Korean J Radiol.
2011 Oct;12(5):568-578. 10.3348/kjr.2011.12.5.568.
Intra-Arterial Treatment in Patients with Acute Massive Gastrointestinal Bleeding after Endoscopic Failure: Comparisons between Positive versus Negative Contrast Extravasation Groups
- Affiliations
-
- 1Department of Radiology, Tri-Service General Hospital, National Defense Medical Center, Taipei, Taiwan, Republic of China. chougo2002@yahoo.com.tw
- 2Department of Internal Medicine, Division of Gastroenterology, Tri-Service General Hospital, National Defense Medical Center, Taipei, Taiwan, Republic of China.
- 3Department of Healthcare Administration, Asia University, Taichung, Taiwan, Republic of China.
- 4Department of Emergency Medicine, Tri-Service General Hospital, National Defense Medical Center, Taipei, Taiwan, Republic of China.
- 5Department of Surgery, Division of General Surgery, Tri-Service General Hospital, National Defense Medical Center, Taipei, Taiwan, Republic of China.
- KMID: 1116442
- DOI: http://doi.org/10.3348/kjr.2011.12.5.568
Abstract
OBJECTIVE
To determine whether treatment outcome is associated with visualization of contrast extravasation in patients with acute massive gastrointestinal bleeding after endoscopic failure.
MATERIALS AND METHODS
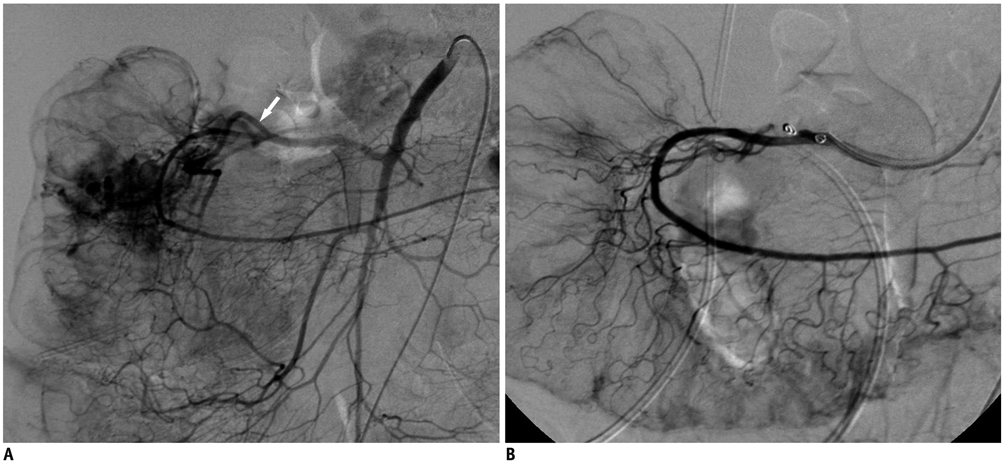
From January 2007 to December 2009, patients that experienced a first attack of acute gastrointestinal bleeding after failure of initial endoscopy were referred to our interventional department for intra-arterial treatment. We enrolled 79 patients and divided them into two groups: positive and negative extravasation. For positive extravasation, patients were treated by coil embolization; and in negative extravasation, patients were treated with intra-arterial vasopressin infusion. The two groups were compared for clinical parameters, hemodynamics, laboratory findings, endoscopic characteristics, and mortality rates.
RESULTS
Forty-eight patients had detectable contrast extravasation (positive extravasation), while 31 patients did not (negative extravasation). Fifty-six patients survived from this bleeding episode (overall clinical success rate, 71%). An elevation of hemoglobin level was observed in the both two groups; significantly greater in the positive extravasation group compared to the negative extravasation group. Although these patients were all at high risk of dying, the 90-day mortality rate was significantly lower in the positive extravasation than in the negative extravasation (20% versus 42%, p < 0.05). A multivariate analysis suggested that successful hemostasis (odds ratio [OR] = 28.66) is the most important predictor affecting the mortality in the two groups of patients.
CONCLUSION
Visualization of contrast extravasation on angiography usually can target the bleeding artery directly, resulting in a higher success rate to control of hemorrhage.
