Yonsei Med J.
2012 Mar;53(2):328-336. 10.3349/ymj.2012.53.2.328.
Spontaneous Bacterial Peritonitis in Patients with Hepatitis B Virus-Related Liver Cirrhosis: Community-Acquired versus Nosocomial
- Affiliations
-
- 1Department of Internal Medicine, Yonsei University College of Medicine, Seoul, Korea. ahnsh@yuhs.ac
- 2Institute of Gastroenterology, Yonsei University College of Medicine, Seoul, Korea.
- 3Department of Laboratory Medicine, Yonsei University College of Medicine, Seoul, Korea.
- 4Liver Cirrhosis Clinical Research Center, Seoul, Korea.
- 5National Health Insurance Corporation, Ilsan Hospital, Goyang, Korea.
- 6Brain Korea 21 Project for Medical Science, Seoul, Korea.
- KMID: 1120199
- DOI: http://doi.org/10.3349/ymj.2012.53.2.328
Abstract
- PURPOSE
Spontaneous bacterial peritonitis (SBP) frequently develops in patients with liver cirrhosis; however, there is little data to suggest whether the acquisition site of infection influences the prognosis. This study compared the bacteriology, clinical characteristics and treatment outcomes of community-acquired SBP (CA-SBP) and nosocomial SBP (N-SBP).
MATERIALS AND METHODS
The medical records of 130 patients with hepatitis B virus (HBV)-related liver cirrhosis, who had experienced a first episode of SBP between January 1999 and December 2008, were reviewed.
RESULTS
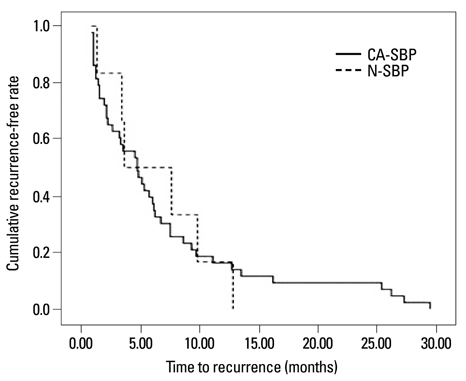
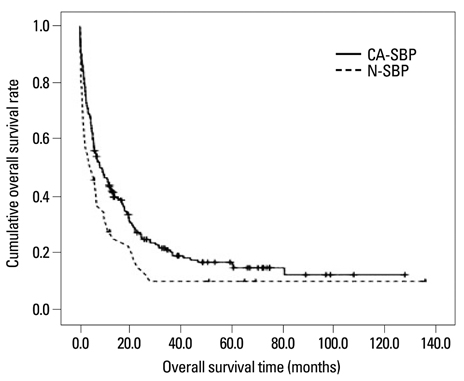
The study population included 111 (85.4%) patients with CA-SBP and 19 (14.6%) patients with N-SBP. Baseline and microbiological characteristics as well as clinical course, including in-hospital mortality, did not differ between patients with CA-SBP and those with N-SBP (all p>0.05). The median survival time was 6.5 months, and 117 (90.0%) patients died during the follow-up period. Patients with CA-SBP and N-SBP survived for median periods of 6.6 and 6.2 months, respectively, without significant difference (p=0.569). Time to recurrence did not differ between patients with CA-SBP and N-SBP (4.7 vs. 3.6 months, p=0.925).
CONCLUSION
The acquisition site of infection did not affect clinical outcomes for patients with HBV-related liver cirrhosis who had experienced their first episode of SBP. Third-generation cephalosporins may be effective in empirically treating these patients, regardless of the acquisition site of the infection.
MeSH Terms
Figure
Reference
-
1. Akriviadis EA, Runyon BA. Utility of an algorithm in differentiating spontaneous from secondary bacterial peritonitis. Gastroenterology. 1990. 98:127–133.
Article2. Runyon BA. Spontaneous bacterial peritonitis: an explosion of information. Hepatology. 1988. 8:171–175.
