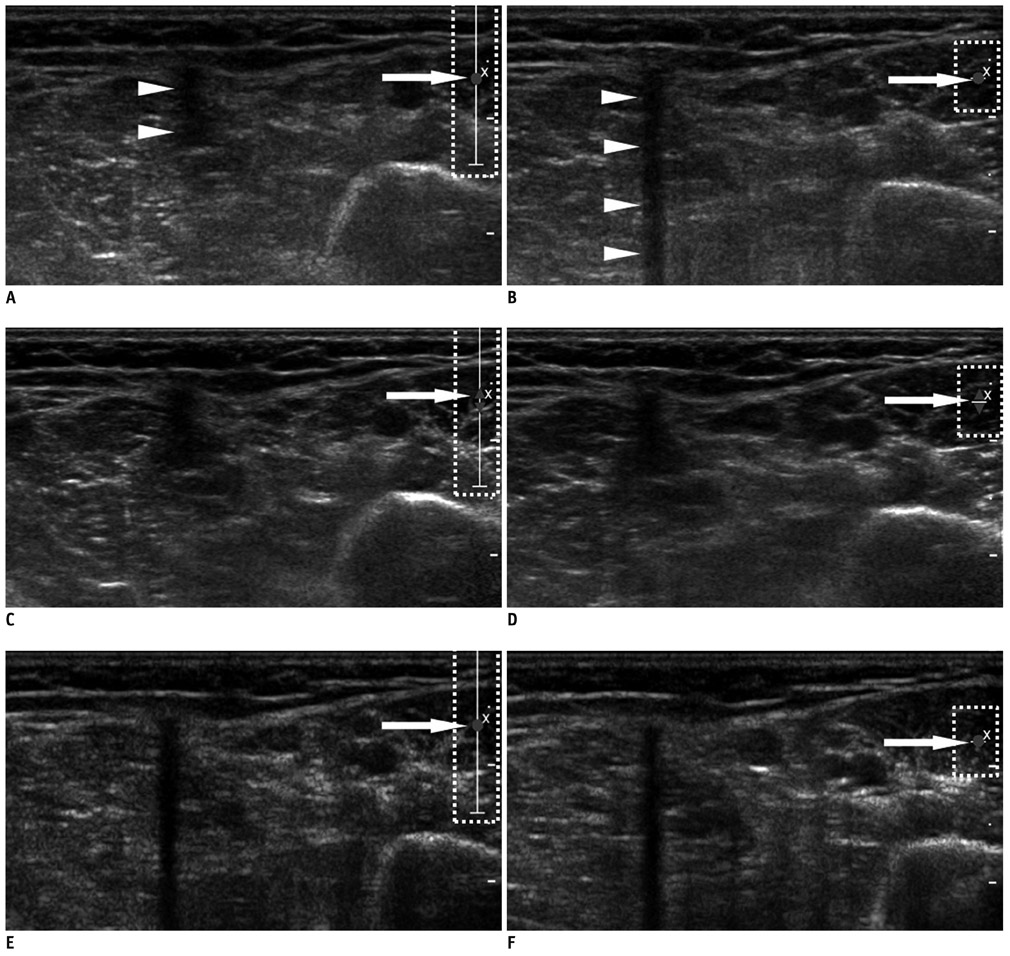
A total of 21 patients, referred for localization of impalpable Implanon(R), underwent US, using the three modes with default settings (i.e., wide focal zone). Representative transverse images of the rods, according to each mode for all patients, were obtained. The resulting 63 images were reviewed by four observers. The observers provided a confidence score for the presence of PAS, using a five-point scale ranging from 1 (definitely absent) to 5 (definitely present), with scores of 4 or 5 for PAS being considered as detection. The average scores of PAS, obtained from the three different modes for each observer, were compared using one-way repeated measure ANOVA. The detection rates were compared using a weighted least square method.
RESULTS
Statistically, the tissue harmonic mode was significantly superior to the other two modes, when comparing the average scores of PAS for all observers (p < 0.00-1). The detection rate was also highest for the tissue harmonic mode (p < 0.001).
