Korean J Radiol.
2007 Aug;8(4):320-327. 10.3348/kjr.2007.8.4.320.
Tumor Response to Transcatheter Arterial Chemoembolization in Recurrent Hepatocellular Carcinoma after Living Donor Liver Transplantation
- Affiliations
-
- 1Department of Radiology, Severance Hospital, University of Yonsei, College of Medicine, Seoul, Korea. kbsung@amc.seoul.kr
- 2Department of Radiology, Seoul Asan Medical Center, University of Ulsan, College of Medicine, Seoul, Korea.
- KMID: 1110729
- DOI: http://doi.org/10.3348/kjr.2007.8.4.320
Abstract
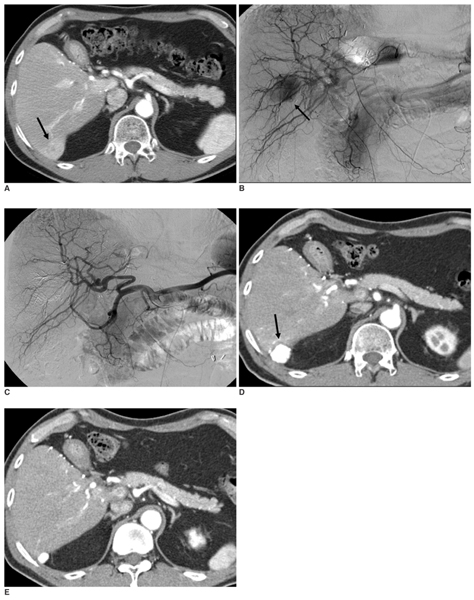
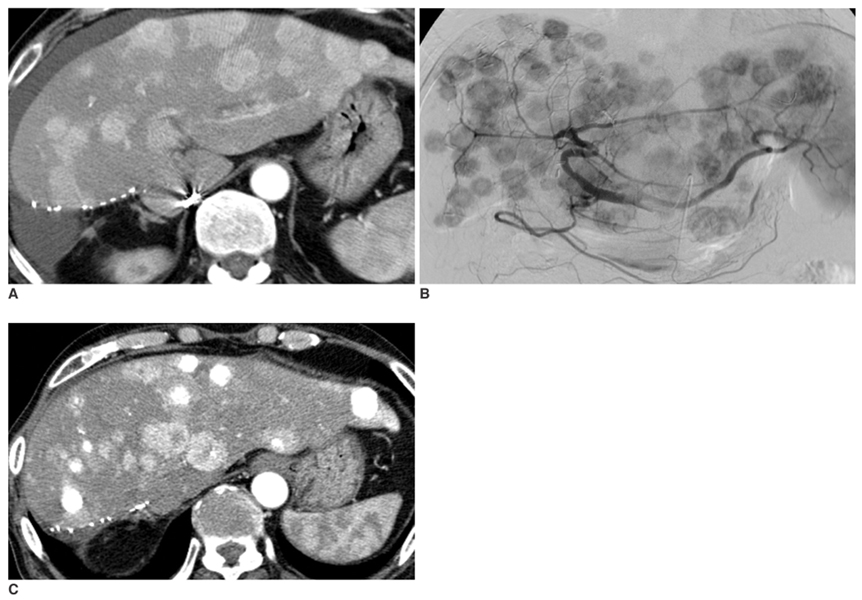
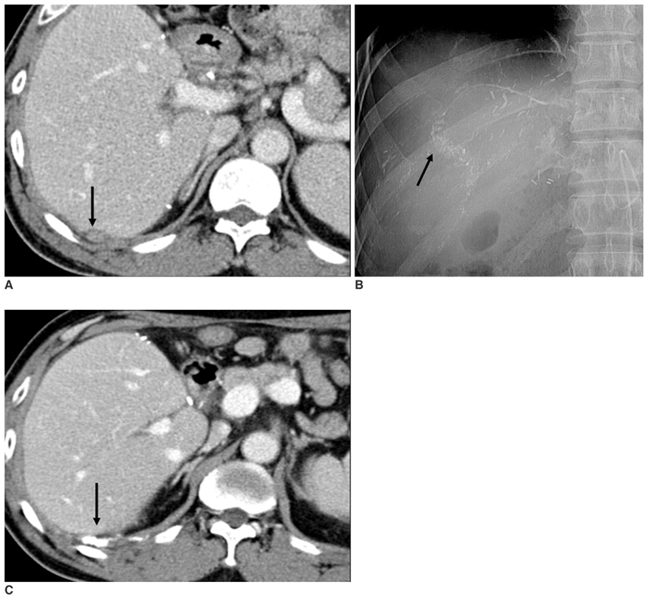
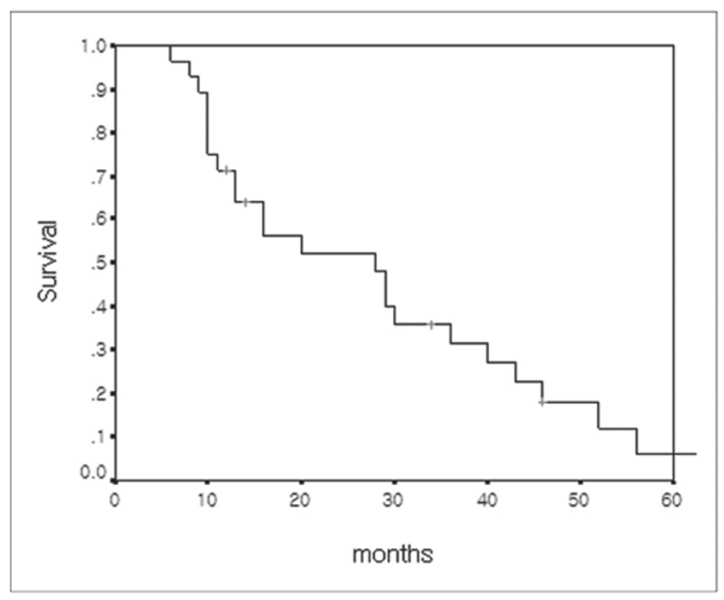
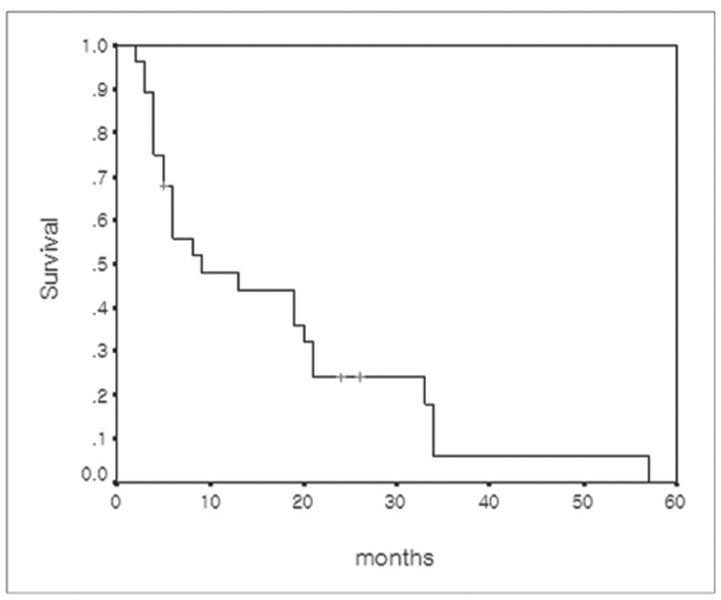
OBJECTIVE
To evaluate the tumor response and patient survival rate following transcatheter arterial chemoembolization (TACE) in recurrent hepatocellular carcinoma (r-HCC) after living donor liver transplantation (LDLT). MATERIALS AND METHODS: Twenty-eight patients with r-HCC underwent one or more cycles of TACE after LDLT (mean, 2.5 cycles). After a mixture of iodized oil and anti-cancer drugs was injected via the arteries feeding the tumors, these vessels were embolized with a gelatin sponge. Tumor response was determined by follow-up CT imaging on all patients four weeks after each TACE procedure. Patient survival was calculated using the Kaplan-Meier survival curve. RESULTS: After TACE, targeted tumor reduced in size by 25% or more in 19 of the 28 study patients (67.9%). However, intrahepatic recurrence or extrahepatic metastasis occurred in 21 of the 28 patients (75.0%) during the 3-month follow-up period and in 26 of the 28 patients (92.9%) during the 6-month period following TACE. Extrahepatic metastasis was noted in 18 of the 28 patients (64.3%). The 1-, 3- and 5-year survival rates following TACE were 47.9, 6.0 and 0%, respectively, with a mean survival of nine months in all patients. There were no significant complications related to TACE. CONCLUSION: TACE produces an effective tumor response for targeted r-HCC after LDLT. However, the survival rate of patients with r-HCC after LDLT is poor due to extrahepatic metastasis and intrahepatic recurrence.