Keyword
MeSH Terms
-
Acute Disease
Adult
Aged
Aged, 80 and over
*Angiography
*Embolization, Therapeutic
Extravasation of Diagnostic and Therapeutic Materials/*radiography
Female
Gastrointestinal Hemorrhage/mortality/radiography/*therapy
Hemostasis, Endoscopic
Hemostatics/*administration & dosage
Humans
Infusions, Intra-Arterial
Male
Middle Aged
*Radiography, Interventional
Treatment Failure
Vasopressins/*administration & dosage
Young Adult
Figure
Reference
-
1. Cook DJ, Fuller HD, Guyatt GH, Marshall JC, Leasa D, Hall R, et al. Canadian Critical Care Trials Group. Risk factors for gastrointestinal bleeding in critically ill patients. N Engl J Med. 1994. 330:377–381.2. Rockall TA, Logan RF, Devlin HB, Northfield TC. Risk assessment after acute upper gastrointestinal haemorrhage. Gut. 1996. 38:316–321.3. Loffroy R, Guiu B. Role of transcatheter arterial embolization for massive bleeding from gastroduodenal ulcers. World J Gastroenterol. 2009. 15:5889–5897.4. Joo I, Kim HC, Chung JW, Jae HJ, Park JH. Risk factors for rebleeding after angiographically negative acute gastrointestinal bleeding. World J Gastroenterol. 2009. 15:4023–4027.5. Velayos FS, Williamson A, Sousa KH, Lung E, Bostrom A, Weber EJ, et al. Early predictors of severe lower gastrointestinal bleeding and adverse outcomes: a prospective study. Clin Gastroenterol Hepatol. 2004. 2:485–490.6. Loffroy R, Guiu B, D'Athis P, Mezzetta L, Gagnaire A, Jouve JL, et al. Arterial embolotherapy for endoscopically unmanageable acute gastroduodenal hemorrhage: predictors of early rebleeding. Clin Gastroenterol Hepatol. 2009. 7:515–523.7. Laing CJ, Tobias T, Rosenblum DI, Banker WL, Tseng L, Tamarkin SW. Acute gastrointestinal bleeding: emerging role of multidetector CT angiography and review of current imaging techniques. Radiographics. 2007. 27:1055–1070.8. Lau JY, Sung JJ, Lam YH, Chan AC, Ng EK, Lee DW, et al. Endoscopic retreatment compared with surgery in patients with recurrent bleeding after initial endoscopic control of bleeding ulcers. N Engl J Med. 1999. 340:751–756.9. Kapetanakis AM, Kyprizlis EP, Tsikrikas TS. Efficacy of repeated therapeutic endoscopy in patients with bleeding ulcer. Hepatogastroenterology. 1997. 44:288–293.10. Conrad SA. Acute upper gastrointestinal bleeding in critically ill patients: causes and treatment modalities. Crit Care Med. 2002. 30:S365–S368.11. Bell SD, Lau KY, Sniderman KW. Synchronous embolization of the gastroduodenal artery and the inferior pancreaticoduodenal artery in patients with massive duodenal hemorrhage. J Vasc Interv Radiol. 1995. 6:531–536.12. Dempsey DT, Burke DR, Reilly RS, McLean GK, Rosato EF. Angiography in poor-risk patients with massive nonvariceal upper gastrointestinal bleeding. Am J Surg. 1990. 159:282–286.13. Eriksson LG, Ljungdahl M, Sundbom M, Nyman R. Transcatheter arterial embolization versus surgery in the treatment of upper gastrointestinal bleeding after therapeutic endoscopy failure. J Vasc Interv Radiol. 2008. 19:1413–1418.14. Defreyne L, Vanlangenhove P, De Vos M, Pattyn P, Van Maele G, Decruyenaere J, et al. Embolization as a first approach with endoscopically unmanageable acute nonvariceal gastrointestinal hemorrhage. Radiology. 2001. 218:739–748.15. Gomes AS, Lois JF, McCoy RD. Angiographic treatment of gastrointestinal hemorrhage: comparison of vasopressin infusion and embolization. AJR Am J Roentgenol. 1986. 146:1031–1037.16. Conn HO, Ramsby GR, Storer EH, Mutchnick MG, Joshi PH, Phillips MM, et al. Intraarterial vasopressin in the treatment of upper gastrointestinal hemorrhage: a prospective, controlled clinical trial. Gastroenterology. 