Korean J Radiol.
2009 Dec;10(6):623-631. 10.3348/kjr.2009.10.6.623.
Typical and Atypical Manifestations of Intrathoracic Sarcoidosis
- Affiliations
-
- 1Department of Radiology, St. Vincent's Hospital, The Catholic University of Korea, Kyunggi-do 442-723, Korea.
- 2Department of Radiology, Incheon St. Mary's Hospital, The Catholic University of Korea, Incheon 403-720, Korea. kjrad@catholic.ac.kr
- 3Department of Pathology, Seoul St. Mary's Hospital, The Catholic University of Korea, Seoul 137-107, Korea.
- KMID: 1102566
- DOI: http://doi.org/10.3348/kjr.2009.10.6.623
Abstract
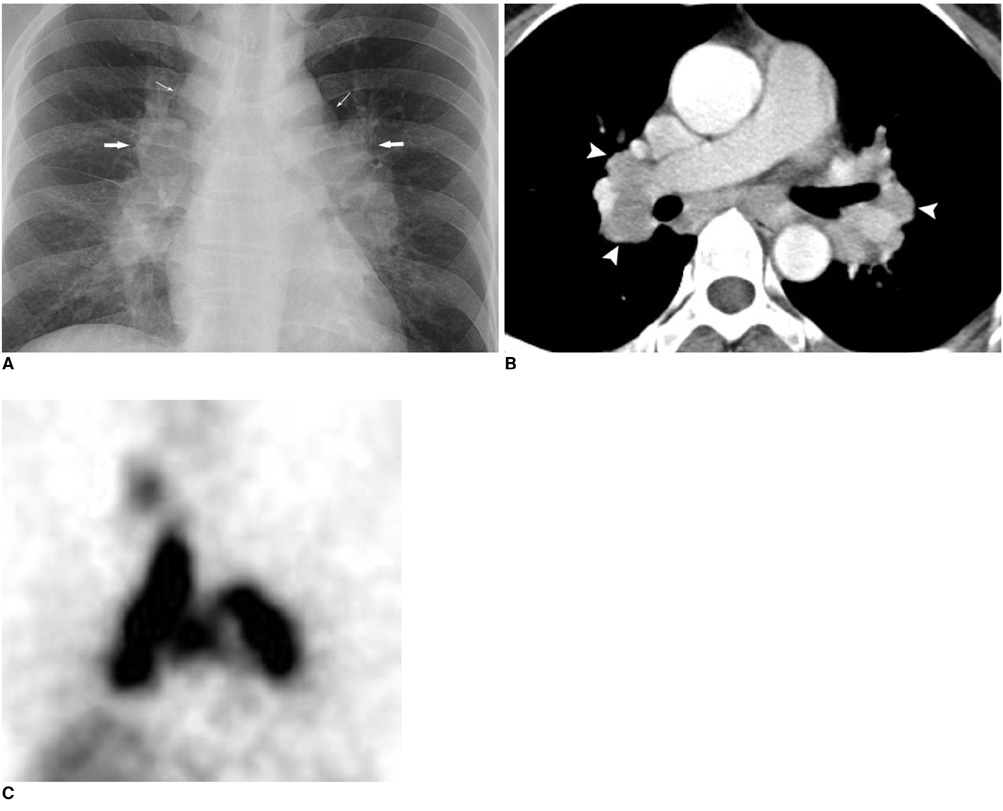
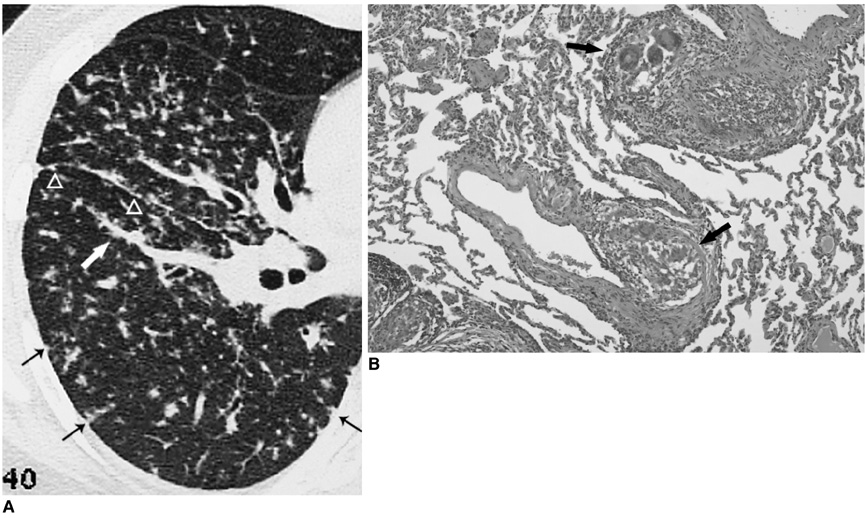
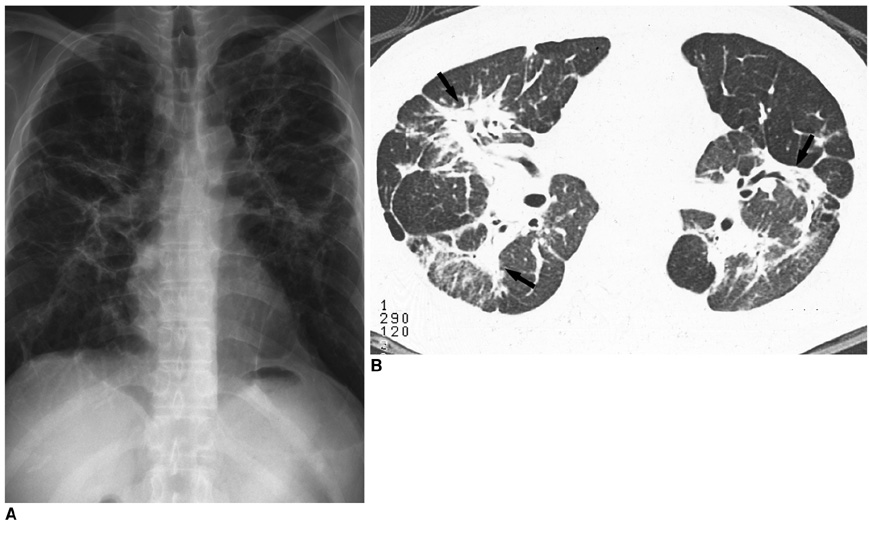
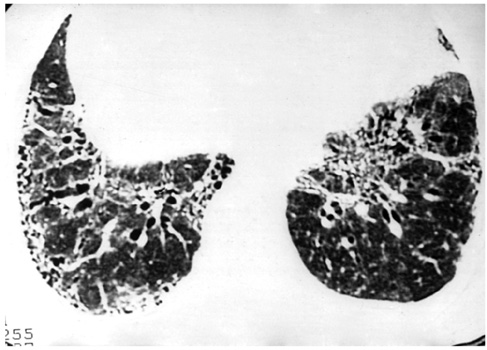
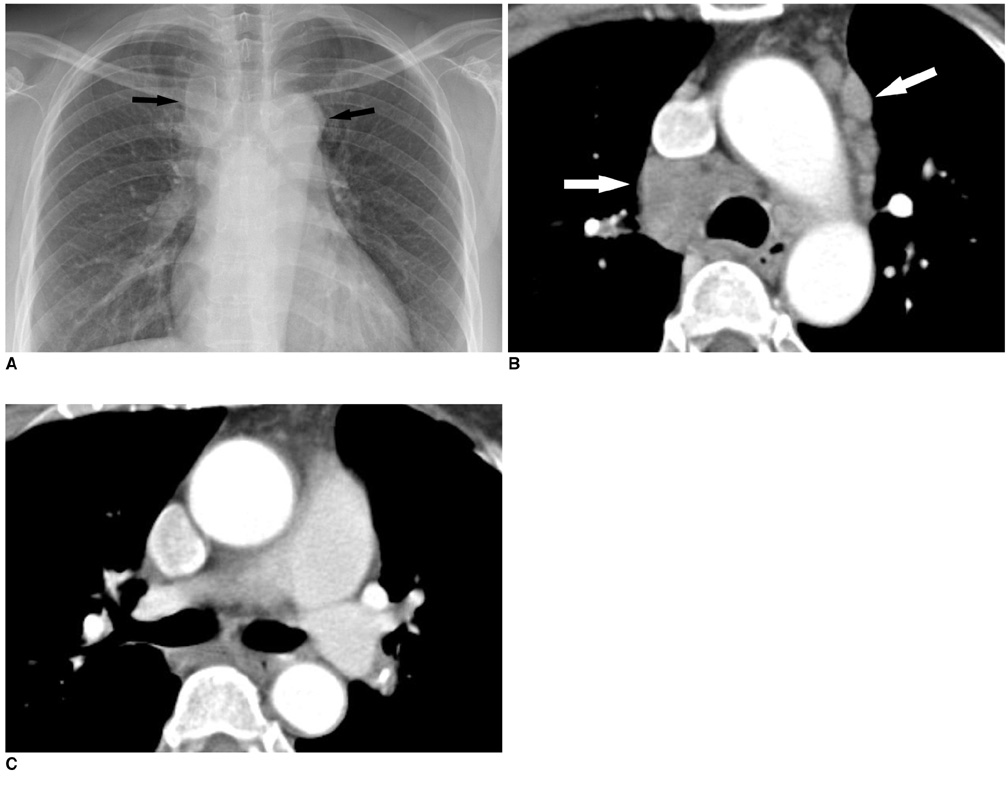
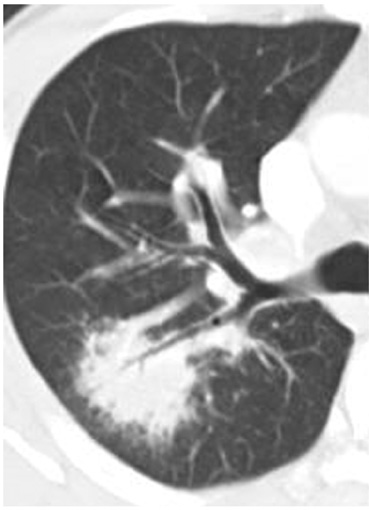
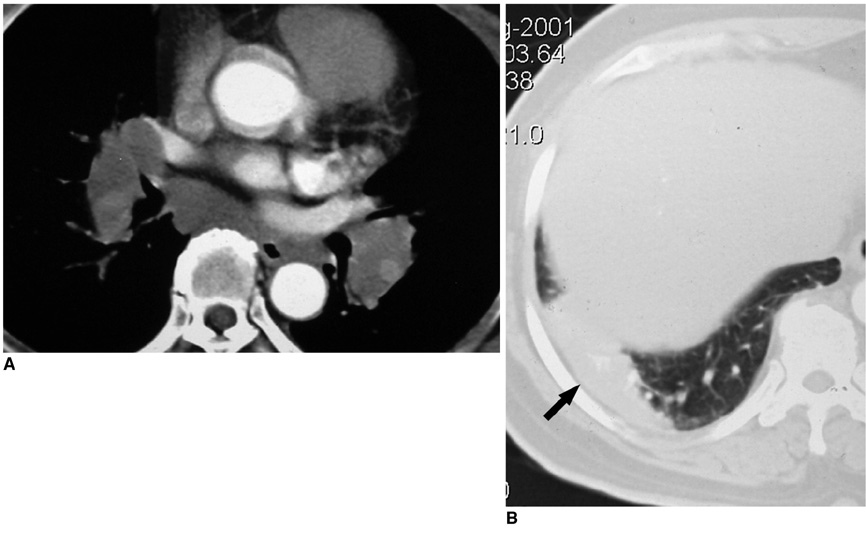
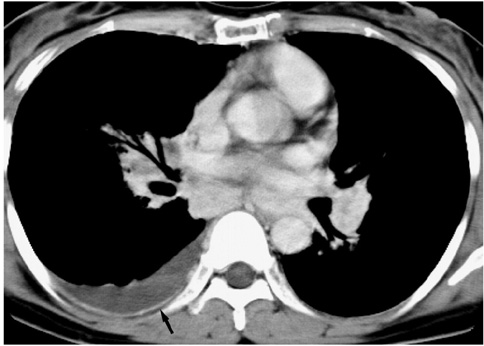
