J Korean Rheum Assoc.
2008 Dec;15(4):285-295. 10.4078/jkra.2008.15.4.285.
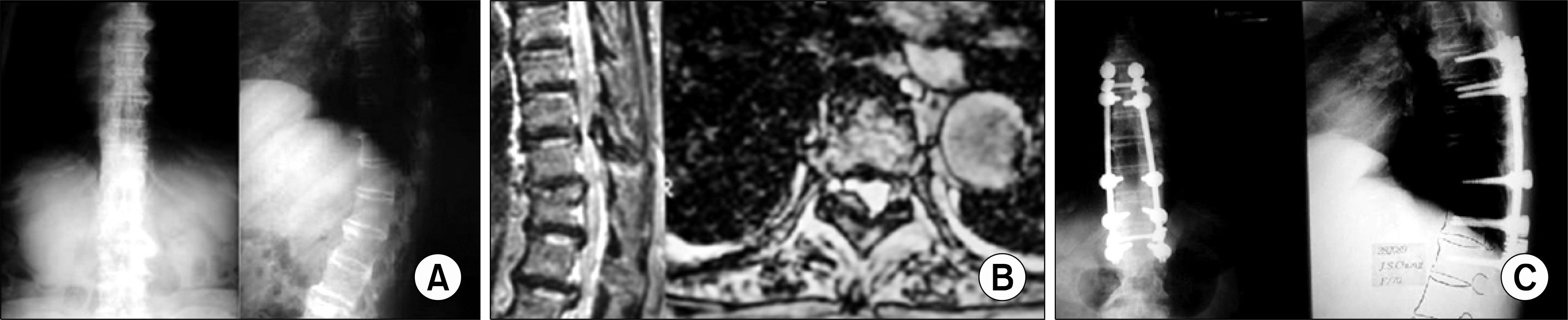
Spinal Diseases and Surgery in Rheumatoid Disorders
- Affiliations
-
- 1Department of Orthopaedic Surgery, Guri Hospital, Hanyang University College of Medicine, Kyunggi-do, Korea. hyparkys@hanyang.ac.kr