MeSH Terms
-
Adult
Aged
Antineoplastic Agents/administration & dosage
Carcinoma, Hepatocellular/blood supply/mortality/*therapy
*Chemoembolization, Therapeutic
Cisplatin/administration & dosage
Contrast Media/administration & dosage
Female
Follow-Up Studies
Humans
Iodized Oil/administration & dosage
Liver Neoplasms/blood supply/mortality/*therapy
Liver Transplantation
Living Donors
Male
Middle Aged
Neoplasm Metastasis
Neoplasm Recurrence, Local/mortality/*therapy
Survival Rate
Figure
Reference
-
1. Kaihara S, Kiuchi T, Ueda M, Oike F, Fujimoto Y, Ogawa K, et al. Living-donor liver transplantation for hepatocellular carcinoma. Transplantation. 2003. 75:S37–S40.2. Kulik L, Abecassis M. Living donor liver transplantation for hepatocellular carcinoma. Gastroenterology. 2004. 127:S277–S282.3. O'Grady JG, Polson RJ, Rolles K, Calne RY, Williams R. Liver transplantation for malignant disease. Results in 93 consecutive patients. Ann Surg. 1988. 207:373–379.4. Ringe B, Pichlmayr R, Wittekind C, Tusch G. Surgical treatment of hepatocellular carcinoma: experience with liver resection and transplantation in 198 patients. World J Surg. 1991. 15:270–285.5. Bismuth H, Chiche L, Adam R, Castaing D, Diamond T, Dennison A. Liver resection versus transplantation for hepatocellular carcinoma in cirrhotic patients. Ann Surg. 1993. 218:145–151.6. Tan KC, Rela M, Ryder SD, Rizzi PM, Karani J, Portmann B, et al. Experience of orthotopic liver transplantation and hepatic resection for hepatocellular carcinoma of less than 8 cm in patients with cirrhosis. Br J Surg. 1995. 82:253–256.7. Todo S, Furukawa H. Living donor liver transplantation for adult patients with hepatocellular carcinoma: experience in Japan. Ann Surg. 2004. 240:451–459. discussion 459-461.8. Gondolesi GE, Roayaie S, Munoz L, Kim-Schluger L, Schiano T, Fishbein TM, et al. Adult living donor liver transplantation for patients with hepatocellular carcinoma: extending UNOS priority criteria. Ann Surg. 2004. 239:142–149.9. Regalia E, Fassati LR, Valente U, Pulvirenti A, Damilano I, Dardano G, et al. Pattern and management of recurrent hepatocellular carcinoma after liver transplantation. J Hepatobiliary Pancreat Surg. 1998. 5:29–34.10. Schwartz M, Roayaie S, Llovet J. How should patients with hepatocellular carcinoma recurrence after liver transplantation be treated? J Hepatol. 2005. 43:584–589.11. Margarit C, Charco R, Hidalgo E, Allende H, Castells L, Bilbao I. Liver transplantation for malignant diseases: selection and pattern of recurrence. World J Surg. 2002. 26:257–263.12. Mazzaferro V, Regalia E, Doci R, Andreola S, Pulvirenti A, Bozzetti F, et al. Liver transplantation for the treatment of small hepatocellular carcinomas in patients with cirrhosis. N Engl J Med. 1996. 334:693–699.13. Atiq OT, Kemeny N, Niedzwiecki D, Botet J. Treatment of unresectable primary liver cancer with intrahepatic fluorodeoxyuridine and mitomycin C through an implantable pump. Cancer. 1992. 69:920–924.14. Llovet JM, Bruix J. Systematic review of randomized trials for unresectable hepatocellular carcinoma: chemoembolization improves survival. Hepatology. 2003. 37:429–442.15. Llovet JM, Burroughs A, Bruix J. Hepatocellular carcinoma. Lancet. 2003. 362:1907–1917.16. Bruix J, Sala M, Llovet JM. Chemoembolization for hepatocellular carcinoma. Gastroenterology. 2004. 127:S179–S188.17. Ebied OM, Federle MP, Carr BI, Pealer KM, Li W, Amesur N, et al. Evaluation of responses to chemoembolization in patients with unresectable hepatocellular carcinoma. Cancer. 2003. 97:1042–1050.18. Roayaie S, Schwartz JD, Sung MW, Emre SH, Miller CM, Gondolesi GE, et al. Recurrence of hepatocellular carcinoma after liver transplant: patterns and prognosis. Liver Transpl. 2004. 10:534–540.19. Yokoyama I, Carr B, Saitsu H, Iwatsuki S, Starzl TE. Accelerated growth rates of recurrent hepatocellular carcinoma after liver transplantation. Cancer. 1991. 68:2095–2100.20. Steininger R, Herbst F, Fugger R, Muhlbacher F, Fritsch A. Immunosuppression does not enhance tumor growth after orthotopic liver transplantation for hepatoma. Transplant Proc. 1992. 24:2690–2692.21. Ishii H, Furuse J, Kinoshita T, Konishi M, Nakagohri T, Takahashi S, et al. Extrahepatic spread from hepatocellular carcinoma: who are candidates for aggressive anti-cancer treatment? Jpn J Clin Oncol. 2004. 34:733–739.22. Chung YH, Song IH, Song BC, Lee GC, Koh MS, Yoon HK, et al. Combined therapy consisting of intraarterial cisplatin infusion and systemic interferon-alpha for hepatocellular carcinoma patients with major portal vein thrombosis or distant metastasis. Cancer. 2000. 88:1986–1991.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Rupture of hepatocellular carcinoma after transcatheter arterial chemoembolization: A case report
- Liver transplantation for hepatocellular carcinoma with portal vein tumor thrombosis
- Indication and Outcome of Liver Transplantation In Patients with Hepatocellular Carcinoma
- Palliative Transcatheter Arterial Chemoembolization for Relieving Metastatic Bone Pain due to Hepatocellular Carcinoma: A Case Report
- Hepatocellular Carcinoma Extending to the Inferior Vena Cava and Right Atrium-A Case Report of 4 Years Survival after Repeated Transcatheter Arterial Chemoembolization Therapy -