Korean J Radiol.
2008 Oct;9(5):409-415. 10.3348/kjr.2008.9.5.409.
Ankle MRI for Anterolateral Soft Tissue Impingement: Increased Accuracy with the Use of Contrast-Enhanced Fat-Suppressed 3D-FSPGR MRI
- Affiliations
-
- 1Department of Radiology and Research Institute of Radiological Science, College of Medicine, Yonsei University, Seoul, Korea. jss@yuhs.ac
- 2Department of Radiology, College of Medicine, Inje University, Busan, Korea.
- 3Department of Orthopedic Surgery, Yonsei University, College of Medicine, Seoul, Korea.
- KMID: 1385398
- DOI: http://doi.org/10.3348/kjr.2008.9.5.409
Abstract
OBJECTIVE
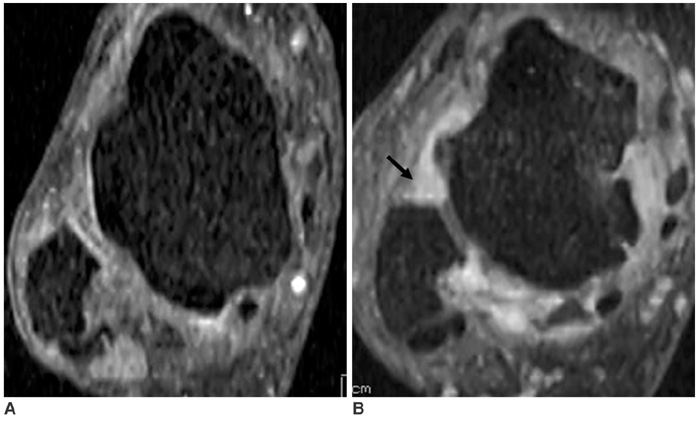
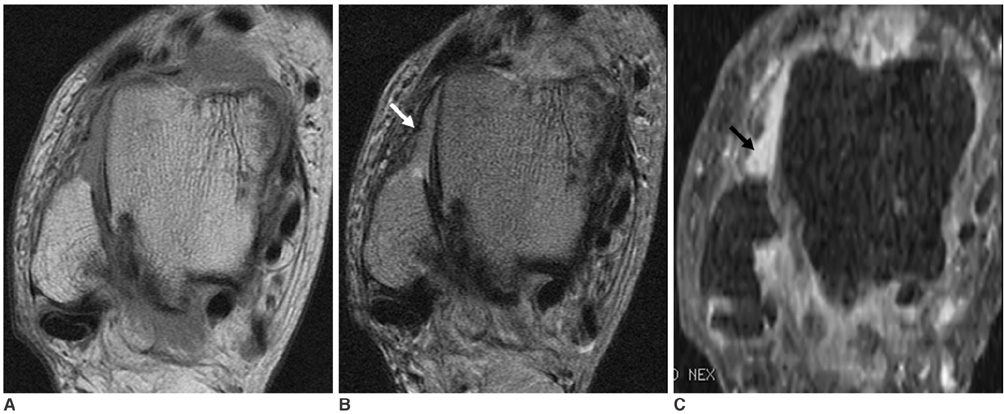
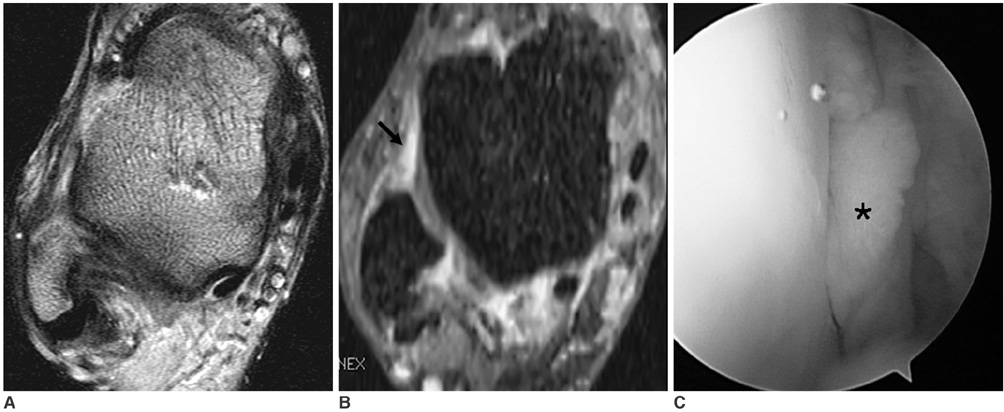
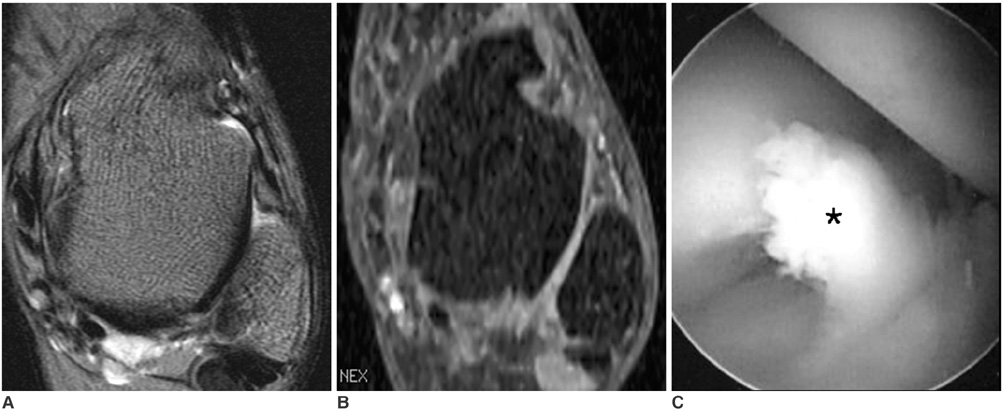
To validate the use of contrast-enhanced (CE) fat-suppressed three-dimensional (3D) fast gradient-recalled acquisition in the steady state with radiofrequency spoiling (FSPGR) magnetic resonance imaging (MRI) for the diagnosis of anterolateral soft tissue impingement of the ankle, as compared to the use of routine ankle MRI. MATERIALS AND METHODS: Contrast-enhanced fat-suppressed 3D-FSPGR MRI and routine MRI scans were retrospectively reviewed for 45 patients with arthroscopically proven anterolateral impingement. In addition, scans were reviewed in 45 control subjects with diagnoses other than impingement. Two radiologists independently reviewed the two sets of images in random order. Using areas (Az) under the receiver operating characteristic curve (ROC), we compared the depiction of anterolateral soft tissue impingement in the two sets of images. RESULTS: The overall accuracy for lesion characterization was significantly higher (p < 0.05) using the CE fat-suppressed 3D-FSPGR MR images (Az = 0.892 and 0.881 for reader 1 and 2, respectively) than using the routine MR images (Az = 0.763 and 0.745). The use of CE fat-suppressed 3D-FSPGR MRI enhanced impingement depiction in most cases. However, in cases with a thickened non-enhancing scar or joint effusion, the routine images better depicted a soft tissue mass that intruded into anterolateral gutter than the CE images. CONCLUSION: The use of CE fat-suppressed 3D-FSPGR MRI of the ankle allows a more accurate assessment of anterolateral soft tissue impingement of the ankle, as compared to the use of routine MRI.
