Korean J Radiol.
2009 Dec;10(6):604-612. 10.3348/kjr.2009.10.6.604.
Usefulness of a Small-Field Digital Mammographic Imaging System Using Parabolic Polycapillary Optics as a Diagnostic Imaging Tool: a Preliminary Study
- Affiliations
-
- 1Department of Radiological Science, Catholic University of Daegu, Gyeongbuk 712-702, Korea.
- 2Department of Radiology and Institute for Radiological Imaging Science, Wonkwang University, Jeonbuk 570-749, Korea. khy1646@wonkwang.ac.kr
- 3Department of Pathology, Wonkwang University, Jeonbuk 570-749, Korea.
- KMID: 1102564
- DOI: http://doi.org/10.3348/kjr.2009.10.6.604
Abstract
OBJECTIVE
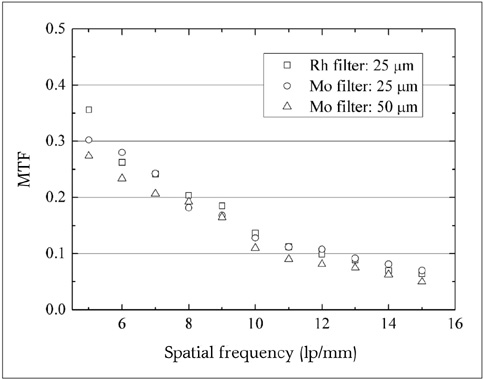
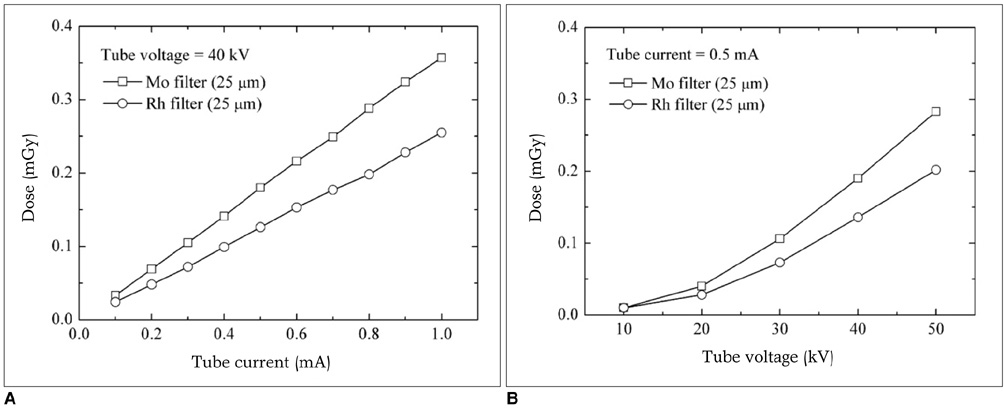
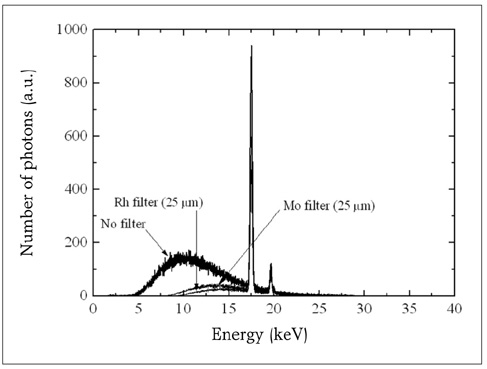
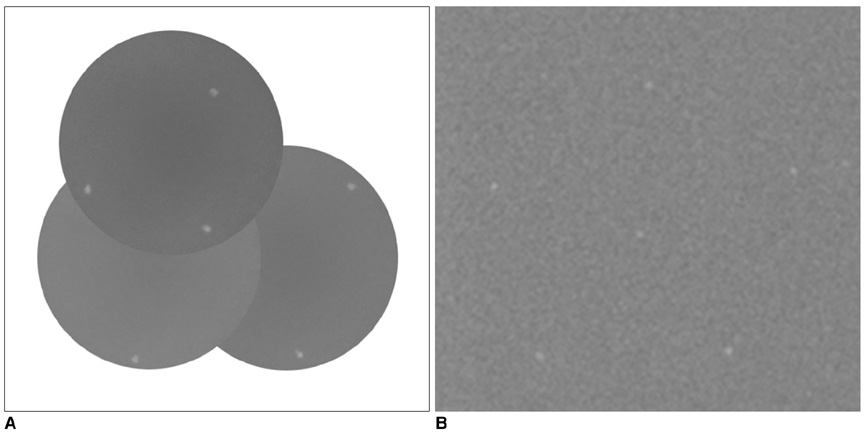
To evaluate the efficacy for spatial resolution and radiation dose of a small-field digital mammographic imaging system using parabolic polycapillary optics. MATERIALS AND METHODS: We developed a small-field digital mammographic imaging system composed of a CCD (charge coupled device) detector and an X-ray source coupled with parabolic polycapillary optics. The spatial resolution and radiation dose according to various filters were evaluated for a small-field digital mammographic imaging system. The images of a test standard phantom and breast cancer tissue sample were obtained. RESULTS: The small-field digital mammographic imaging system had spatial resolutions of 12 lp/mm with molybdenum and rhodium filters with a 25-micrometer thickness. With a thicker molybdenum filter (100 micrometer thick), the system had a higher spatial resolution of 11 lp/mm and contrast of 0.48. The radiation dose for a rhodium filter with a 25-micrometer thickness was 0.13 mGy within a 10-mm-diameter local field. A larger field image greater than 10 mm in diameter could be obtained by scanning an object. On the small-field mammographic imaging system, microcalcifications of breast cancer tissue were clearly observed. CONCLUSION: A small-field digital mammographic imaging system with parabolic polycapillary optics may be a useful diagnostic tool for providing high-resolution imaging with a low radiation dose for examination of local volumes of breast tissue.
