Korean J Gastroenterol.
2012 Sep;60(3):172-176. 10.4166/kjg.2012.60.3.172.
Intestinal Amyloidosis with Intractable Diarrhea and Intestinal Pseudo-obstruction
- Affiliations
-
- 1Department of Internal Medicine, Chonnam National University Medical School, Gwangju, Korea. dshskim@jnu.ac.kr
- 2Department of Pathology, Chonnam National University Medical School, Gwangju, Korea.
- KMID: 1389726
- DOI: http://doi.org/10.4166/kjg.2012.60.3.172
Abstract
- We report herein a case of intestinal amyloidosis with grave prognosis that caused intractable diarrhea and intestinal pseudo-obstruction, alternately in spite of intensive conservative treatment. A 44-year-old woman was admitted for fever, diarrhea, and crampy abdominal pain which had been continuned during 6 months. Abdomen CT scan showed edematous wall thickening of the small bowel and right colon, and colonoscopic biopsy revealed amyloid deposition in the mucosa. Monoclonal light chains in serum and/or urine were not detected and highly elevated serum amyloid A was shown. In spite of intensive treatment including oral prednisolone and colchicine, diarrhea and intestinal pseudo-obstruction developed alternately, general status rapidly got worsened and died after two months.
Keyword
MeSH Terms
-
Administration, Oral
Adult
Amyloidosis/complications/*diagnosis/drug therapy
Anti-Inflammatory Agents/therapeutic use
Colchicine/therapeutic use
Colonoscopy
Diarrhea/*etiology
Female
Humans
Intestinal Mucosa/pathology
Intestinal Pseudo-Obstruction/*diagnosis/etiology
Prednisolone/therapeutic use
Serum Amyloid A Protein/metabolism
Tomography, X-Ray Computed
Tubulin Modulators/therapeutic use
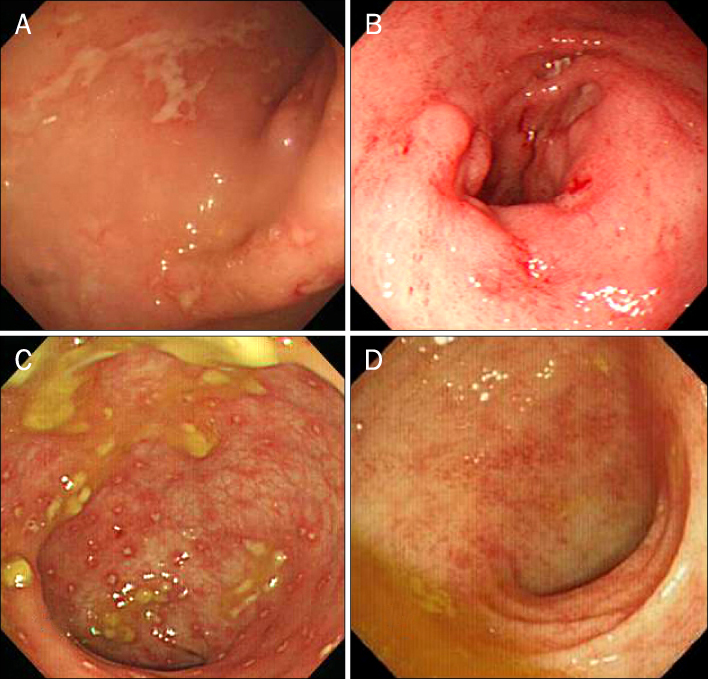
Figure
Cited by 1 articles
-
A Case of Primary Gastric Amyloidosis with Fulminant Heart Failure
Seonghun Hong, Young-Woon Chang, Jong Kyu Byun, Min Je Kim, Jung Min Chae, Sun Hee Park, Chi Hyuk Oh, Yong-Koo Park
Korean J Gastroenterol. 2015;66(4):227-230. doi: 10.4166/kjg.2015.66.4.227.
