Korean J Gastroenterol.
2012 Mar;59(3):205-210. 10.4166/kjg.2012.59.3.205.
Transient Lower Esophageal Sphincter Relaxation and the Related Esophageal Motor Activities
- Affiliations
-
- 1Department of Internal Medicine, Soonchunhyang University College of Medicine, Bucheon, Korea. sjhong@schmc.ac.kr
- KMID: 1245204
- DOI: http://doi.org/10.4166/kjg.2012.59.3.205
Abstract
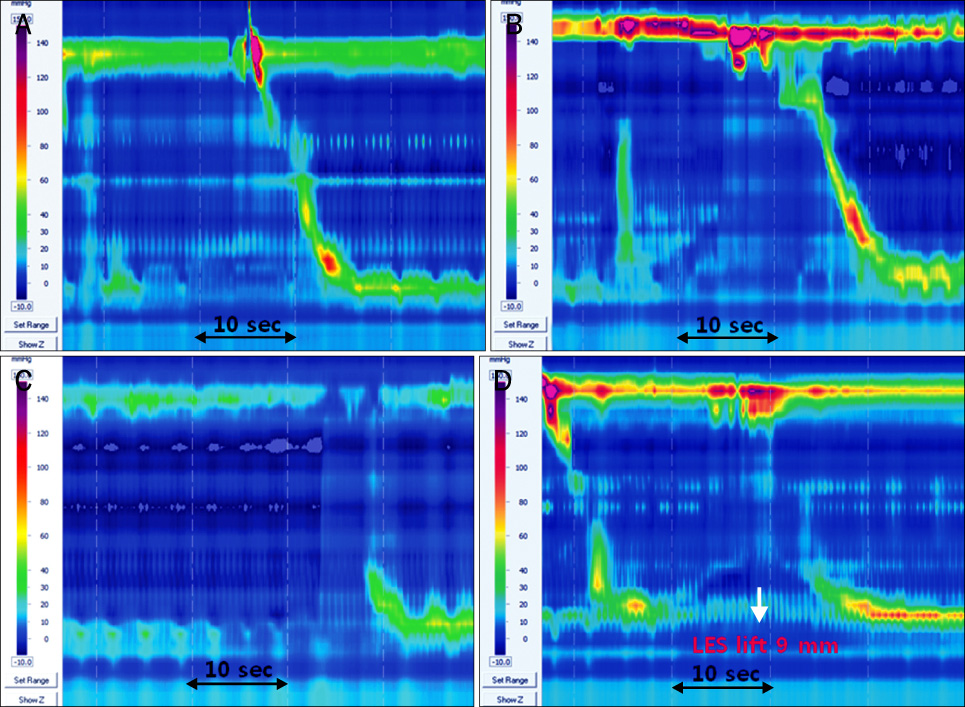
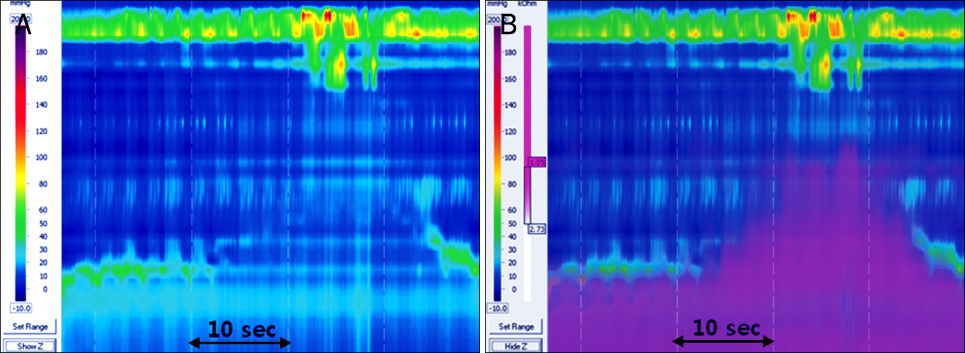
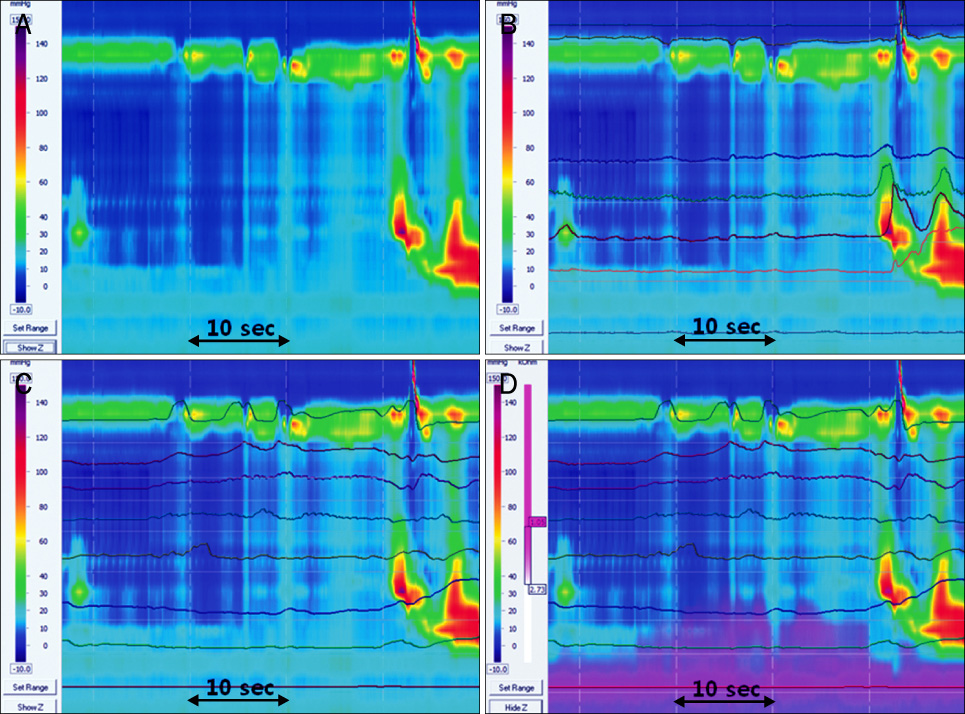
- Transient lower esophageal sphincter (LES) relaxation (TLESR) is defined as LES relaxation without a swallow. TLESRs are observed in both of the normal individuals and the patients with gastroesophageal reflux disorder (GERD). However, TLESR is widely considered as the major mechanism of the GERD. The new equipments such as high resolution manometry and impedance pH study is helped to understand of TLESR and the related esophageal motor activities. The strong longitudinal muscle contraction was observed during development of TLESR. Most of TLESRs are terminated by TLESR related motor events such as primary peristalsis and secondary contractions. The majority of TLESRs are associated with gastroesophageal reflux. Upper esophageal sphincter (UES) contraction is mainly associated with liquid reflux during recumbent position and UES relaxation predominantly related with air reflux during upright position. The frequency of TLESR in GERD patients seems to be not different compared to normal individuals, but the refluxate of GERD patients tend to be more acidic during TLESR.
MeSH Terms
Figure
Cited by 1 articles
-
Can Acid Pocket-targeting Alginate-antacid (Gaviscon Double Action) Relieve Upper Gastrointestinal Symptoms in Gastro-oesophageal Reflux Disease?
Sung Eun Kim, Moo In Park
Korean J Gastroenterol. 2014;63(6):386-388. doi: 10.4166/kjg.2014.63.6.386.
