Korean J Radiol.
2004 Sep;5(3):171-177. 10.3348/kjr.2004.5.3.171.
Acute Necrotizing Encephalopathy in Korean Infants and Children: Imaging Findings and Diverse Clinical Outcome
- Affiliations
-
- 1Department of Radiology and Center for Imaging Science, Samsung Medical Center, Sungkyunkwan University School of Medicine, Korea. jhkate.kim@samsung.com
- 2Department of Radiology, Seoul National University College of Medicine, Korea.
- 3Department of Radiology, Incheon Medical Center, College of Medicine, Inha University, Korea.
- 4Department of Radiology, Asan Kang Nung Hospital, Korea.
- 5Department of Radiology, Asan Medical Center, University of Ulsan College of Medicine, Korea.
- 6Department of Radiology, Gachon Medical School, Ghil Medical Center, Korea.
- 7Department of Pediatrics, Samsung Medical Center, Sungkyunkwan University School of Medicine, Korea.
- KMID: 1118822
- DOI: http://doi.org/10.3348/kjr.2004.5.3.171
Abstract
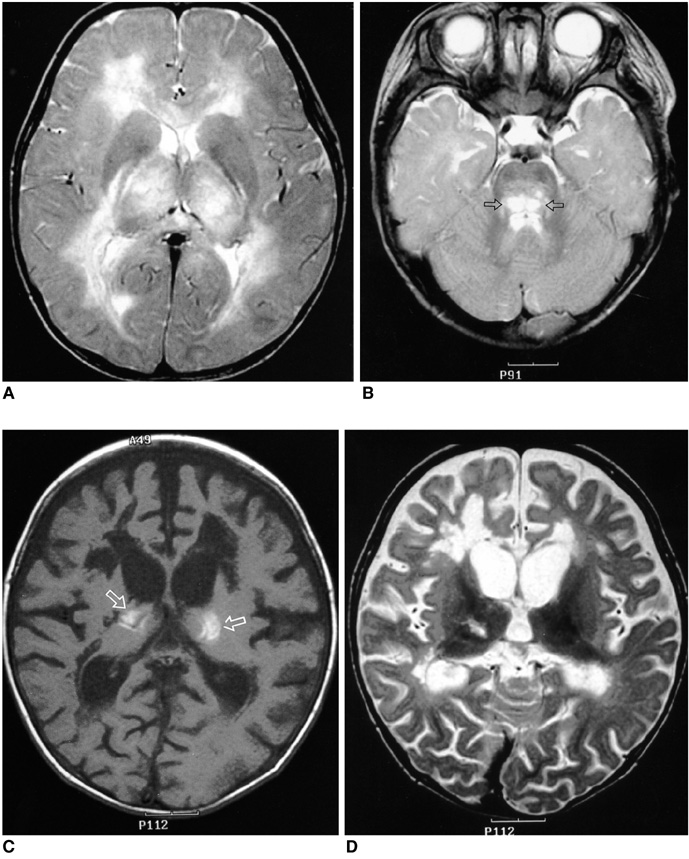
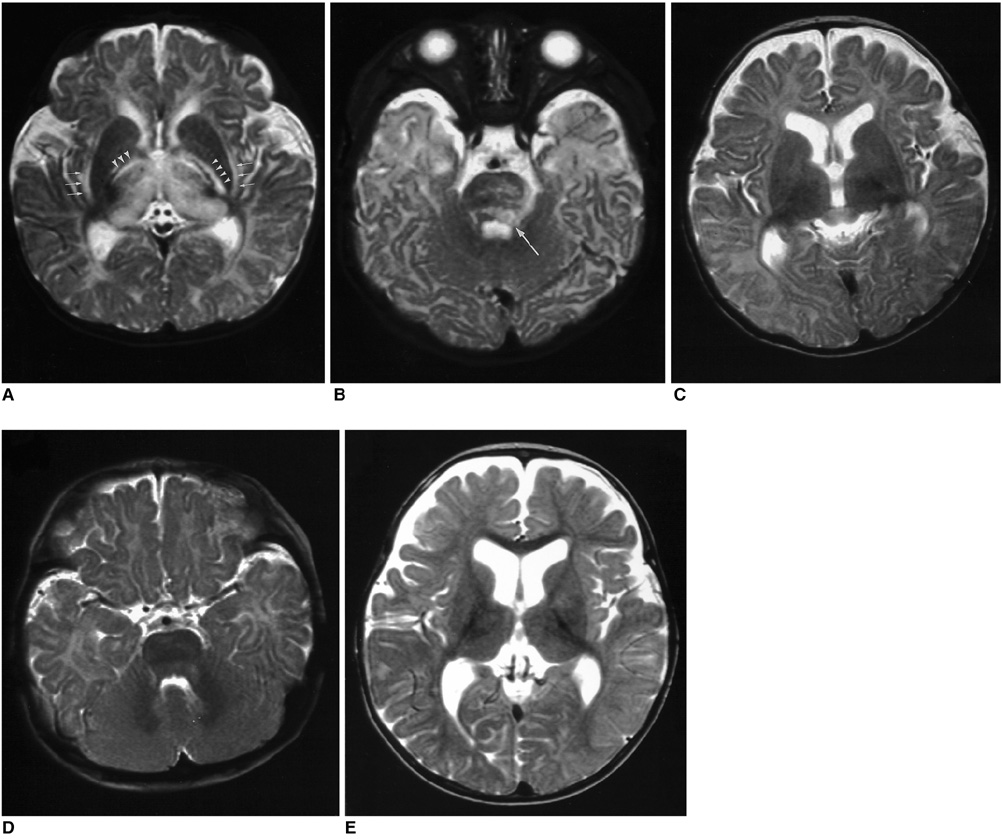
OBJECTIVE
The purpose of our study was to describe acute necrotizing encephalopathy in Korean infants and children, and we sought to evaluate the prognostic factors. MATERIALS AND METHODS: Acute necrotizing encephalopathy was diagnosed in 14 Korean infants and children. We retrospectively analyzed the neuroimaging findings including the follow-up changes. The clinical course of the disease was graded, and we evaluated prognostic factors including age, serum level of the aminotransferase, hemorrhage, and localized atrophy of the brain. RESULTS: This encephalopathy predominantly affected the bilateral thalami (n=14), pons (n=12), and midbrain (n=10) in a symmetrical pattern. Hemorrhage was observed in eight patients (57%). On the follow-up images (n=12), the brain lesions were reduced in extent for all patients, and generalized atrophy was seen in six patients. Localized tissue loss was observed in five patients and a complete resolution occurred for one patient. All the patients survived and two recovered completely; mild (n=6) to severe (n=6) neurological deficits persisted in the remaining 12 patients. The significant prognostic factors identified in this study were the presence of hemorrhage (p = 0.009) and localized atrophy (p = 0.015). CONCLUSION: Acute necrotizing encephalopathy in Korean patients showed the characteristic patterns of the post-infectious encephalopathy as described in the literature. The high survival rate and the relatively favorable clinical course observed for the present study suggest a more diverse spectrum of disease severity than was previously described. The presence of hemorrhage and localized tissue loss on MR images may suggest a poor prognosis.
MeSH Terms
Figure
Cited by 2 articles
-
Clinical Spectrum and Prognostic Factors of Acute Necrotizing Encephalopathy in Children
Hye-Eun Seo, Su-Kyeong Hwang, Byung Ho Choe, Min-Hyun Cho, Sung-Pa Park, Soonhak Kwon
J Korean Med Sci. 2010;25(3):449-453. doi: 10.3346/jkms.2010.25.3.449.Arterial Spin Labelling Perfusion, Proton MR Spectroscopy and Susceptibility-Weighted MR Findings of Acute Necrotizing Encephalopathy: a Case Report