- KMID: 1270159
- DOI: http://doi.org/10.4078/jkra.2008.15.4.285
Abstract
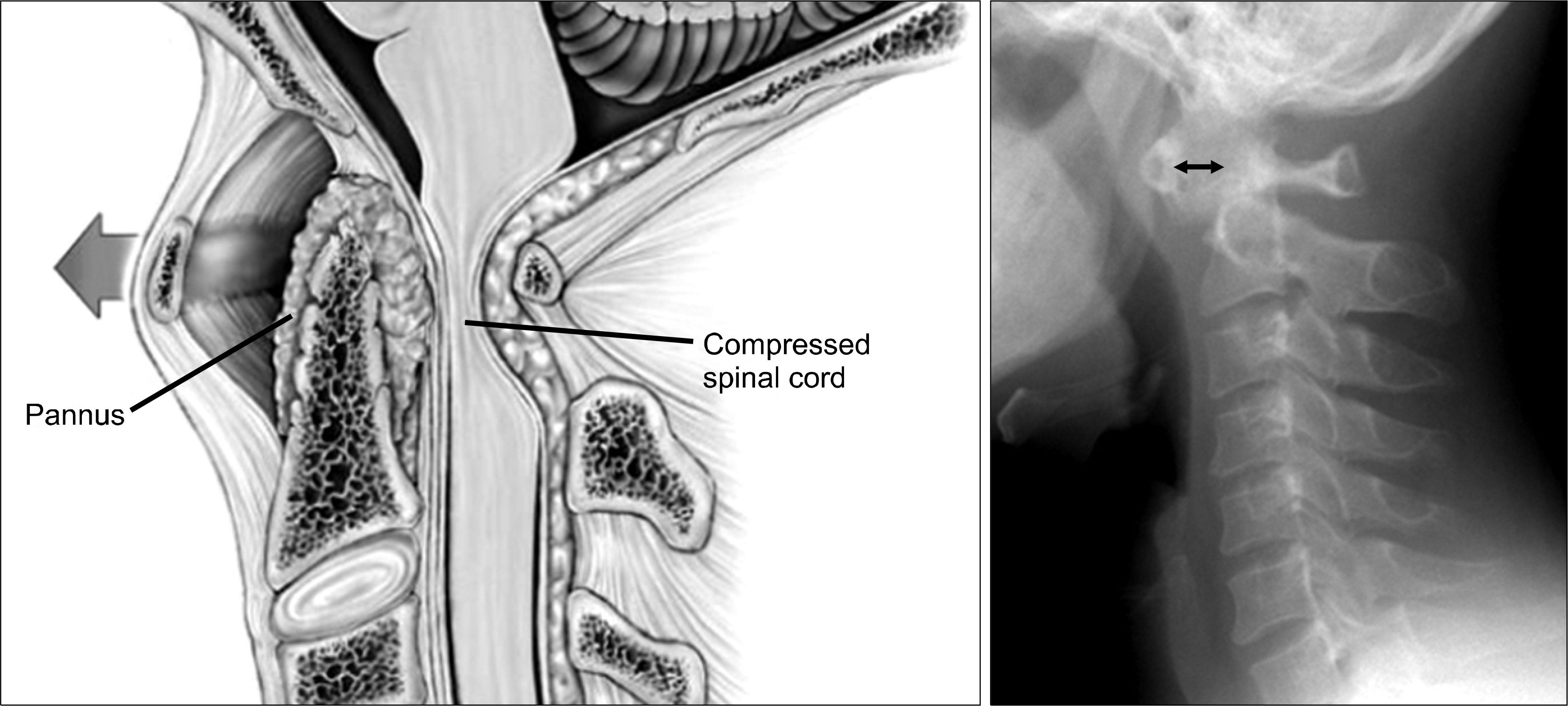
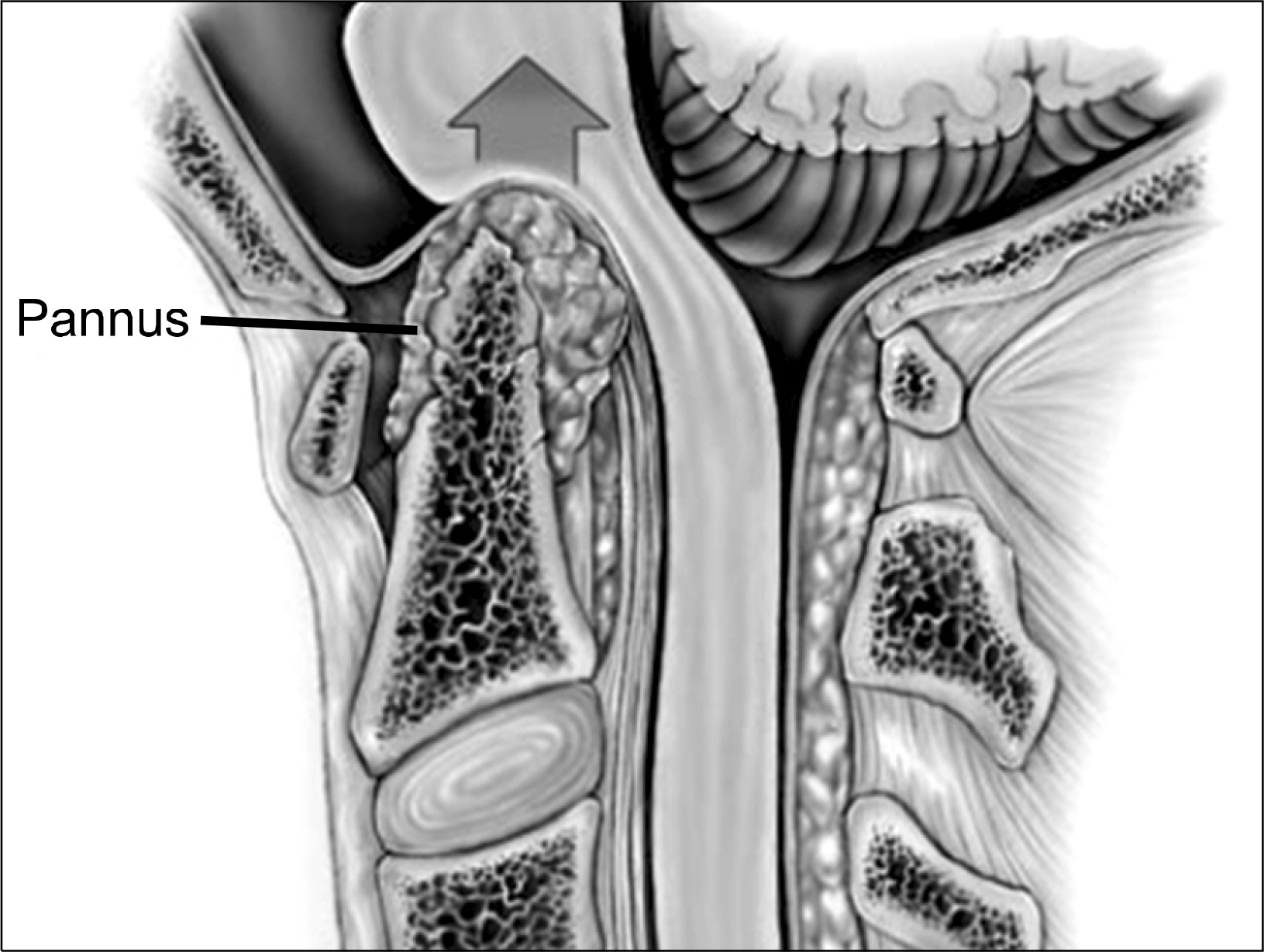
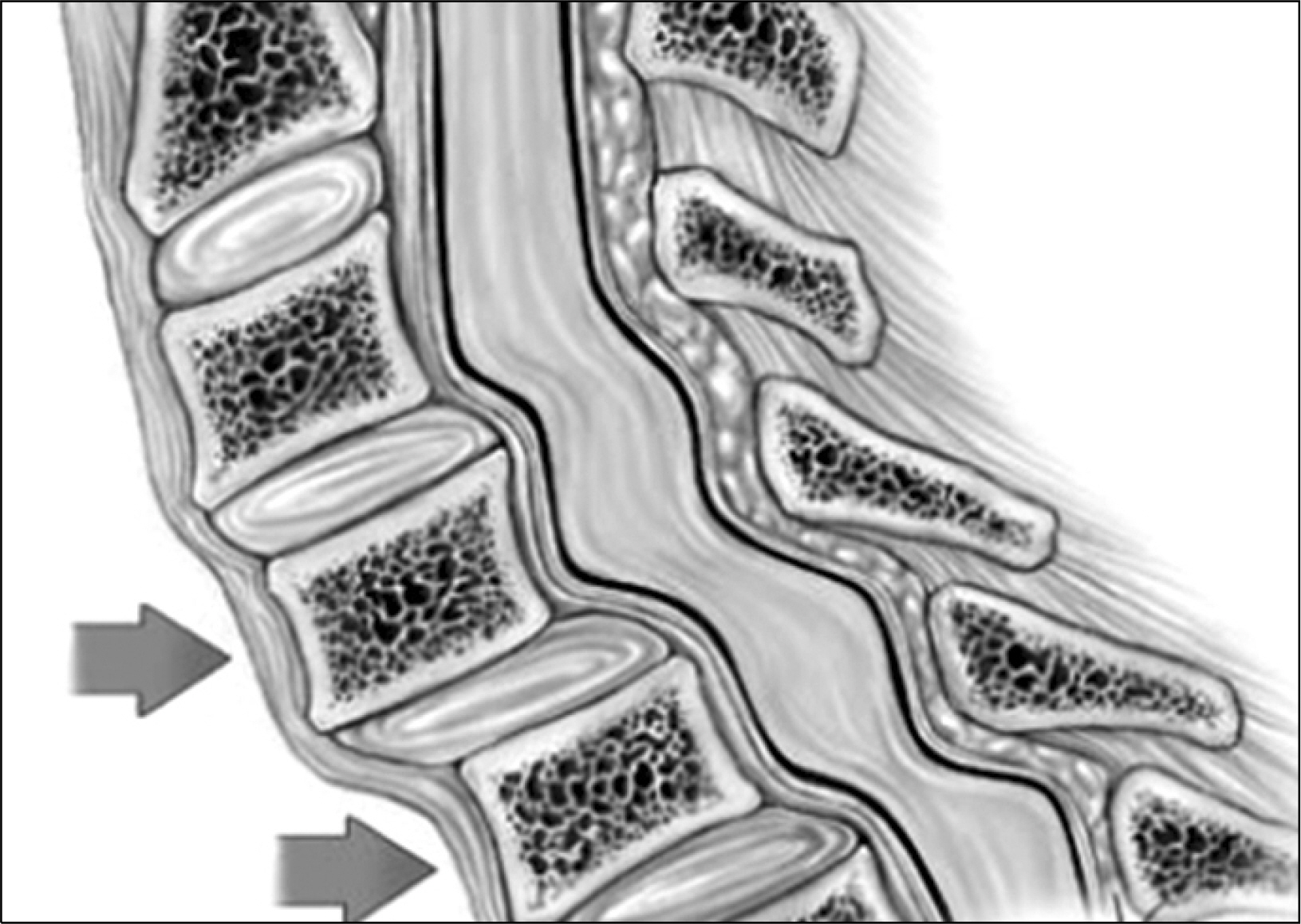
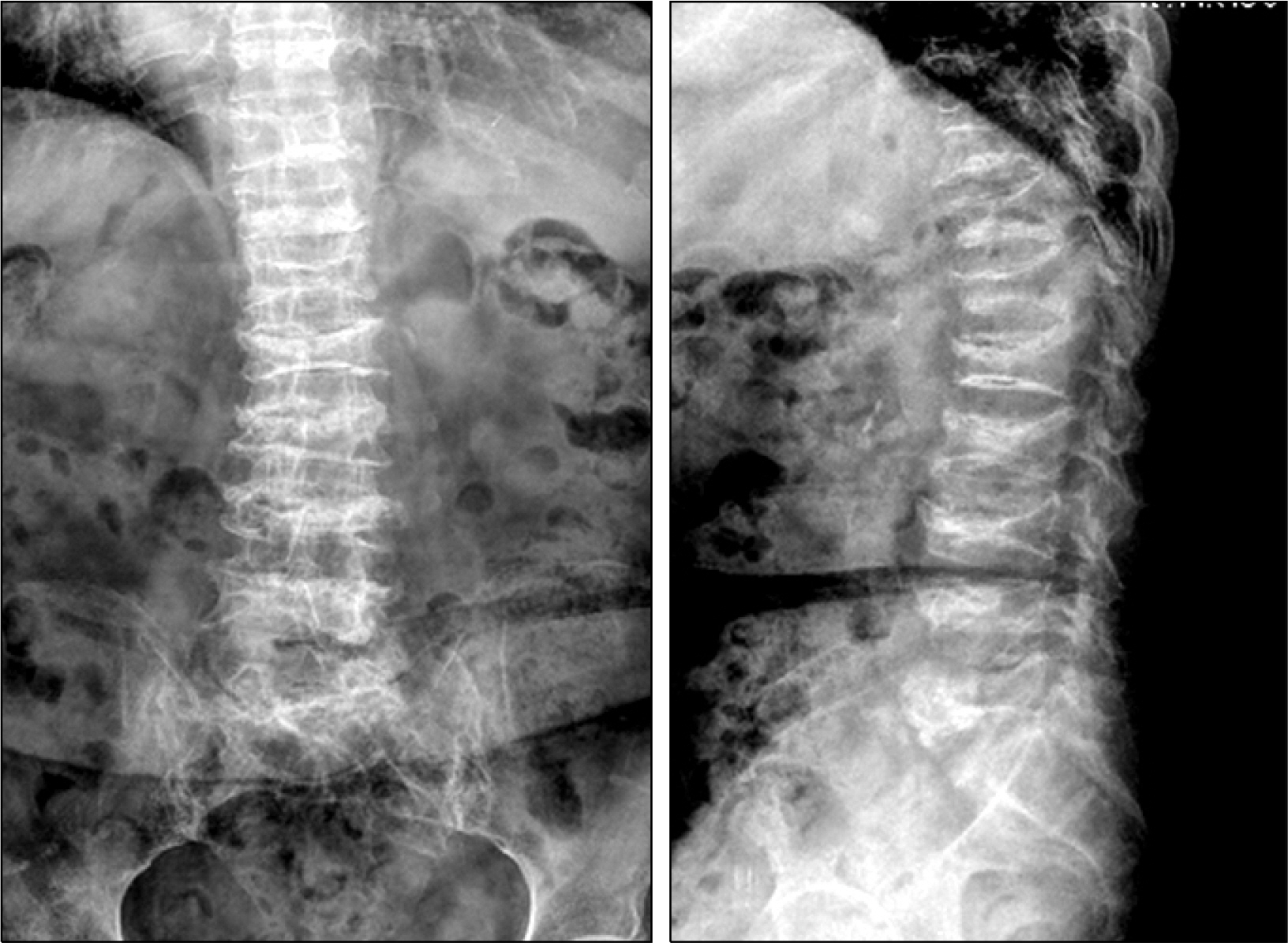
