Korean J Radiol.
2012 Jun;13(3):275-282. 10.3348/kjr.2012.13.3.275.
Thyroid Incidentaloma Detected by Time-Resolved Magnetic Resonance Angiography at 3T: Prevalence and Clinical Significance
- Affiliations
-
- 1Department of Radiology, Konkuk University Medical Center, Konkuk University School of Medicine, Seoul 143-914, Korea. mdmoonwj@naver.com
- 2Department of Neurology, Konkuk University Medical Center, Konkuk University School of Medicine, Seoul 143-914, Korea.
- KMID: 1372846
- DOI: http://doi.org/10.3348/kjr.2012.13.3.275
Abstract
OBJECTIVE
To determine the prevalence of thyroid incidentalomas detected by time-resolved magnetic resonance angiography (TRMRA) and to evaluate their clinical significance by using an ultrasonographic (US) and cytologic correlation.
MATERIALS AND METHODS
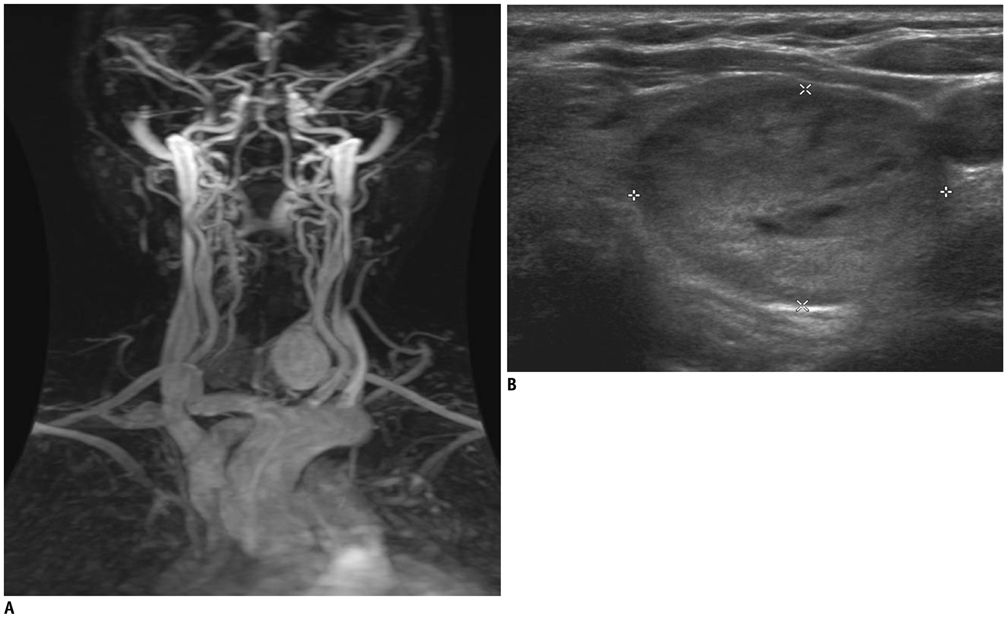
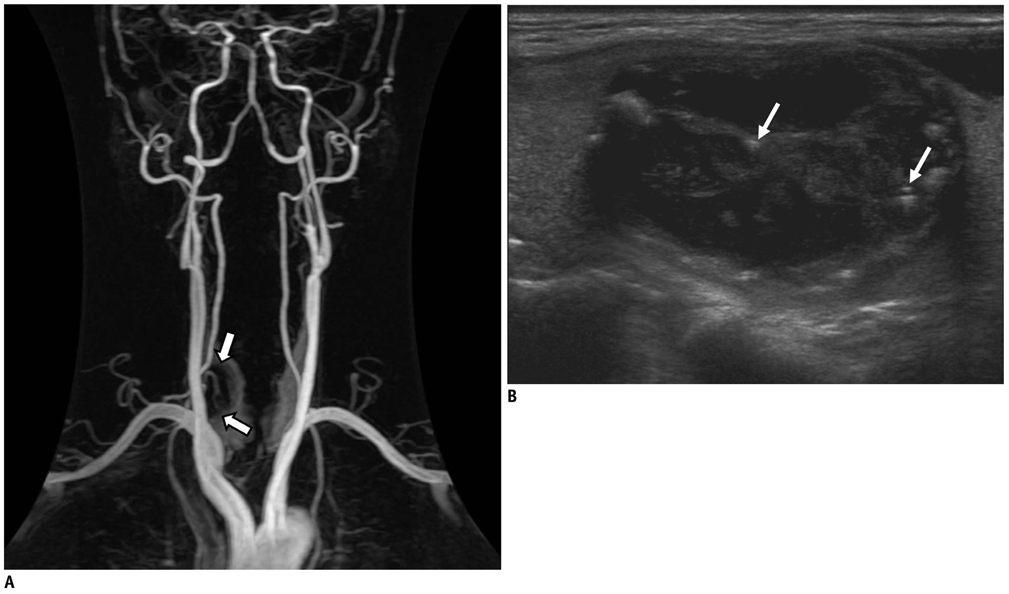
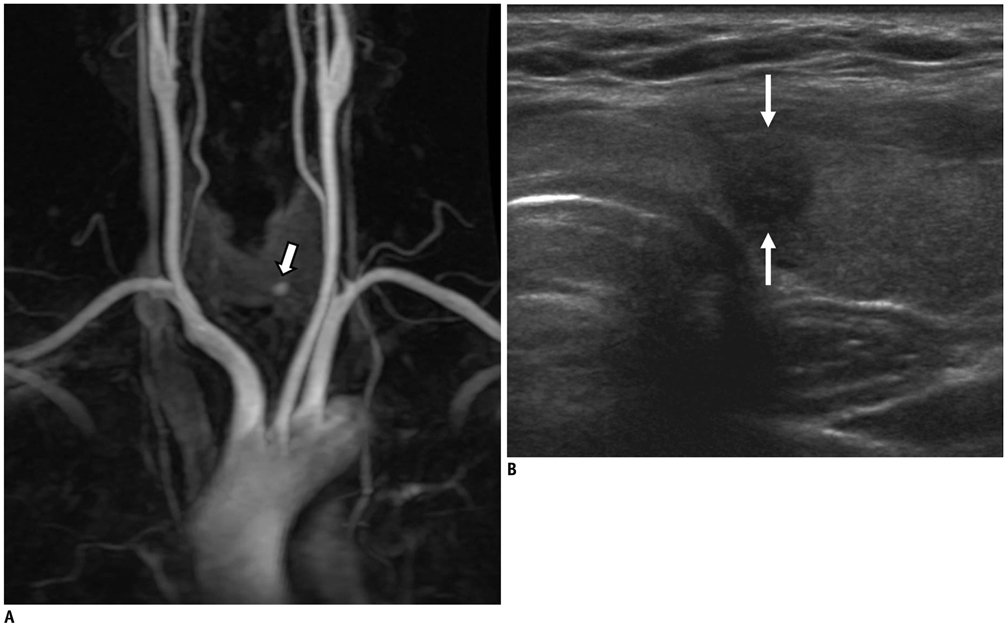
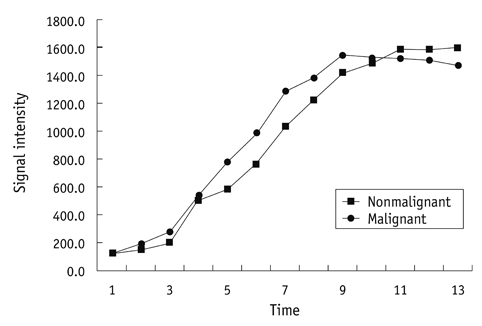
We retrospectively reviewed 2010 consecutive TRMRA examinations performed at our institution between August 2006 and April 2010. The TRMRA findings of thyroid incidentalomas were analyzed according to location, size, as well as vascularity, and were correlated with the US findings and cytologic results. Each nodule was classified as suspiciously malignant, indeterminate or probably benign according to the US criteria recommended by the Korean Society of Thyroid Radiology.
RESULTS
A total of 102 incidentalomas were detected in 90 of 2010 patients (5%). TRMRA showed homogenous hypervascularity in 48 (47%), inhomogeneous hypervascularity in 46 (45%), and hypovascularity in 8 (8%) thyroid nodules. At follow-up study, out of 26 patients with 30 incidentalomas on TRMRA, 27 nodules were identified on US. Of the 27 nodules, 24 (89%) nodule were classified as indeterminate, two (7%) as probably benign, and one (4%) as suspiciously malignant. Among the 16 nodules with available cytopathologic results, 14 (82%) were benign, one (6%) was indeterminate, and one (6%) was malignant.
CONCLUSION
Thyroid incidentalomas are found in 5% of TRMRA examinations. Although their presence does not necessarily indicate malignancy, nonspecific findings of detected incidentalomas on TRMRA require further evaluation by US.