Hwanwoong Kwon, Dae Seob Choi, Jungho Jang
Investig Magn Reson Imaging. 2019;23(2):157-161. doi: 10.13104/imri.2019.23.2.157.
Reference
-
1. Mizuguchi M, Abe J, Mikkaichi K, et al. Acute necrotising encephalopathy of childhood: a new syndrome presenting with multifocal, symmetric brain lesions. J Neurol Neurosurg Psychiatry. 1995. 58:555–561.2. Yagishita A, Nakano I, Ushioda T, Otsuki N, Hasegawa A. Acute encenphalopathy with bilateral thalamotegmental involvement in infants and children: imaging and pathology findings. AJNR Am J Neuroradiol. 1995. 16:439–447.3. Kato T. The similarity and homogeneity in acute necrotizing encephalopathy: acute cerebral necrotizing syndrome. Brain Dev. 1999. 21:138–139.4. Goo HW, Choi CG, Yoon CH, Ko TS. Acute necrotizing encephalopathy: diffusion MR imaging and localized proton MR spectroscopic findings in two infants. Korean J Radiol. 2003. 4:61–65.5. Kim TK, Eun BL, Cha SH, et al. Moyamoya disease in a child with previous acute necrotizing encephalopathy. Pediatr Radiol. 2003. 33:644–647. (Epub 2003 Jun 12).6. Mizuguchi M. Acute necrotizing encephalopathy of childhood: a novel form of acute encephalopathy prevalent in Japan and Taiwan. Brain Dev. 1997. 19:81–92.7. Campistol J, Gassio R, Pineda M, Fernandez-Alvarez E. Acute necrotizing encephalopathy of childhood (infantile bilateral thalamic necrosis): two non-Japanese cases. Dev Med Child Neurol. 1998. 40:771–774.8. Porto L, Lanferman H, Moller-Hartmann W, Jacobi G, Zanella F. Acute necrotising encephalopathy of childhood after exanthema subitum outside Japan or Taiwan. Neuroradiology. 1999. 41:732–734.9. Voudris KA, Skaardoutsou A, Haronitis I, Vagiakou EA, Zeis PM. Brain MRI findings in influenza A-associated acute necrotizing encephalopathy of childhood. Eur J Paediatr Neurol. 2001. 5:199–202.10. Ravid S, Topper L, Eviatar L. Acute necrotizing encephalopathy presenting as a basal ganglia syndrome. J Child Neurol. 2001. 16:461–462.11. Macieira L, Carvalho L, Fagundes F, Borges L, Neves F. Acute necrotizing encephalopathy due to influenza A. Rev Neurol. 2000. 30:798–799.12. Mastroyianni SD, Voudris KA, Katsarou E, et al. Acute necrotizing encephalopathy associated with parainfluenza virus in a Caucasian child. J Child Neurol. 2003. 18:570–572.13. Weitkamp JH, Spring MD, Brogan T, Moses H, Bloch KC, Wright PF. Influenza A virus-associated acute necrotizing encephalopathy in the United States. Pediatr Infect Dis J. 2004. 23:259–263.14. Protheroe SM, Mellor DH. Imaging in influenza A encephalitis. Arch Dis Child. 1991. 66:702–705.15. Matsushita E, Takita K, Shimada A. Suspected acute encephalopathy with symmetrical abnormal signal areas in the basal ganglia, thalamus, midbrain and pons diagnosed by magnetic resonance imaging. Acta Paediatr Jpn. 1997. 39:454–458.16. Sugaya N. Influenza-associated encephalopathy in Japan: pathogenesis and treatment. Pediatr Int. 2000. 42:215–218.17. Wang HS, Huang SC. Acute necrotizing encephalopathy of childhood. Chang Gung Med J. 2001. 