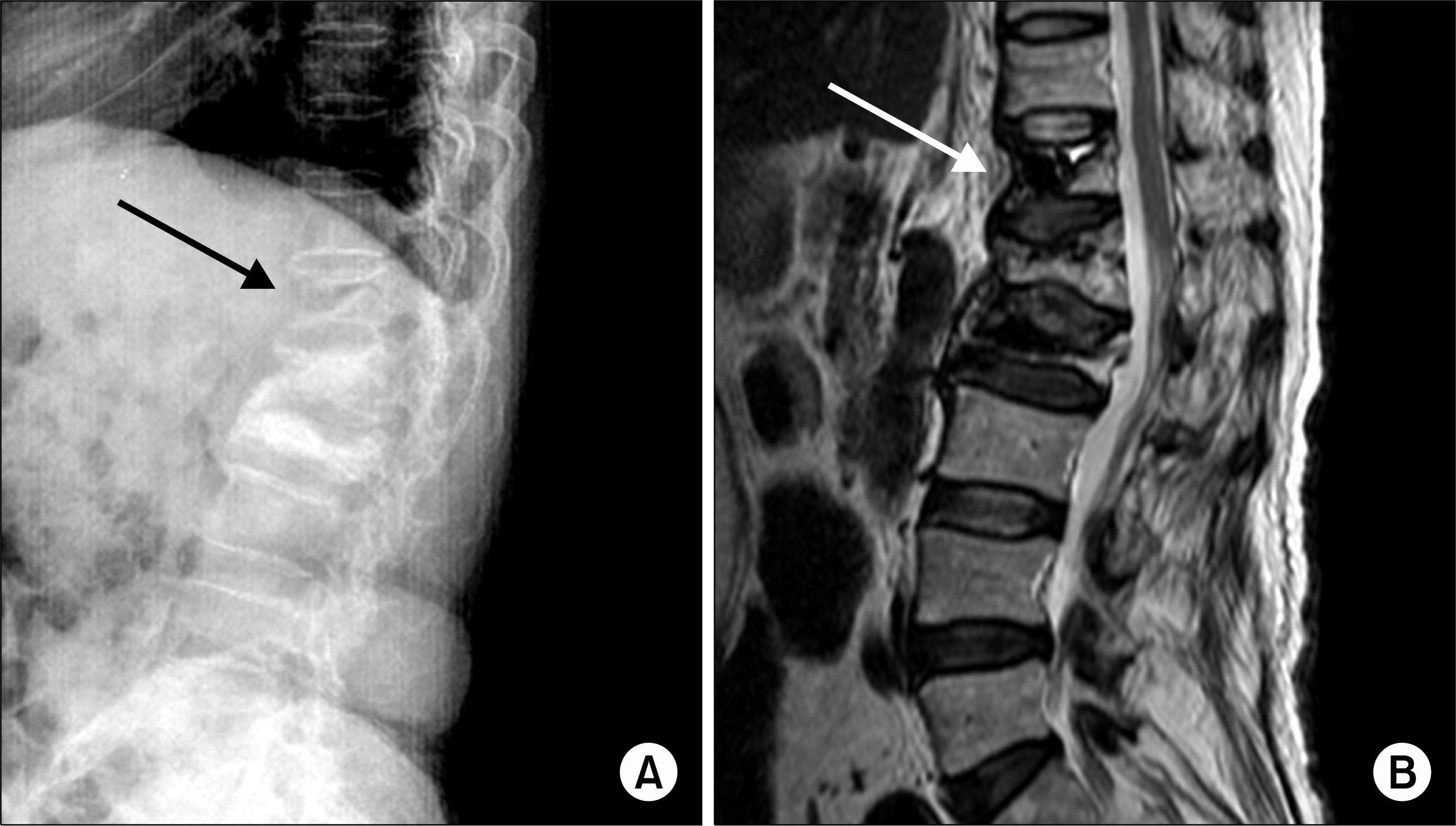
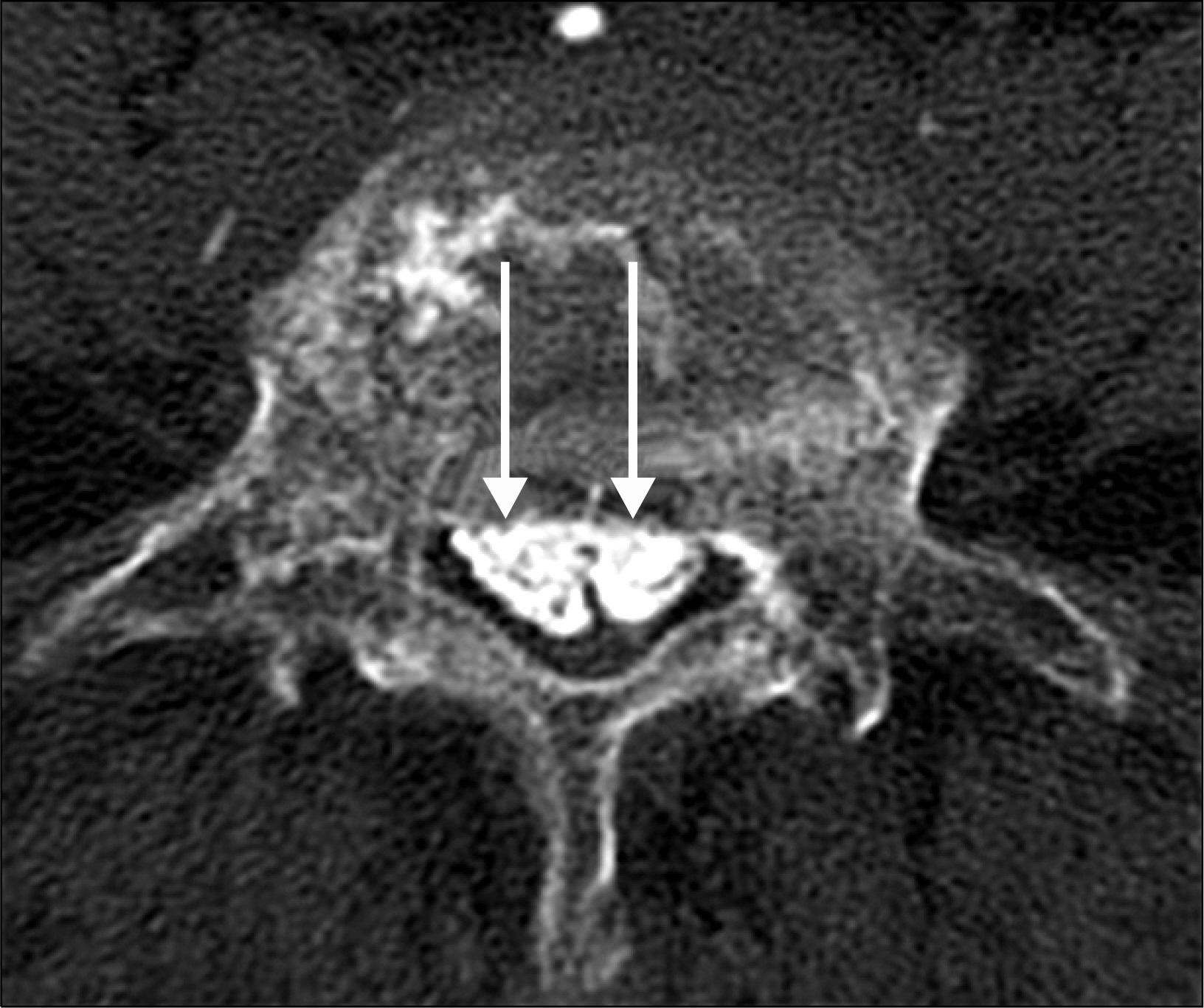
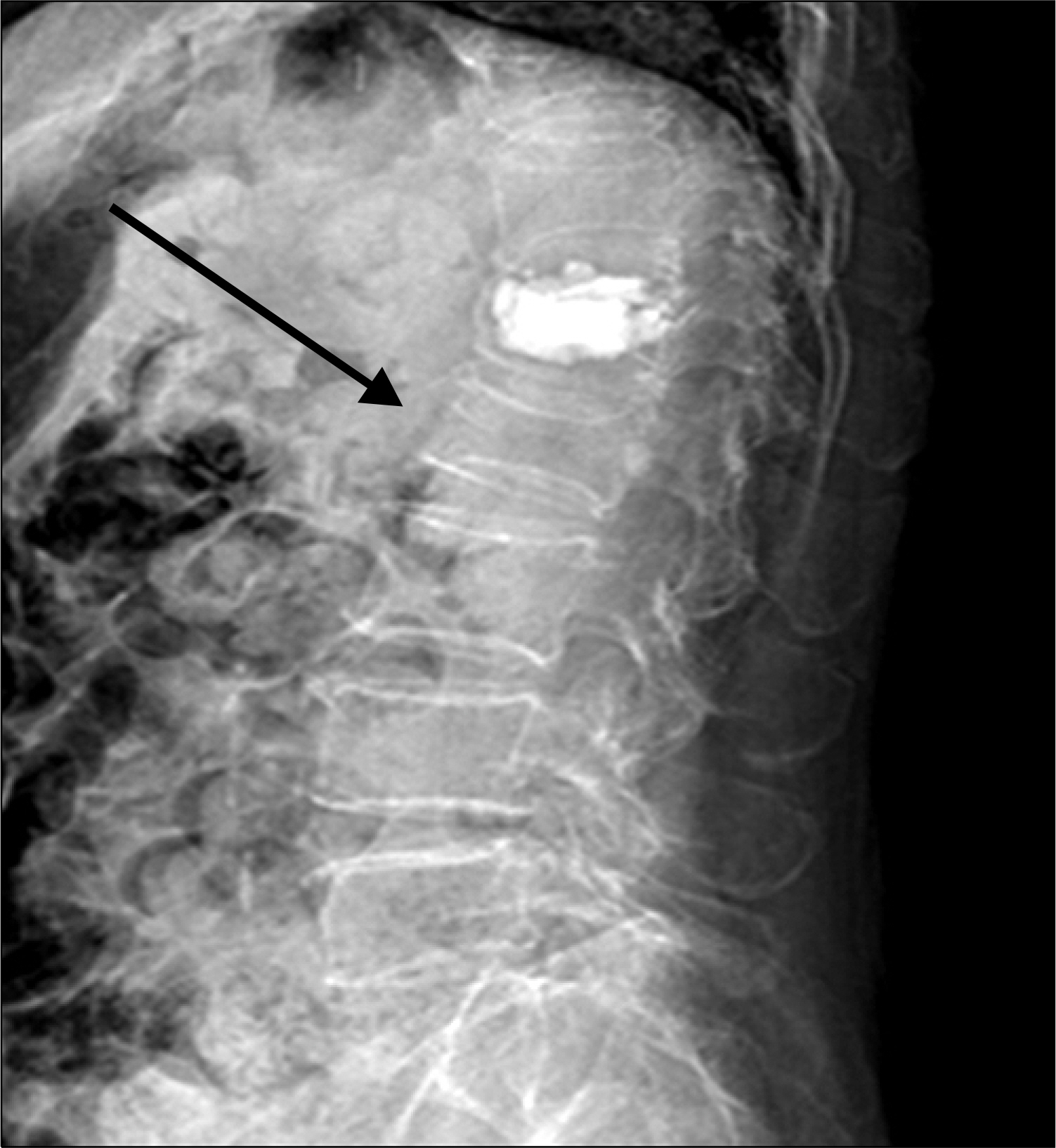
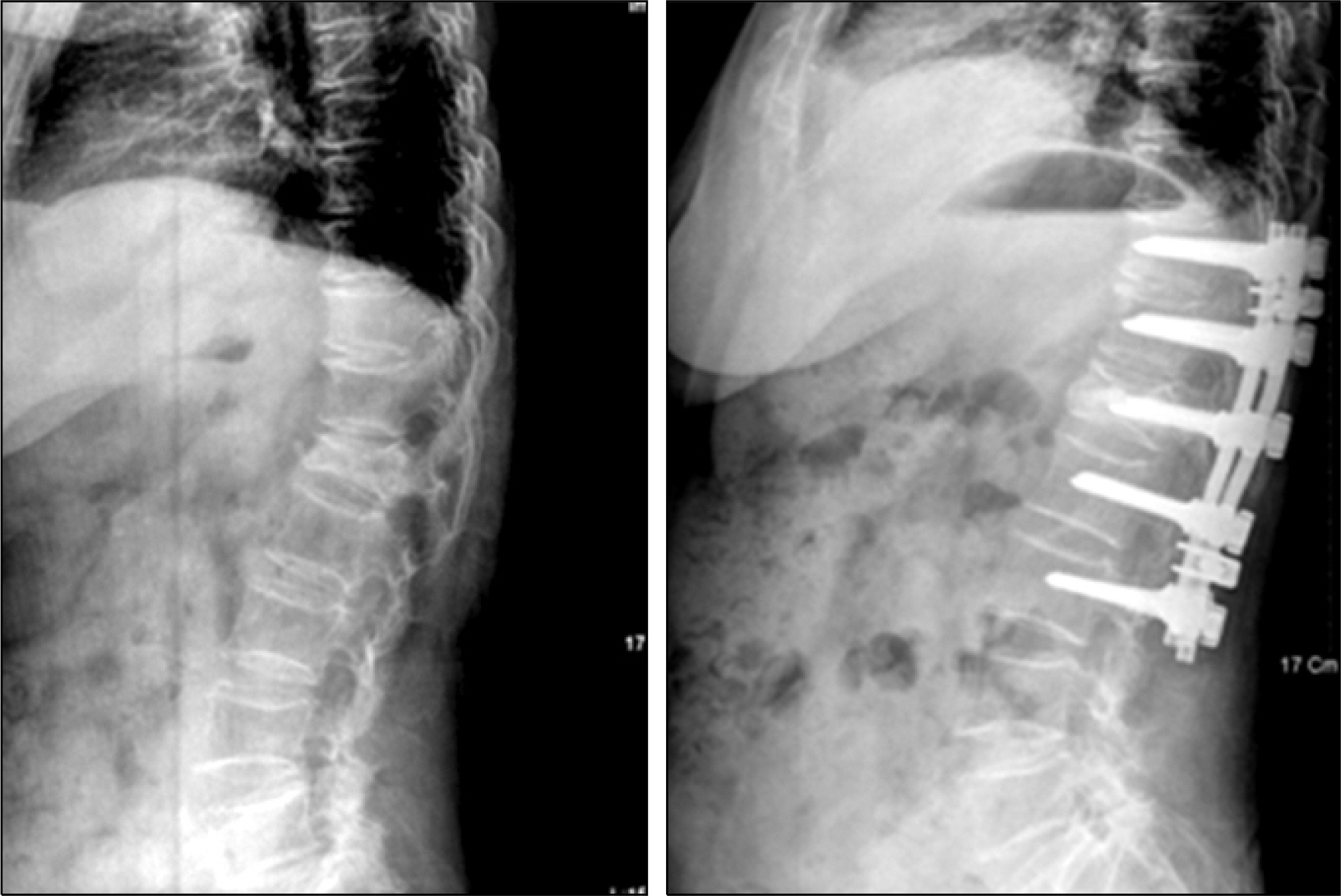
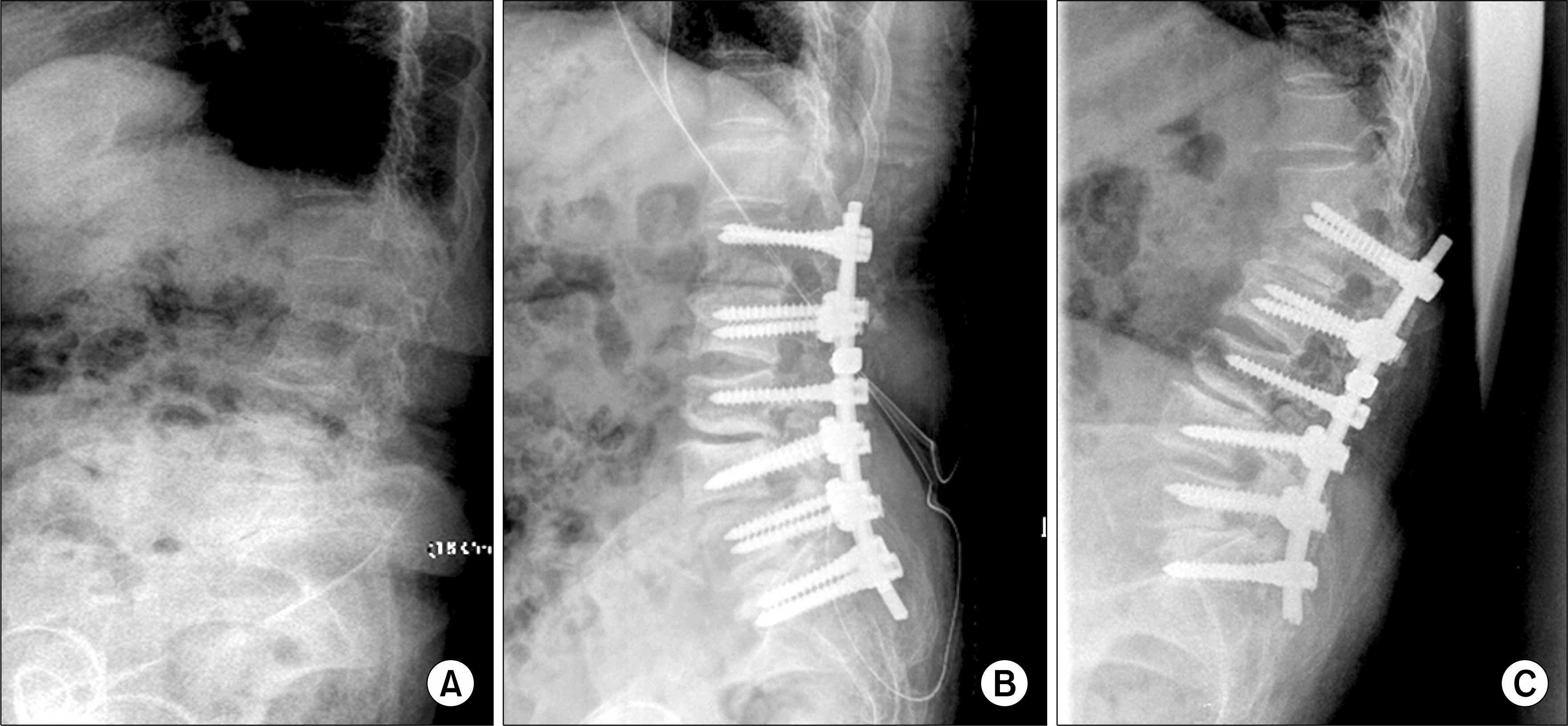
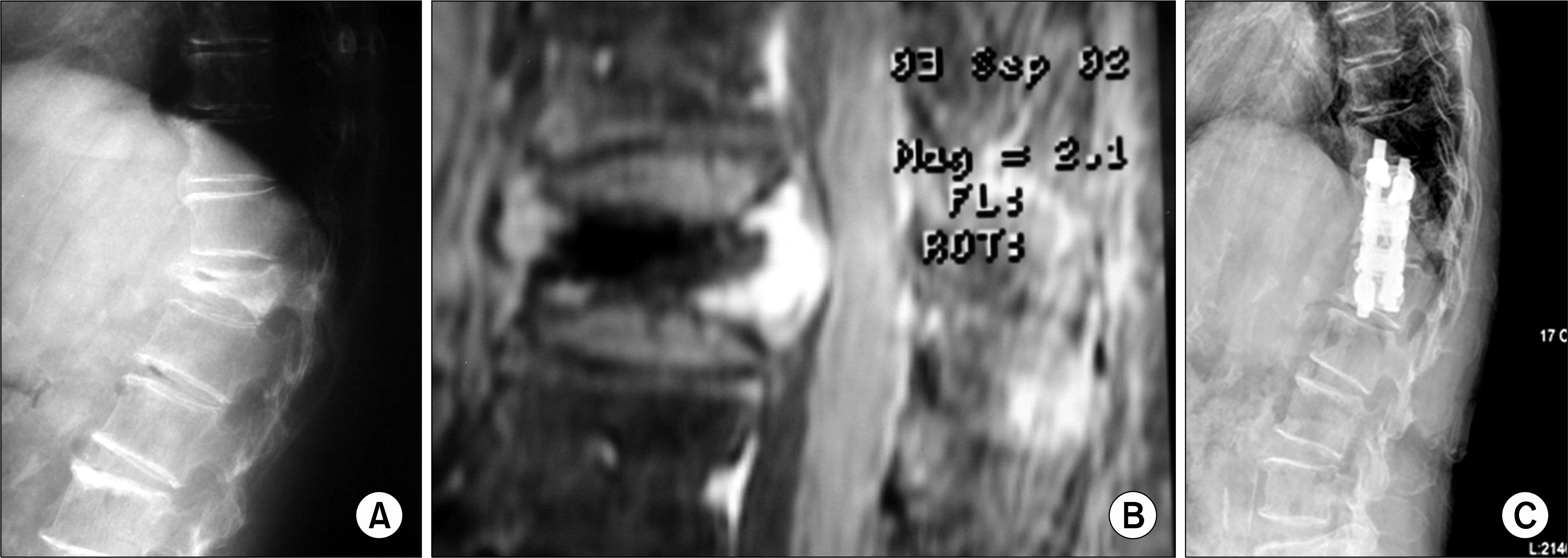
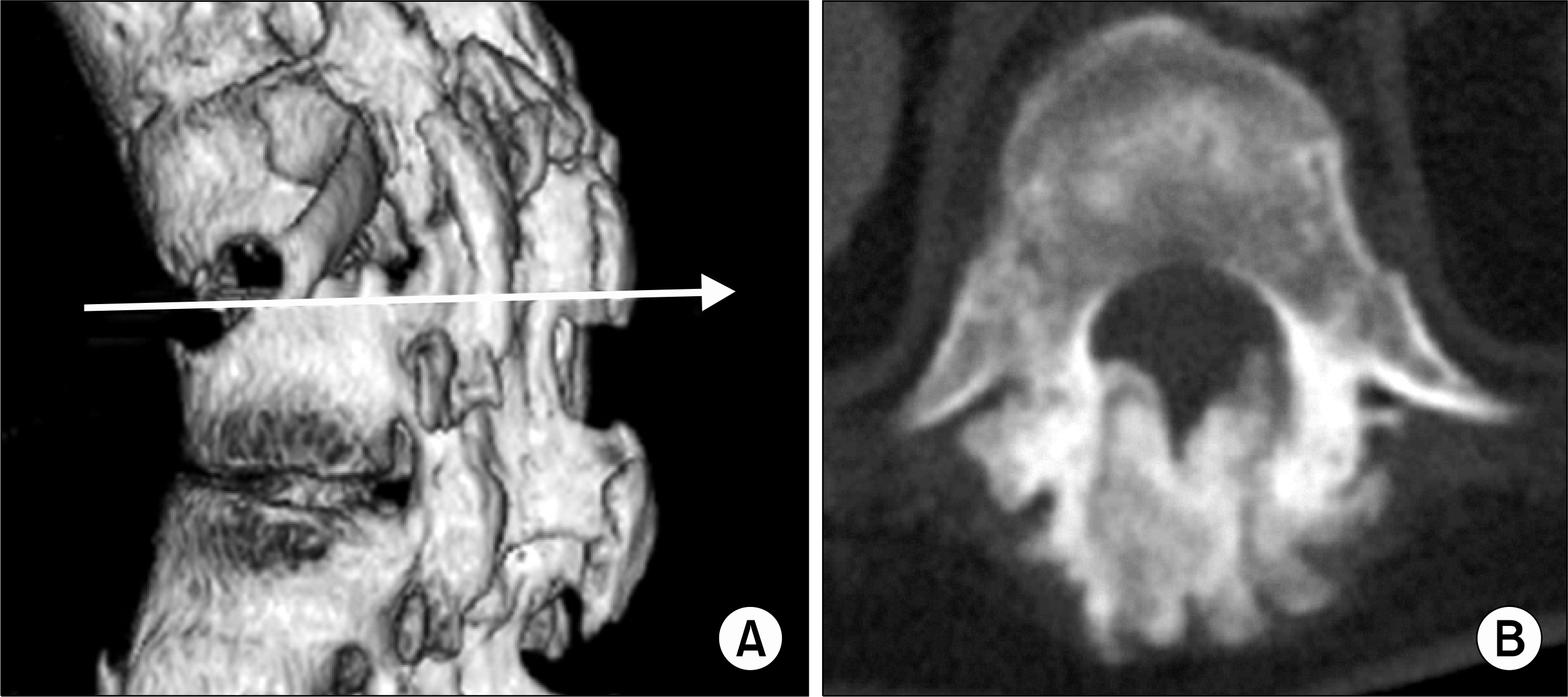