Reference
-
1. Mittal RK, McCallum RW. Characteristics and frequency of transient relaxations of the lower esophageal sphincter in patients with reflux esophagitis. Gastroenterology. 1988. 95:593–599.2. Schoeman MN, Tippett MD, Akkermans LM, Dent J, Holloway RH. Mechanisms of gastroesophageal reflux in ambulant healthy human subjects. Gastroenterology. 1995. 108:83–91.3. Mittal RK, Balaban DH. The esophagogastric junction. N Engl J Med. 1997. 336:924–932.4. Dent J, Dodds WJ, Friedman RH, et al. Mechanism of gastroesophageal reflux in recumbent asymptomatic human subjects. J Clin Invest. 1980. 65:256–267.5. Ye X, Liu H, Wu C, et al. Proton pump inhibitors therapy and risk of hip fracture: a systematic review and meta-analysis. Eur J Gastroenterol Hepatol. 2011. 23:794–800.6. Khalili H, Huang ES, Jacobson BC, Camargo CA Jr, Feskanich D, Chan AT. Use of proton pump inhibitors and risk of hip fracture in relation to dietary and lifestyle factors: a prospective cohort study. BMJ. 2012. 344:e372.7. Johnstone J, Nerenberg K, Loeb M. Meta-analysis: proton pump inhibitor use and the risk of community-acquired pneumonia. Aliment Pharmacol Ther. 2010. 31:1165–1177.8. Eom CS, Jeon CY, Lim JW, Cho EG, Park SM, Lee KS. Use of acid-suppressive drugs and risk of pneumonia: a systematic review and meta-analysis. CMAJ. 2011. 183:310–319.9. Trikudanathan G, Israel J, Cappa J, O'Sullivan DM. Association between proton pump inhibitors and spontaneous bacterial peritonitis in cirrhotic patients-a systematic review and meta-analysis. Int J Clin Pract. 2011. 65:674–678.10. Fernando H, Bassler N, Habersberger J, et al. Randomized double-blind placebo-controlled crossover study to determine the effects of esomeprazole on inhibition of platelet function by clopidogrel. J Thromb Haemost. 2011. 9:1582–1589.11. Kwok CS, Nijjar RS, Loke YK. Effects of proton pump inhibitors on adverse gastrointestinal events in patients receiving clopidogrel: systematic review and meta-analysis. Drug Saf. 2011. 34:47–57.12. Farré R, Sifrim D. Regulation of basal tone, relaxation and contraction of the lower oesophageal sphincter. Relevance to drug discovery for oesophageal disorders. Br J Pharmacol. 2008. 153:858–869.13. Hershcovici T, Mashimo H, Fass R. The lower esophageal sphincter. Neurogastroenterol Motil. 2011. 23:819–830.14. Martin CJ, Patrikios J, Dent J. Abolition of gas reflux and transient lower esophageal sphincter relaxation by vagal blockade in the dog. Gastroenterology. 1986. 91:890–896.15. Holloway RH, Penagini R, Ireland AC. Criteria for objective definition of transient lower esophageal sphincter relaxation. Am J Physiol. 1995. 268:G128–G133.16. Roman S, Zerbib F, Belhocine K, des Varannes SB, Mion F. High resolution manometry to detect transient lower oesophageal sphincter relaxations: diagnostic accuracy compared with perfused-sleeve manometry, and the definition of new detection criteria. Aliment Pharmacol Ther. 2011. 34:384–393.17. Rohof WO, Boeckxstaens GE, Hirsch DP. High-resolution esophageal pressure topography is superior to conventional sleeve manometry for the detection of transient lower esophageal sphincter relaxations associated with a reflux event. Neurogastroenterol Motil. 2011. 23:427–432.18. Pandolfino JE, Zhang QG, Ghosh SK, Han A, Boniquit C, Kahrilas PJ. Transient lower esophageal sphincter relaxations and reflux: mechanistic analysis using concurrent fluoroscopy and high-resolution manometry. Gastroenterology. 2006. 131:1725–1733.19. Babaei A, Bhargava V, Korsapati H, Zheng WH, Mittal RK. A unique longitudinal muscle contraction pattern associated with transient lower esophageal sphincter relaxation. Gastroenterology. 2008. 