Korean J Radiol.
2009 Dec;10(6):587-595. 10.3348/kjr.2009.10.6.587.
The Incidence and Anatomy of Accessory Pudendal Arteries as Depicted on Multidetector-Row CT Angiography: Clinical Implications of Preoperative Evaluation for Laparoscopic and Robot-Assisted Radical Prostatectomy
- Affiliations
-
- 1Department of Radiology, Anam Hospital, Korea University, College of Medicine, Korea. urorad@korea.ac.kr
- 2Department of Urology, Anam Hospital, Korea University, College of Medicine, Korea.
- KMID: 1102562
- DOI: http://doi.org/10.3348/kjr.2009.10.6.587
Abstract
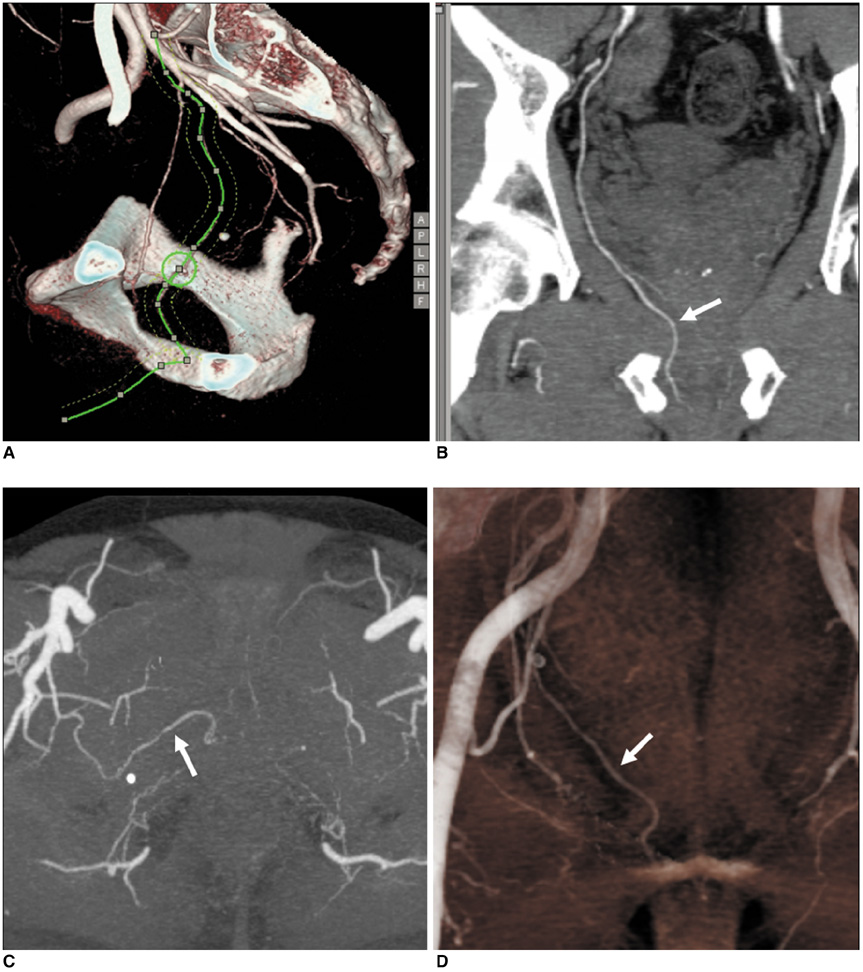
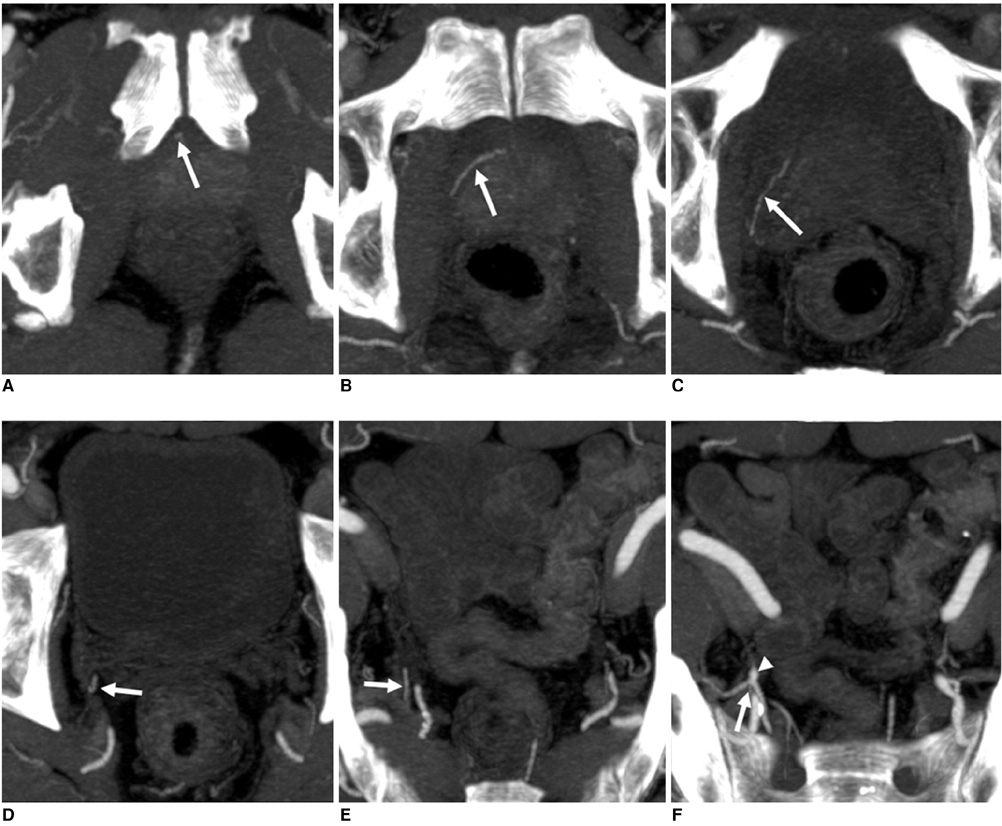
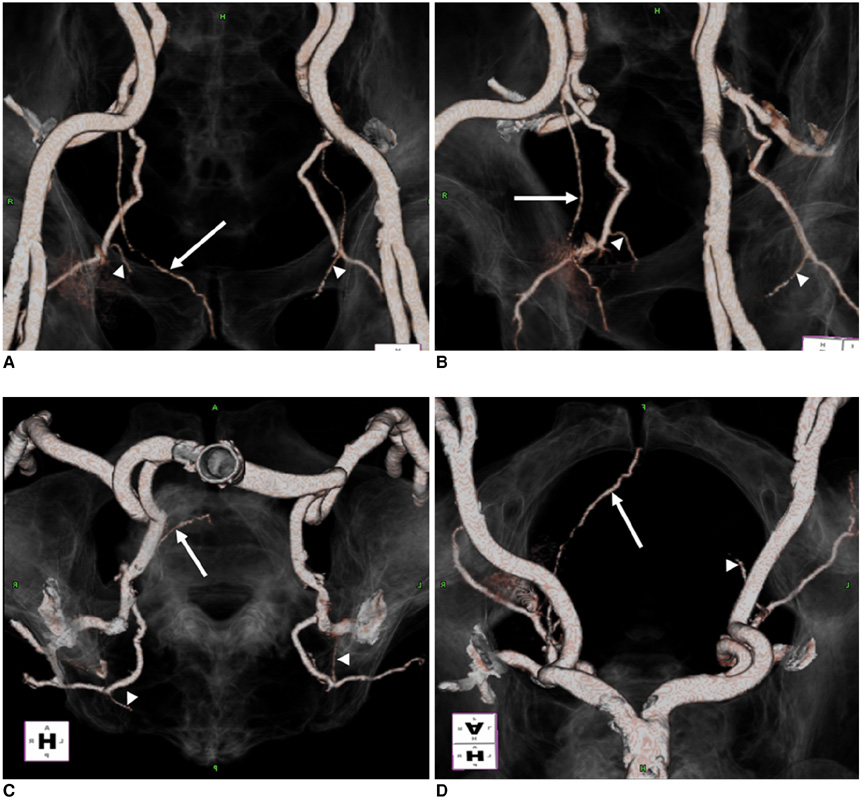
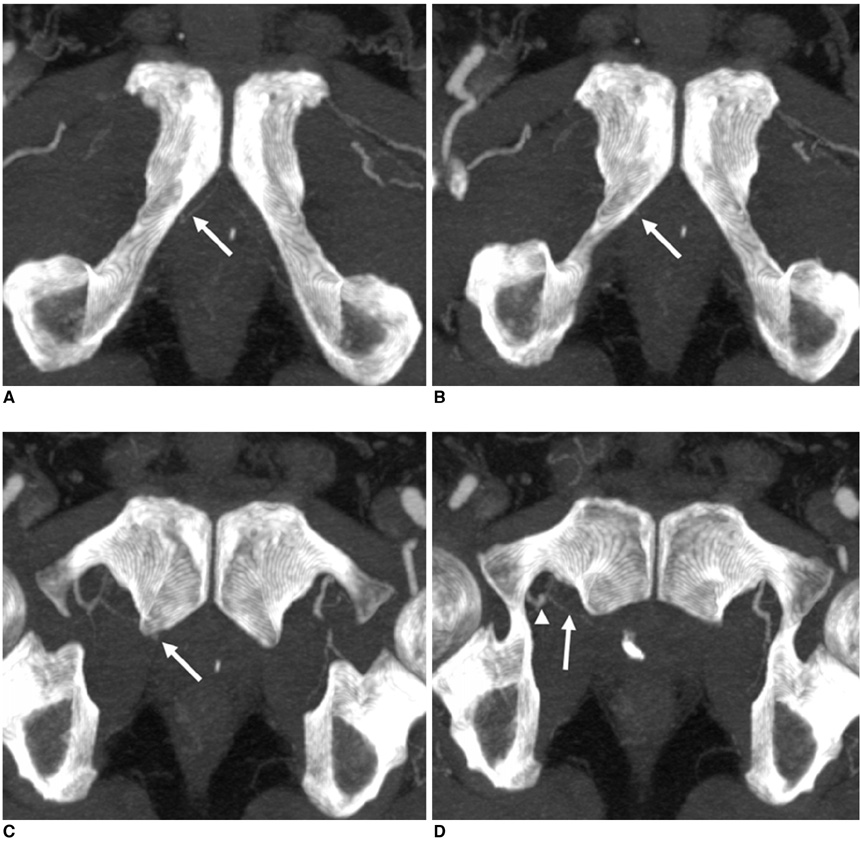
OBJECTIVE
To help preserve accessory pudendal arteries (APAs) and to ensure optimal postoperative sexual function after a laparoscopic or robot-assisted radical prostatectomy, we have evaluated the incidence of APAs as detected on multidetector-row CT (MDCT) angiography and have provided a detailed anatomical description. MATERIALS AND METHODS: The distribution of APAs was evaluated in 121 consecutive male patients between February 2006 and July 2007 who underwent 64-channel MDCT angiography of the lower extremities. We defined an APA as any artery located within the periprostatic