- Sarcoidosis is a systemic disorder of unknown cause that is characterized by the presence of noncaseating granulomas. The radiological findings associated with sarcoidosis have been well described. The findings include symmetric, bilateral hilar and paratracheal lymphadenopathy, with or without concomitant parenchymal abnormalities (multiple small nodules in a peribronchovascular distribution along with irregular thickening of the interstitium). However, in 25% to 30% of cases, the radiological findings are atypical and unfamiliar to most radiologists, which cause difficulty for making a correct diagnosis. Many atypical forms of intrathoracic sarcoidosis have been described sporadically. We have collected cases with unusual radiological findings associated with pulmonary sarcoidosis (unilateral or asymmetric lymphadenopathy, necrosis or cavitation, large opacity, ground glass opacity, an airway abnormality and pleural involvement) and describe the typical forms of the disorder as well. The understanding of a wide range of the radiological manifestations of sarcoidosis will be very helpful for making a proper diagnosis.
Keyword
MeSH Terms
Figure
Reference
-
1. Colby TV, Carrington CB. Thurlbeck WM, editor. Infiltrative lung disease. Pathology of the lung. 1988. Stuttgart: Thieme Medical;425–517.2. Müller NL, Kullnig P, Miller RR. The CT findings of pulmonary sarcoidosis: analysis of 25 patients. AJR Am J Roentgenol. 1989. 152:1179–1182.3. Koyama T, Ueda H, Togashi K, Umeoka S, Kataoka M, Nagai S. Radiologic manifestations of sarcoidosis in various organs. Radiographics. 2004. 24:87–104.4. Hamper UM, Fishman EK, Khouri NF, Johns CJ, Wang KP, Siegelman SS. Typical and atypical CT manifestations of pulmonary sarcoidosis. J Comput Assist Tomogr. 1986. 10:928–936.5. Rockoff SD, Rohatgi PK. Unusual manifestations of thoracic sarcoidosis. AJR Am J Roentgenol. 1985. 144:513–528.6. Baughman RP, Teirstein AS, Judson MA, Rossman MD, Yeager H Jr, Bresnitz EA, et al. Clinical characteristics of patients in a case control study of sarcoidosis. Am J Respir Crit Care Med. 2001. 164:1885–1889.7. Sulavik SB, Spencer RP, Weed DA, Shapiro HR, Shiue ST, Castriotta RJ. Recognition of distinctive patterns of gallium-67 distribution in sarcoidosis. J Nucl Med. 1990. 31:1909–1914.8. Conant EF, Glickstein MF, Mahar P, Miller WT. Pulmonary sarcoidosis in the older patient: conventional radiographic features. Radiology. 1988. 169:315–319.9. Miller BH, Rosado-de-Christenson ML, McAdams HP, Fishback NF. Thoracic sarcoidosis: radiologic-pathologic correlation. Radiographics. 1995. 15:421–437.10. Nakatsu M, Hatabu H, Morikawa K, Uematsu H, Ohno Y, Nishimura K, et al. Large coalescent parenchymal nodules in pulmonary sarcoidosis: "sarcoid galaxy" sign. AJR Am J Roentgenol. 2002. 178:1389–1393.11. Rohatgi PK, Schwab LE. Primary acute pulmonary cavitation in sarcoidosis. AJR Am J Roentgenol. 1980. 134:1199–1203.12. Nishimura K, Itoh H, Kitaichi M, Nagai S, Izumi T. Pulmonary sarcoidosis: correlation of CT and histopathologic findings. Radiology. 1993. 189:105–109.13. Huggins JT, Doelken P, Sahn SA, King L, Judson MA. Pleural effusions in a series of 181 outpatients with sarcoidosis. Chest. 2006. 129:1599–1604.