Keyword
MeSH Terms
-
Adolescent
Adult
Aged
Ankle Joint/*pathology
Contrast Media
Female
Gadolinium DTPA/diagnostic use
Humans
Image Interpretation, Computer-Assisted
Imaging, Three-Dimensional
Joint Diseases/*diagnosis
Magnetic Resonance Imaging/*methods
Male
Middle Aged
ROC Curve
Retrospective Studies
Sensitivity and Specificity
Statistics, Nonparametric
Figure
Reference
-
1. Kim SH, Ha KI. Arthroscopic treatment for impingement of the anterolateral soft tissues of the ankle. J Bone Joint Surg Br. 2000. 82:1019–1021.2. Ferkel RD, Karzel RP, Del Pizzo W, Friedman MJ, Fischer SP. Arthroscopic treatment of anterolateral impingement of the ankle. Am J Sports Med. 1991. 19:440–446.3. Martin DF, Curl WW, Baker CL. Arthroscopic treatment of chronic synovitis of the ankle. Arthroscopy. 1989. 5:110–114.4. Meislin RJ, Rose DJ, Parisien JS, Springer S. Arthroscopic treatment of synovial impingement of the ankle. Am J Sports Med. 1993. 21:186–189.5. Liu SH, Raskin A, Osti L, Baker C, Jacobson K, Finerman G, et al. Arthroscopic treatment of anterolateral ankle impingement. Arthroscopy. 1994. 10:215–218.6. Thein R, Eichenblat M. Arthroscopic treatment of sports-related synovitis of the ankle. Am J Sports Med. 1992. 20:496–498.7. McCarroll JR, Schrader JW, Shelbourne KD, Rettig AC, Bisesi MA. Meniscoid lesions of the ankle in soccer players. Am J Sports Med. 1987. 15:255–257.8. Robinson P, White LM, Salonen DC, Daniels TR, Ogilvie-Harris D. Anterolateral ankle impingement: MR arthrographic assessment of the anterolateral recess. Radiology. 2001. 221:186–190.9. Robinson P, White LM. Soft-tissue and osseous impingement syndromes of the ankle: role of imaging in diagnosis and management. Radiographics. 2002. 22:1457–1471.10. Cerezal L, Abascal F, Canga A, Pereda T, Garcia-Valtuille R, Perez-Carro L, et al. MR imaging of ankle impingement syndromes. AJR Am J Roentgenol. 2003. 181:551–559.11. Rubin DA, Tishkoff NW, Britton CA, Conti SF, Towers JD. Anterolateral soft tissue impingement in the ankle: Diagnosis using MR imaging. AJR Am J Roentgenol. 1997. 169:829–835.12. Liu SH, Nuccion SL, Finerman G. Diagnosis of anterolateral ankle impingement. Am J Sports Med. 1997. 25:389–393.13. Farooki S, Yao L, Seeger LL. Anterolateral impingement of the ankle: effectiveness of MR imaging. Radiology. 1998. 207:357–360.14. Jordan LK 3rd, Helms CA, Cooperman AE, Speer KP. Magnetic resonance imaging findings in anterolateral impingement of the ankle. Skeletal Radiol. 2000. 29:34–39.15. Huh YM, Suh JS, Lee JW, Song HT. Synovitis and soft tissue impingement of the ankle: assessment with enhanced three-dimensional FSPGR MR imaging. J Magn Reson Imaging. 2004. 19:108–116.16. Kundel HL, Polansky M. Measurement of observer agreement. Radiology. 2003. 228:303–308.17. Steinbach LS, Palmer WE, Schweitzer ME. Special focus session. MR arthrography. Radiographics. 2002. 22:1223–1246.18. Li D, Haacke EM, Tarr RW, Venkatesan R, Lin W, Wielopolski P. Magnetic resonance imaging of the brain with gadopentetate dimeglumine-DTPA: comparison of T1-weighted spin-echo and 3D gradient-echo sequences. J Magn Reson Imaging. 1996. 6:415–424.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Anterior Impingement Syndrome of the Ankle
- Arthroscopic Treatment of Anterior Ankle Impingement
- Efficiency of Contrast-Enhanced Fat-Suppressed Proton Density Images for Shoulder MRI: Comparison with Contrast-enhanced Fat-suppressed T1 Weighted Image and Arthroscopy
- Importance of Bone Marrow and Soft Tissue Edema to Improve the Diagnostic Accuracy of Lumbosacral MRI for Transverse Process Fractures and Sacral Fractures
- Ankle Lesions, Associated with Anterior Soft Tissue Impingement