MeSH Terms
Figure
Reference
-
1. American Cancer Society. Cancer facts and figures 2003. 2003. Atlanta:2. Stoutjesdijk MJ, Boetes C, Jager GJ, Beex L, Bult P, Hendriks JH, et al. Magnetic resonance imaging and mammography in women with a hereditary risk of breast cancer. J Natl Cancer Inst. 2001. 93:1095–1102.3. Cady B, Steele GD Jr, Morrow M, Gardner B, Smith BL, Lee NC, et al. Evaluation of common breast problems: guidance for primary care providers. CA Cancer J Clin. 1998. 48:49–63.4. Elmore JG, Armstrong K, Lehman CD, Fletcher SW. Screening for breast cancer. JAMA. 2005. 293:1245–1256.5. Pisano ED, Gatsonis C, Hendrick E, Yaffe M, Baum JK, Acharyya S, et al. Diagnostic performance of digital versus film mammography for breast-cancer screening. N Engl J Med. 2005. 353:1773–1783.6. Pisano ED, Yaffe MJ. Digital mammography. Radiology. 2005. 234:353–362.7. Abreu CC, Kruger DG, MacDonald CA, Mistretta CA, Peppler WW, Xiao QF. Measurements of capillary X-ray optics with potential for use in mammographic imaging. Med Phys. 1995. 22:1793–1801.8. Bradford CD, Peppler WW, Ross RE. Multitapered X-ray capillary optics for mammography. Med Phys. 2002. 29:1097–1108.9. Kruger DG, Abreu CC, Hendee EG, Kocharian A, Peppler WW, Mistretta CA, et al. Imaging characteristics of X-ray capillary optics in digital mammography. Med Phys. 1996. 23:187–196.10. Kumakhov MA. Channeling of photons and new X-ray optics. Nucl Instrum Methods Phy Res B. 1990. 48:283–286.11. MacDonald CA, Gibson WM. Applications and advances in polycapillary optics. X-Ray Spectrom. 2003. 32:258–268.12. Bushberg JT, Seibert JA, Leidholdt EM Jr, Boone JM. The essential physics of medical imaging. 2001. 2nd ed. Lippincott Williams & Wilkins.13. Wu X, Barnes GT, Tucker DM. Spectral dependence of grandular tissue dose in screen-film mammography. Radiology. 1991. 179:143–148.14. Sobol WT, Wu X. Parametrization of mammography normalized average glandular dose tables. Med Phys. 1997. 24:547–554.15. American College of Radiology. Mammography Quality Control Manual. 1999. Washington DC: American College of Radiology.16. Attwood D. Soft X-ray and extreme ultraviolet radiation: principle and applications. 2000. Cambridge University Press.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Magnetic Resonance Imaging Meets Fiber Optics: a Brief Investigation of Multimodal Studies on Fiber OpticsBased Diagnostic / Therapeutic Techniques and Magnetic Resonance Imaging
- Principles of Adaptive Optics and Clinical Applications
- Comparison of Image Quality between Mammography Dedicated Monitor and UHD 4K Monitor, Using Standard Mammographic Phantom: A Preliminary Study
- Postoperative Evaluation of Lumbar Disc Herniation Using Digital Infrared Thermographic Imaging
- Clinical Efficacy of Digital Infrared Thermographic Imaging in Multiple Lumbar Disc Herniations