Reference
-
1. Kala Z, Válek V, Kysela P. Amyloidosis of the small intestine. Eur J Radiol. 2007. 63:105–109.2. Fonnesu C, Giovinale M, Verrecchia E, et al. Gastrointestinal amyloidosis: a case of chronic diarrhoea. Eur Rev Med Pharmacol Sci. 2009. 13:Suppl 1. 45–50.3. Westermark P. Aspects on human amyloid forms and their fibril polypeptides. FEBS J. 2005. 272:5942–5949.4. Levine RA. Amyloid disease of the liver. Correlation of clinical, functional and morphologic features in forty-seven patients. Am J Med. 1962. 33:349–357.5. Naiki H, Nagai Y. Molecular pathogenesis of protein misfolding diseases: pathological molecular environments versus quality control systems against misfolded proteins. J Biochem. 2009. 146:751–756.6. Ebert EC, Nagar M. Gastrointestinal manifestations of amyloidosis. Am J Gastroenterol. 2008. 103:776–787.7. Röcken C, Shakespeare A. Pathology, diagnosis and pathogenesis of AA amyloidosis. Virchows Arch. 2002. 440:111–122.8. Okuda Y, Takasugi K, Oyama T, Oyama H, Nanba S, Miyamoto T. Intractable diarrhoea associated with secondary amyloidosis in rheumatoid arthritis. Ann Rheum Dis. 1997. 56:535–541.9. Fushimi T, Takahashi Y, Kashima Y, et al. Severe protein losing enteropathy with intractable diarrhea due to systemic AA amyloidosis, successfully treated with corticosteroid and octreotide. Amyloid. 2005. 12:48–53.10. Cathcart ES. Kelley WN, Harris ED, Ruddy S, Sledge CB, editors. Amyloidosis. Textbook of rheumatology. 1993. Philadelphia: W.B. Saunders Company;1413–1428.11. Feurle GE. Pathophysiology of diarrhea in patients with familial amyloid neuropathy. Digestion. 1987. 36:13–17.12. Hiramatsu K, Kaneko S, Shirota Y, et al. Gastrointestinal amyloidosis secondary to hypersensitivity vasculitis presenting with intestinal pseudoobstruction. Dig Dis Sci. 1998. 43:1824–1830.13. Braunstein JM, Aman A, Warman J. Colonic amyloidosis. Clin Gastroenterol Hepatol. 2007. 5:A30.14. Yamada M, Hatakeyama S, Tsukagoshi H. Gastrointestinal amyloid deposition in AL (primary or myeloma-associated) and AA (secondary) amyloidosis: diagnostic value of gastric biopsy. Hum Pathol. 1985. 16:1206–1211.15. Legge DA, Carlson HC, Wollaeger EE. Roentgenologic appearance of systemic amyloidosis involving gastrointestinal tract. Am J Roentgenol Radium Ther Nucl Med. 1970. 110:406–412.16. Kim SH, Han JK, Lee KH, et al. Abdominal amyloidosis: spectrum of radiological findings. Clin Radiol. 2003. 58:610–620.17. Schroeder FM, Miller FJ Jr, Nelson JA, Rankin RS. Gastrointestinal angiographic findings in systemic amyloidosis. AJR Am J Roentgenol. 1978. 131:143–146.18. Tada S, Iida M, Yao T, et al. Endoscopic features in amyloidosis of the small intestine: clinical and morphologic differences between chemical types of amyloid protein. Gastrointest Endosc. 1994. 40:45–50.19. Michael H, Brandt LJ, Tanaka KE, Berkowitz D, Cardillo M, Weidenheim K. Congo-red negative colonic amyloid with scalloping of the valvulae conniventes. Gastrointest Endosc. 2001. 53:653–655.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Megacystis Associated with Primary Chronic Intestinal Pseudoobstruction
- Chronic Idiopathic Intestinal Pseudo-obstruction in Adult: A Case Report with a Clinical Analysis of Other Reported Cases in Korean Literature
- Pseudo-Obstruction of Jejunum due to AA Amyloidosis Associated with Latent Syphilis
- A case of chronic intestinal pseudo-obstruction syndrome
- Acute Intestinal Pseudo-Obstruction in a Patient with MELAS Syndrome