134:1322–1331.20. Mittal RK, Karstens A, Leslie E, Babaei A, Bhargava V. Ambulatory high-resolution manometry, lower esophageal sphincter lift and transient lower esophageal sphincter relaxation. Neurogastroenterol Motil. 2012. 24:40–46.21. Tipnis NA, Liu J, Puckett JL, Mittal RK. Common cavity pressure during gastroesophageal reflux: reassessment using simultaneous pressure, impedance, and ultrasound imaging. Am J Physiol Gastrointest Liver Physiol. 2006. 290:G1149–G1156.22. Sakurai J, Obata K, Ozaki N, et al. Activation of extracellular signal-regulated protein kinase in sensory neurons after noxious gastric distention and its involvement in acute visceral pain in rats. Gastroenterology. 2008. 134:1094–1103.23. Miwa H, Kondo T, Oshima T, Fukui H, Tomita T, Watari J. Esophageal sensation and esophageal hypersensitivity-overview from bench to bedside. J Neurogastroenterol Motil. 2010. 16:353–362.24. Kuribayashi S, Massey BT, Hafeezullah M, et al. Terminating motor events for TLESR are influenced by the presence and distribution of refluxate. Am J Physiol Gastrointest Liver Physiol. 2009. 297:G71–G75.25. Babaei A, Bhargava V, Mittal RK. Upper esophageal sphincter during transient lower esophageal sphincter relaxation: effects of reflux content and posture. Am J Physiol Gastrointest Liver Physiol. 2010. 298:G601–G607.26. Trudgill NJ, Riley SA. Transient lower esophageal sphincter relaxations are no more frequent in patients with gastroesophageal reflux disease than in asymptomatic volunteers. Am J Gastroenterol. 2001. 96:2569–2574.27. Iwakiri K, Hayashi Y, Kotoyori M, et al. Transient lower esophageal sphincter relaxations (TLESRs) are the major mechanism of gastroesophageal reflux but are not the cause of reflux disease. Dig Dis Sci. 2005. 50:1072–1077.28. Hayashi Y, Iwakiri K, Kotoyori M, Sakamoto C. Mechanisms of acid gastroesophageal reflux in the Japanese population. Dig Dis Sci. 2008. 53:1–6.29. Sifrim D, Holloway R, Silny J, Tack J, Lerut A, Janssens J. Composition of the postprandial refluxate in patients with gastroesophageal reflux disease. Am J Gastroenterol. 2001. 96:647–655.30. Wong WM, Lai KC, Hui WM, et al. Pathophysiology of gastroesophageal reflux diseases in Chinese--role of transient lower esophageal sphincter relaxation and esophageal motor dysfunction. Am J Gastroenterol. 2004. 99:2088–2093.31. Pandolfino JE, Shi G, Trueworthy B, Kahrilas PJ. Esophagogastric junction opening during relaxation distinguishes nonhernia reflux patients, hernia patients, and normal subjects. Gastroenterology. 2003. 125:1018–1024.32. Schneider JH, Küper MA, Königsrainer A, Brücher BL. Transient lower esophageal sphincter relaxation and esophageal motor response. J Surg Res. 2010. 159:714–719.33. Schneider JH, Küper M, Königsrainer A, Brücher B. Transient lower esophageal sphincter relaxation in morbid obesity. Obes Surg. 2009. 19:595–600.34. Grossi L, Ciccaglione AF, Travaglini N, Marzio L. Transient lower esophageal sphincter relaxations and gastroesophageal reflux episodes in healthy subjects and GERD patients during 24 hours. Dig Dis Sci. 2001. 46:815–821.35. Kwiatek MA, Post J, Pandolfino JE, Kahrilas PJ. Transient lower oesophageal sphincter relaxation in achalasia: everything but LOS relaxation. Neurogastroenterol Motil. 2009. 21:1294–1301.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Obesity is Associated with Increased Transient Lower Esophageal Sphincter Relaxation
- Specific Movement of Esophagus During Transient Lower Esophageal Sphincter Relaxation in Gastroesophageal Reflux Disease
- Is Aperistalsis with Complete Lower Esophageal Sphincter Relaxation an Early Stage of Classic Achalasia?
- A Case of Esophageal Carcinoma Following Esophagomyotomy for Achalasia
- A Case of Nutcracker Esophagus Combined with Hypertensive Lower Esophageal Sphincter