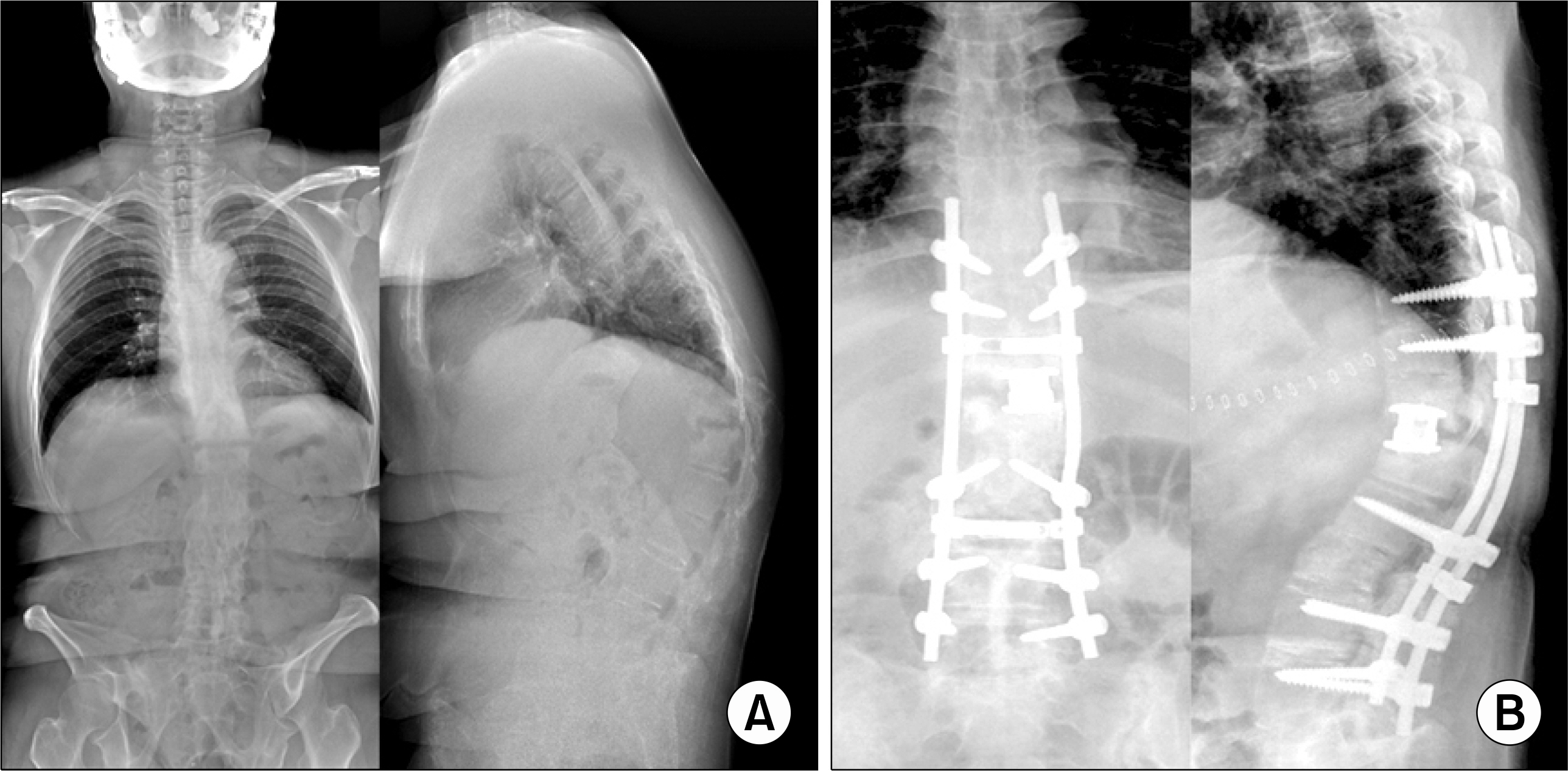
- Rheumatoid disorders are chronic multi-systemic diseases of unknown cause. The characteristic feature is persistent inflammatory synovitis usually involving peripheral joints in a symmetrical distribution. Features of spinal involvement in rheumatoid disorders include erosive synovitis, ligamentous subluxation, osteopenia, and vertebral-body fractures. In this article, authors describe common spinal disorders in rheumatoid diseases and also spinal surgery.
Keyword
Figure
Reference
-
References
1. Garrod AB. Nature and treatment of gout and rheumatic gout. London, Walton and Maberly. 1859.2. Wollowick AL, Casden AM, Kuflik PL, Neuwirth MJ. Rheumatoid arthritis in the cervical spine: What you need to know. Am J Orthop. 2007; 36:400–6.3. Rawlins BA, Girardi FP, Boachie-Adjei O. Rheumatoid arthritis of the cervical spine. Rheum Dis Clin North Am. 1998; 24:55–65.
Article4. Boden SD, Dodge LD, Bohlman HH, Rechtine GR. Rheumatoid arthritis of the cervical spine. A longterm analysis with predictors of paralysis and recovery. J Bone Joint Surg Am. 1993; 75:1282–97.