CONCLUSION
Tissue harmonic mode in uS appears to be the most suitable in detecting subdermal contraceptive implant rods.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Experiences of localization and removal of non-palpable subdermal contraceptive implants with ultrasound
SooHyun Kim, Young Sik Choi, Jeong Sook Kim, Sungjun Kim, SiHyun Cho
Obstet Gynecol Sci. 2019;62(3):166-172. doi: 10.5468/ogs.2019.62.3.166.
Reference
-
1. Shulman LP, Gabriel H. Management and localization strategies for the nonpalpable Implanon rod. Contraception. 2006. 73:325–330.2. Mascarenhas L. Insertion and removal of Implanon. Contraception. 1998. 58:6 Suppl. 79S–83S.3. James P, Trenery J. Ultrasound localisation and removal of non-palpable Implanon implants. Aust N Z J Obstet Gynaecol. 2006. 46:225–228.4. Persaud T, Walling M, Geoghegan T, Buckley O, Stunell H, Torreggiani WC. Ultrasound-guided removal of Implanon devices. Eur Radiol. 2008. 18:2582–2585.5. McNeill G, Ward E, Halpenny D, Snow A, Torreggiani W. Ultrasound appearances of Implanon implanted contraceptive devices. JBR-BTR. 2009. 92:259–260.6. Horton LK, Jacobson JA, Powell A, Fessell DP, Hayes CW. Sonography and radiography of soft-tissue foreign bodies. AJR Am J Roentgenol. 2001. 176:1155–1159.7. Young AS, Shiels WE 2nd, Murakami JW, Coley BD, Hogan MJ. Self-embedding behavior: radiologic management of self-inserted soft-tissue foreign bodies. Radiology. 2010. 257:233–239.8. Gabriel H, Shulman L, Marko J, Nikolaidis P, Chirita V. Compound versus fundamental imaging in the detection of subdermal contraceptive implants. J Ultrasound Med. 2007. 26:355–359.9. Westerway SC, Picker R, Christie J. Implanon implant detection with ultrasound and magnetic resonance imaging. Aust N Z J Obstet Gynaecol. 2003. 43:346–350.10. Gönen M, Panageas KS, Larson SM. Statistical issues in analysis of diagnostic imaging experiments with multiple observations per patient. Radiology. 2001. 221:763–767.11. Agresti A. Categorical data analysis. 2002. Hoboken: John Wiley & Sons;481–629.12. Stokes ME, Davis CS, Koch GG. Categorical Data Analysis Using the SAS System. 2000. 2nd ed. Cary: SAS Institute Inc.;430–437.13. Hangiandreou NJ. AAPM/RSNA physics tutorial for residents. Topics in US: B-mode US: basic concepts and new technology. Radiographics. 2003. 23:1019–1033.14. Comstock C. Bassett LW, Mahoney MC, Apple SK, D'Orsi CJ, editors. Ultrasound Equipment. Breast Imaging. 2011. 1st ed. Philadelphia: Elsevier;146–152.15. Piessens SG, Palmer DC, Sampson AJ. Ultrasound localisation of non-palpable Implanon. Aust N Z J Obstet Gynaecol. 2005. 45:112–116.16. Lieu D. Ultrasound physics and instrumentation for pathologists. Arch Pathol Lab Med. 2010. 134:1541–1556.17. Desser TS, Jeffrey RB. Tissue harmonic imaging techniques: physical principles and clinical applications. Semin Ultrasound CT MR. 2001. 22:1–10.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- High Resolution Ultrasonographic Evaluation of the Gallbladder: Value of Advanced Imaging Techniques
- Ultrasonographic Evaluation of the Normal Kidney: Comparison of Fundamental, Tissue Harmonic, and Pulse Inversion Harmonic Imaging
- Ultrasonographic Evaluation of Focal Hepatic Lesions : Comparison of Fundamental, Tissue Harmonic, Fundamental Compound and Harmonic Compound Imaging Techniques
- Sonographic Evaluation of Breast Nodules: Comparison of Conventional, Real-Time Compound, and Pulse-Inversion Harmonic Images
- Migration of a contraceptive subdermal device into the lung