Article3. Such J, Runyon BA. Spontaneous bacterial peritonitis. Clin Infect Dis. 1998. 27:669–674.
Article4. Navasa M, Follo A, Llovet JM, Clemente G, Vargas V, Rimola A, et al. Randomized, comparative study of oral ofloxacin versus intravenous cefotaxime in spontaneous bacterial peritonitis. Gastroenterology. 1996. 111:1011–1017.
Article5. Runyon BA, McHutchison JG, Antillon MR, Akriviadis EA, Montano AA. Short-course versus long-course antibiotic treatment of spontaneous bacterial peritonitis. A randomized controlled study of 100 patients. Gastroenterology. 1991. 100:1737–1742.
Article6. Altman C, Grangé JD, Amiot X, Pelletier G, Lacaine F, Bodin F, et al. Survival after a first episode of spontaneous bacterial peritonitis. Prognosis of potential candidates for orthotopic liver transplantation. J Gastroenterol Hepatol. 1995. 10:47–50.
Article7. Sheer TA, Runyon BA. Spontaneous bacterial peritonitis. Dig Dis. 2005. 23:39–46.
Article8. Guarner C, Runyon BA, Young S, Heck M, Sheikh MY. Intestinal bacterial overgrowth and bacterial translocation in cirrhotic rats with ascites. J Hepatol. 1997. 26:1372–1378.
Article9. Fiuza C, Salcedo M, Clemente G, Tellado JM. In vivo neutrophil dysfunction in cirrhotic patients with advanced liver disease. J Infect Dis. 2000. 182:526–533.
Article10. Runyon BA. Patients with deficient ascitic fluid opsonic activity are predisposed to spontaneous bacterial peritonitis. Hepatology. 1988. 8:632–635.
Article11. Cheong HS, Kang CI, Lee JA, Moon SY, Joung MK, Chung DR, et al. Clinical significance and outcome of nosocomial acquisition of spontaneous bacterial peritonitis in patients with liver cirrhosis. Clin Infect Dis. 2009. 48:1230–1236.
Article12. Song JY, Jung SJ, Park CW, Sohn JW, Kim WJ, Kim MJ, et al. Prognostic significance of infection acquisition sites in spontaneous bacterial peritonitis: nosocomial versus community acquired. J Korean Med Sci. 2006. 21:666–671.
Article13. Bert F, Andreu M, Durand F, Degos F, Galdbart JO, Moreau R, et al. Nosocomial and community-acquired spontaneous bacterial peritonitis: comparative microbiology and therapeutic implications. Eur J Clin Microbiol Infect Dis. 2003. 22:10–15.
Article14. Terg R, Levi D, Lopez P, Rafaelli C, Rojter S, Abecasis R, et al. Analysis of clinical course and prognosis of culture-positive spontaneous bacterial peritonitis and neutrocytic ascites. Evidence of the same disease. Dig Dis Sci. 1992. 37:1499–1504.
Article15. Hoefs JC, Canawati HN, Sapico FL, Hopkins RR, Weiner J, Montgomerie JZ. Spontaneous bacterial peritonitis. Hepatology. 1982. 2:399–407.
Article16. Runyon BA, Hoefs JC. Culture-negative neutrocytic ascites: a variant of spontaneous bacterial peritonitis. Hepatology. 1984. 4:1209–1211.
Article17. Umgelter A, Reindl W, Miedaner M, Schmid RM, Huber W. Failure of current antibiotic first-line regimens and mortality in hospitalized patients with spontaneous bacterial peritonitis. Infection. 2009. 37:2–8.
Article18. Kim SU, Han KH, Nam CM, Park JY, Kim do Y, Chon CY, et al. Natural history of hepatitis B virus-related cirrhotic patients hospitalized to control ascites. J Gastroenterol Hepatol. 2008. 23:1722–1727.
Article19. Sort P, Navasa M, Arroyo V, Aldeguer X, Planas R, Ruiz-del-Arbol L, et al. Effect of intravenous albumin on renal impairment and mortality in patients with cirrhosis and spontaneous bacterial peritonitis. N Engl J Med. 1999. 341:403–409.