Article5. Cassar-Pullicino VN. The spine in rheumatological disorders. Imaging. 1999; 11:104–18.
Article6. Fujiwara K, Fujimoto M, Owaki H, Kono J, Nakase T, Yonenobu K, et al. Cervical lesions related to the systemic progression in rheumatoid arthritis. Spine. 1998; 23:2052–6.
Article7. Roche CJ, Eyes BE, Whitehouse GH. The rheumatoid cervical spine: signs of instability on plain cervical radiographs. Clin Radiol. 2002; 57:241–9.
Article8. Collins DN, Barnes CL, FitzRandolph RL. Cervical spine instability in rheumatoid patients having total hip or knee arthroplasty. Clin Orthop Relat Res. 1991; 272:127–35.
Article9. Pellicci PM, Ranawat CS, Tsairis P, Bryan WJ. A prospective study of the progression to rheumatoid arthritis of the cervical spine. J Bone Joint Surg Am. 1981; 63:342–50.10. Peppelman WC, Kraus DR, Donaldson WF III, Agarwal A. Cervical spine surgery in rheumatoid arthritis: improvement of neurologic deficit after cervical spine fusion. Spine. 1993; 18:2375–9.11. Ranawat CS, O'Leary P, Pellicci P, Tsairis P, Marchisello P, Dorr L. Cervical spine fusion in rheumatoid arthritis. J Bone Joint Surg Am. 1979; 61:1003–10.
Article12. Sunahara N, Matsunaga S, Mori T, Ijiri K, Sakou T. Clinical course of conservatively managed rheumatoid arthritis patients with myelopathy. Spine. 1997; 22:603–8.
Article13. Anderson DG, Vaccaro AR. Decision making in spinal care. P. 158, 164, 350, 371, New York, Thieme medical publishers. 2007.14. Barr JD, Barr MS, Lemley TJ, McCann RM. Percutaneous vertebroplasty for pain relief and spinal stabilization. Spine. 2000; 25:923–8.
Article15. Evans AJ, Jensen ME, Kip KE, DeNardo AJ, Lawler GJ, Negin GA, et al. Vertebral compression fractures: pain reduction and improvement in functional mobility after percutaneous polymethylmethacrylate vertebroplasty: retrospective report of 245 cases. Radiology. 2003; 226:366–72.16. Grados F, Depriester C, Cayrolle G, Hardy N, Deramond H, Fardellone P. Long-term observations of vertebral osteoporotic fractures treated by percutaneous vertebroplasty. Rheumatology (Oxford). 2000; 39:1410–4.
Article17. Jensen ME, Evans AJ, Mathis JM, Kallmes DF, Cloft HJ, Dion JE. Percutaneous polymethylmethacrylate vertebroplasty in the treatment of osteoporotic vertebral body compression fractures: technical aspects. AJNR Am J Neuroradiol. 1997; 18:1897–904.18. Coumans JV, Reinhardt MK, Lieberman IH. Kyphoplasty for vertebral compression fractures: 1-year clinical outcomes from a prospective study. J Neurosurg. 2003; 99:44–50.
Article19. Harrop JS, Prpa B, Reinhardt MK, Lieberman I. Primary and secondary osteoporosis: incidence of subsequent vertebral compression fractures after kyphoplasty. Spine. 2004; 29:2120–5.
Article20. Ledlie JT, Renfro M. Balloon kyphoplasty: one-year outcomes in vertebral body height restoration, chronic pain, and activity levels. J Neurosurg. 2003; 98:36–42.
Article21. Lieberman IH, Dudeney S, Reinhardt MK, Bell G. Initial outcome and efficacy of “kyphoplasty” in the treatment of painful osteoporotic vertebral compression fractures. Spine. 2001; 26:1631–8.
Article22. Phillips FM, Ho E, Campbell-Hupp M, McNally T, Todd Wetzel F, Gupta P. Early radiographic and clinical results of balloon kyphoplasty for the treatment of osteoporotic vertebral compression fractures. Spine. 2003; 28:2260–5.
Article23. Bennett DL, Ohashi K, El-Khoury GY. Spondyloarthropathies: ankylosing spondylitis and psoriatic arthritis. Radiol Clin North Am. 2004; 42:121–34.
Article24. Hitchon PW, From AM, Brenton MD, Glaser JA, Torner JC. Fractures of the thoracolumbar spine complicating ankylosing spondylitis. J Neurosurg. 2002; 97:218–22.
Article25. Miceli-Richard C, van der Heijde D, Dougados M. Spondyloarthropathy for p racticing rheumatologists: diagnosis, indication for disease-controlling antirheumatic therapy, and evaluation of the response. Rheum Dis Clin North Am. 2003; 29:449–62.26. Smith-peterson MN, Larson CB, Aufranc OE. Osteotomy of the spine for correction of flexion deformitiy in rheumatoid arthritis. J Bone Joint Surg. 1945; 27:1–11.27. Kim KT, Lee SU, Kim YW, Kwon OS, Cho CH. Posterior closed wedge lumbar osteotomy in the kyphotic deformity of ankylosing spondylitis. J Korean Orthop Assoc. 1997; 32:1756–65.28. Kim KT, Suk KS, Lee SH, Bae SC. The treatment of spinal pseudarthrosis in ankylosing spondylitis J Korean Orthop Assoc. 2005; 40:312–20.29. Cammisa M, De Serio A, Guglielmi G. Diffuse idiopathic skeletal hyperostosis. Eur J Radiol. 1998; 27:7–11. S.
Article30. Resnick D, Niwayama G. Diffuse idiopathic skeletal hyperostosis (DISH): ankylosing hyperostosis of Forestier and Rotes-Querol. In: Resnick D, ed. Diagnosis of Bone and Joint Disorders. 3rd ed. p.1436–95. Philadelphia, WB Saunders,. 1995.31. Park YS, Lee IH, Kim MK. A Case of Myelopathy due to the nodular ossification of the ligamentum flavum of thoracic spine in diffuse idiopathic skeletal hyperostosis. J Korean Rheumatism Assoc. 2000; 7:174–8.32. Park YS, Cho WJ. A diffuse idiopathic skeletal hyperostosis patient associated withossification of thoracic ligamentum flavum −A case report–. J Korean Orthop Assoc. 2006; 41:574–7.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Sweet's Syndrome associated with Rheumatoid Arthritis
- Thoracolumbar Epidural Pannus Causing Paraplegia in Rhematoid Arthritis
- Cervical Compressive Myelopathy Due to Rheumatoid Pannus Presenting as Occipital Neuralgia
- Clinical significance of rheumatoid factor in juvenile rheumatoid arthritis
- New Diagnostic and Classification Criteria of Chronic Pain Diseases: Rheumatoid Arthritis, Fibromyalgia and Spondylarthritis