Keyword
MeSH Terms
-
Adult
Aged
Aged, 80 and over
Contrast Media/diagnostic use
Female
Humans
Incidental Findings
Magnetic Resonance Angiography/*methods
Male
Middle Aged
Organometallic Compounds/diagnostic use
Prevalence
Retrospective Studies
Thyroid Neoplasms/*diagnosis/epidemiology/ultrasonography
Thyroid Nodule/*diagnosis/epidemiology/ultrasonography
Figure
Reference
-
1. American Thyroid Association (ATA) Guidelines Taskforce on Thyroid Nodules and Differentiated Thyroid Cancer. Cooper DS, Doherty GM, Haugen BR, Kloos RT, Lee SL, et al. Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid. 2009. 19:1167–1214.2. Lohan DG, Barkhordarian F, Saleh R, Krishnam M, Salamon N, Ruehm SG, et al. MR angiography at 3 T for assessment of the external carotid artery system. AJR Am J Roentgenol. 2007. 189:1088–1094.3. Markl M, Uhl M, Wieben O, Ness T, Langer M, Hennig J, et al. High resolution 3T MRI for the assessment of cervical and superficial cranial arteries in giant cell arteritis. J Magn Reson Imaging. 2006. 24:423–427.4. Nael K, Michaely HJ, Villablanca P, Salamon N, Laub G, Finn JP. Time-resolved contrast enhanced magnetic resonance angiography of the head and neck at 3.0 tesla: initial results. Invest Radiol. 2006. 41:116–112.5. Lohan DG, Tomasian A, Saleh R, Krishnam M, Finn JP. Hypervascular thyroid nodules on time-resolved MR angiography at 3 T: radiologic-pathologic correlation. AJR Am J Roentgenol. 2008. 190:W255–W260.6. Moon WJ, Jung SL, Lee JH, Na DG, Baek JH, Lee YH, et al. Benign and malignant thyroid nodules: US differentiation--multicenter retrospective study. Radiology. 2008. 247:762–770.7. Moon WJ, Baek JH, Jung SL, Kim DW, Kim EK, Kim JY, et al. Ultrasonography and the ultrasound-based management of thyroid nodules: consensus statement and recommendations. Korean J Radiol. 2011. 12:1–14.8. Youserm DM, Huang T, Loevner LA, Langlotz CP. Clinical and economic impact of incidental thyroid lesions found with CT and MR. AJNR Am J Neuroradiol. 1997. 18:1423–1428.9. Yoon DY, Chang SK, Choi CS, Yun EJ, Seo YL, Nam ES, et al. The prevalence and significance of incidental thyroid nodules identified on computed tomography. J Comput Assist Tomogr. 2008. 32:810–815.10. Iyer NG, Shaha AR, Silver CE, Devaney KO, Rinaldo A, Pellitteri PK, et al. Thyroid incidentalomas: to treat or not to treat. Eur Arch Otorhinolaryngol. 2010. 267:1019–1026.11. Ahmed S, Horton KM, Jeffrey RB Jr, Sheth S, Fishman EK. Incidental thyroid nodules on chest CT: Review of the literature and management suggestions. AJR Am J Roentgenol. 2010. 195:1066–1071.12. Chan BK, Desser TS, McDougall IR, Weigel RJ, Jeffrey RB Jr. Common and uncommon sonographic features of papillary thyroid carcinoma. J Ultrasound Med. 2003. 22:1083–1090.13. Papini E, Guglielmi R, Bianchini A, Crescenzi A, Taccogna S, Nardi F, et al. Risk of malignancy in nonpalpable thyroid nodules: predictive value of ultrasound and color-Doppler features. J Clin Endocrinol Metab. 2002. 87:1941–1946.14. Holden A. The role of colour and duplex Doppler ultrasound in the assessment of thyroid nodules. Australas Radiol. 1995. 39:343–349.15. Frates MC, Benson CB, Doubilet PM, Cibas ES, Marqusee E. Can color Doppler sonography aid in the prediction of malignancy of thyroid nodules? J Ultrasound Med. 2003. 22:127–131. quiz 132-134.16. Pacella CM, Guglielmi R, Fabbrini R, Bianchini A, Rinaldi R, Panunzi C, et al. Papillary carcinoma in small hypoechoic thyroid nodules: predictive value of echo color Doppler evaluation. Preliminary results. J Exp Clin Cancer Res. 1998. 17:127–112.17. Iared W, Shigueoka DC, Cristófoli JC, Andriolo R, Atallah AN, Ajzen SA, et al. Use of color Doppler ultrasonography for the prediction of malignancy in follicular thyroid neoplasms: systematic review and meta-analysis. J Ultrasound Med. 2010. 29:419–425.18. Moon HJ, Kwak JY, Kim MJ, Son EJ, Kim EK. Can vascularity at power Doppler US help predict thyroid malignancy? Radiology. 2010. 255:260–269.19. Kusunoki T, Murata K, Nishida S, Tomura T, Inoue M. Histopathological findings of human thyroid tumors and dynamic MRI. Auris Nasus Larynx. 2002. 29:357–360.20. Tezelman S, Giles Y, Tunca F, Gok K, Poyanli A, Salmaslioglu A, et al. Diagnostic value of dynamic contrast medium enhanced magnetic resonance imaging in preoperative detection of thyroid carcinoma. Arch Surg. 2007. 142:1036–1041.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- High field strength magnetic resonance imaging of abdominal diseases
- Introduction to high field strength magnetic resonance imaging
- High field strength magnetic resonance imaging in children
- High field strength magnetic resonance imaging of brain lesion
- New Diagnostic Tool for Far Lateral Lumbar Disc Herniation : The Clinical Usefulness of 3-Tesla Magnetic Resonance Myelography Comparing with the Discography CT