1975. 68:211–221.17. Waltman AC, Greenfield AJ, Novelline RA, Athanasoulis CA. Pyloroduodenal bleeding and intraarterial vasopressin: clinical results. AJR Am J Roentgenol. 1979. 133:643–646.18. Darcy M. Treatment of lower gastrointestinal bleeding: vasopressin infusion versus embolization. J Vasc Interv Radiol. 2003. 14:535–543.19. Chang YC, Tsang YM, Kung KL, Choi WM, Huang KM, Hsu CY, et al. Transcatheter control of intractible gastrointestinal bleeding. J Formos Med Assoc. 1991. 90:81–87.20. Tan KK, Wong D, Sim R. Superselective embolization for lower gastrointestinal hemorrhage: an institutional review over 7 years. World J Surg. 2008. 32:2707–2715.21. Walsh RM, Anain P, Geisinger M, Vogt D, Mayes J, Grundfest-Broniatowski S, et al. Role of angiography and embolization for massive gastroduodenal hemorrhage. J Gastrointest Surg. 1999. 3:61–65. discussion 66.22. Schenker MP, Duszak R Jr, Soulen MC, Smith KP, Baum RA, Cope C, et al. Upper gastrointestinal hemorrhage and transcatheter embolotherapy: clinical and technical factors impacting success and survival. J Vasc Interv Radiol. 2001. 12:1263–1271.23. Loffroy R, Guiu B, Mezzetta L, Minello A, Michiels C, Jouve JL, et al. Short- and long-term results of transcatheter embolization for massive arterial hemorrhage from gastroduodenal ulcers not controlled by endoscopic hemostasis. Can J Gastroenterol. 2009. 23:115–120.24. Padia SA, Geisinger MA, Newman JS, Pierce G, Obuchowski NA, Sands MJ. Effectiveness of coil embolization in angiographically detectable versus non-detectable sources of upper gastrointestinal hemorrhage. J Vasc Interv Radiol. 2009. 20:461–466.25. Kim JH, Shin JH, Yoon HK, Chae EY, Myung SJ, Ko GY, et al. Angiographically negative acute arterial upper and lower gastrointestinal bleeding: incidence, predictive factors, and clinical outcomes. Korean J Radiol. 2009. 10:384–390.26. Aina R, Oliva VL, Therasse E, Perreault P, Bui BT, Dufresne MP, et al. Arterial embolotherapy for upper gastrointestinal hemorrhage: outcome assessment. J Vasc Interv Radiol. 2001. 12:195–200.27. Frodsham A, Berkmen T, Ananian C, Fung A. Initial experience using N-butyl cyanoacrylate for embolization of lower gastrointestinal hemorrhage. J Vasc Interv Radiol. 2009. 20:1312–1319.28. Jae HJ, Chung JW, Jung AY, Lee W, Park JH. Transcatheter arterial embolization of nonvariceal upper gastrointestinal bleeding with N-butyl cyanoacrylate. Korean J Radiol. 2007. 8:48–56.29. Toyoda H, Nakano S, Kumada T, Takeda I, Sugiyama K, Osada T, et al. Estimation of usefulness of N-butyl-2-cyanoacrylate-lipiodol mixture in transcatheter arterial embolization for urgent control of life-threatening massive bleeding from gastric or duodenal ulcer. J Gastroenterol Hepatol. 1996. 11:252–258.30. Choi YH, Yoon CJ, Park JH, Chung JW, Kwon JW, Choi GM. Balloon-occluded retrograde transvenous obliteration for gastric variceal bleeding: its feasibility compared with transjugular intrahepatic portosystemic shunt. Korean J Radiol. 2003. 4:109–116.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Nonvariceal Upper Gastrointestinal Bleeding: the Usefulness of Rotational Angiography after Endoscopic Marking with a Metallic Clip
- Outcomes and complications of embolization for gastrointestinal bleeding
- Interventional radiological approaches to non-variceal gastrointestinal bleeding
- Refractory Gastrointestinal Bleeding: Role of Angiographic Intervention
- Immediate surgical treatment for massive extravasation of computed tomography contrast medium in the hand: a case report