24:1–10.18. Tran TD, Kubota M, Takeshita K, Yanagisawa M, Sakakihara Y. Varicella-associated acute necrotizing encephalopathy with a good prognosis. Brain Dev. 2001. 23:54–57.19. Fujimoto Y, Shibata M, Tsuyuki M, Okada M, Tsuzuki K. Influenza A virus encephalopathy with symmetrical thalamic lesions. Eur J Pediatr. 2000. 159:319–321.20. Harada M, Hisaoka S, Mori K, Yoneda K, Noda S, Nishitani H. Differences in water diffusion and lactate production in two different types of postinfectious encephalopathy. J Magn Reson Imaging. 2000. 11:559–563.21. Huang SM, Chen CC, Chiu PC, Cheng MF, Lai PH, Hsieh KS. Acute necrotizing encephalopathy of childhood associated with influenza type B virus infection in a 3-year-old girl. J Child Neurol. 2004. 19:64–67.22. Albayram S, Bilgi Z, Selcuk H, et al. Diffusion-weighted MR imaging findings of acute necrotizing encephalopathy. AJNR Am J Neuroradiol. 2004. 25:792–797.23. Sazgar M, Robinson JL, Chan AK, Sinclair DB. Influenza B acute necrotizing encephalopathy: a case report and literature review. Pediatr Neurol. 2003. 28:396–399.24. Mizuguchi M, Hayashi M, Nakano I, et al. Concentric structure of thalamic lesions in acute necrotizing encephalopathy. Neuroradiology. 2002. 44:489–493. (Epub 2002 Apr 04).25. Bassuk AG, Burrowes DM, McRae W. Acute necrotizing encephalopathy of childhood with radiographic progression over 10 hours. Neurology. 2003. 60:1552–1553.26. Yoshikawa H, Watanabe T, Abe T, Oda Y. Clinical diversity in acute necrotizing encephalopathy. J Child Neurol. 1999. 14:249–255.27. Cusmai R, Bertini E, Capua MD, et al. Bilateral, reversible, selective thalamic involvement demonstrated by brain MR and acute severe neurological dysfuction with favorable outcome. Neuropediatrics. 1994. 25:44–47.28. Barkovich AJ. Infections of the nervous system. Pediatric neuroimaging. 2000. 3rd ed. Philadelphia: Lippincott Willams & Wilkins;744–746.29. Kumar S, Misra UK, Kalita J, Salwani V, Gupta RK, Gujral R. MRI in Japanese encephalitis. Neuroradiology. 1997. 39:180–184.30. Abe T, Kojima K, Shoji H, et al. Japanese encephalitis. JMRI. 1998. 8:755–761.31. Anezaki T, Aida I, Takagi M, Inuzuka T, Tsuji S. An early-onset case of acute disseminated encephalomyelitis with bilateral thalamic lesions on MRI. Rinsho Shinkeigaku. 1999. 39:821–824.32. Baum PA, Barkovich AJ, Koch TK, Berg BO. Deep gray matter involvement in children with acute disseminated encephalomyelitis. AJNR Am J Neuroradiol. 1994. 15:1275–1283.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- MR Imaging of Acute Necrotizing Encephalopathy:A Report of Two Cases
- Acute Necrotizing Encephalopathy: Diffusion MR Imaging and Localized Proton MR Spectroscopic Findings in Two Infants
- Arterial Spin Labelling Perfusion, Proton MR Spectroscopy and Susceptibility-Weighted MR Findings of Acute Necrotizing Encephalopathy: a Case Report
- A Case of Acute Necrotizing Encephalopathy
- Rotavirus infection-associated central nervous system complications: clinicoradiological features and potential mechanisms