Article20. Kim SU, Kim do Y, Lee CK, Park JY, Kim SH, Kim HM, et al. Ascitic fluid infection in patients with hepatitis B virus-related liver cirrhosis: culture-negative neutrocytic ascites versus spontaneous bacterial peritonitis. J Gastroenterol Hepatol. 2010. 25:122–128.
Article21. Rimola A, García-Tsao G, Navasa M, Piddock LJ, Planas R, Bernard B, et al. Diagnosis, treatment and prophylaxis of spontaneous bacterial peritonitis: a consensus document. International Ascites Club. J Hepatol. 2000. 32:142–153.
Article22. al Amri SM, Allam AR, al Mofleh IA. Spontaneous bacterial peritonitis and culture negative neutrocytic ascites in patients with non-alcoholic liver cirrhosis. J Gastroenterol Hepatol. 1994. 9:433–436.
Article23. Novella M, Solà R, Soriano G, Andreu M, Gana J, Ortiz J, et al. Continuous versus inpatient prophylaxis of the first episode of spontaneous bacterial peritonitis with norfloxacin. Hepatology. 1997. 25:532–536.
Article24. Llovet JM, Bartolí R, March F, Planas R, Viñado B, Cabré E, et al. Translocated intestinal bacteria cause spontaneous bacterial peritonitis in cirrhotic rats: molecular epidemiologic evidence. J Hepatol. 1998. 28:307–313.
Article25. Park YH, Lee HC, Song HG, Jung S, Ryu SH, Shin JW, et al. Recent increase in antibiotic-resistant microorganisms in patients with spontaneous bacterial peritonitis adversely affects the clinical outcome in Korea. J Gastroenterol Hepatol. 2003. 18:927–933.
Article26. Kim YS, Um SH, Ryu HS, Lee JB, Lee JW, Park DK, et al. The prognosis of liver cirrhosis in recent years in Korea. J Korean Med Sci. 2003. 18:833–841.
Article27. Han YS, Kim BH, Baek IY, Lee DK, Kim KJ, Dong SH, et al. The change of the etiology, complications and cause of death of the liver cirrhosis in 1990s. Korean J Hepatol. 2000. 6:328–339.28. Kaymakoglu S, Eraksoy H, Okten A, Demir K, Calangu S, Cakaloglu Y, et al. Spontaneous ascitic infection in different cirrhotic groups: prevalence, risk factors and the efficacy of cefotaxime therapy. Eur J Gastroenterol Hepatol. 1997. 9:71–76.
Article29. Johnson CC, Baldessarre J, Levison ME. Peritonitis: update on pathophysiology, clinical manifestations, and management. Clin Infect Dis. 1997. 24:1035–1045.
Article30. Bhuva M, Ganger D, Jensen D. Spontaneous bacterial peritonitis: an update on evaluation, management, and prevention. Am J Med. 1994. 97:169–175.
Article31. Angeloni S, Leboffe C, Parente A, Venditti M, Giordano A, Merli M, et al. Efficacy of current guidelines for the treatment of spontaneous bacterial peritonitis in the clinical practice. World J Gastroenterol. 2008. 14:2757–2762.
Article32. Felisart J, Rimola A, Arroyo V, Perez-Ayuso RM, Quintero E, Gines P, et al. Cefotaxime is more effective than is ampicillin-tobramycin in cirrhotics with severe infections. Hepatology. 1985. 5:457–462.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Spontaneous Bacterial Peritonitis
- Prognostic Significance of Infection Acquisition Sites in Spontaneous Bacterial Peritonitis: Nosocomial versus Community Acquired
- Spontaneous Bacterial Empyema in a Patient with Liver Cirrhosis
- Spontaneous Bacterial Peritonitis Caused by Hafnia alvei in a Patient with Liver Cirrhosis
- Post-traumatic primary bacterial peritonitis