region running parallel to the dorsal vascular complex. We also subclassified APAs into lateral and apical APAs. Two radiologists retrospectively evaluated the origin, course and number of APAs; the final APA subclassification based on MDCT angiography source data was determined by consensus. RESULTS: We identified 44 APAs in 36 of 121 patients (30%). Two distinct varieties of APAs were identified. Thirty-three APAs (75%) coursed near the anterolateral region of the prostatic apex, termed apical APAs. The remaining 11 APAs (25%) coursed along the lateral aspect of the prostate, termed lateral APAs. All APAs originated from the internal obturator artery and iliac artery or a branch of the iliac artery such as the inferior vesical artery. The majority of apical APAs arose from the internal obturator artery (84%). Seven patients (19%) had multiple APAs. CONCLUSION: APAs are more frequently detected by the use of MDCT angiography than as suggested by previous surgical studies. The identification of APAs on MDCT angiography may provide useful information for the surgical preservation of APAs during a laparoscopic or robot-assisted radical prostatectomy.
Keyword
MeSH Terms
Figure
Reference
-
1. Jemal A, Siegel R, Ward E, Hao Y, Xu J, Murray T, et al. Cancer statistics, 2008. CA Cancer J Clin. 2008. 58:71–96.2. Hsing AW, Tsao L, Devesa SS. International trends and patterns of prostate cancer incidence and mortality. Int J Cancer. 2000. 85:60–67.3. Merrill RM, Stephenson RA. Trends in mortality rates in patients with prostate cancer during the era of prostate specific antigen screening. J Urol. 2000. 163:503–510.4. Parker SL, Tong T, Bolden S, Wingo PA. Cancer statistics, 1996. CA Cancer J Clin. 1996. 46:5–27.5. Walsh PC, Donker PJ. Impotence following radical prostatectomy: insight into etiology and prevention. J Urol. 1982. 128:492–497.6. Walsh PC, Lepor H, Eggleston JC. Radical prostatectomy with preservation of sexual function: anatomical and pathological considerations. Prostate. 1983. 4:473–485.7. Potosky AL, Davis WW, Hoffman RM, Stanford JL, Stephenson RA, Penson DF, et al. Five-year outcomes after prostatectomy or radiotherapy for prostate cancer: the prostate cancer outcomes study. J Natl Cancer Inst. 2004. 96:1358–1367.8. Aboseif S, Shinohara K, Breza J, Benard F, Narayan P. Role of penile vascular injury in erectile dysfunction after radical prostatectomy. Br J Urol. 1994. 73:75–82.9. Droupy S, Hessel A, Benoit G, Blanchet P, Jardin A, Giuliano F. Assessment of the functional role of accessory pudendal arteries in erection by transrectal color Doppler ultrasound. J Urol. 1999. 162:1987–1991.10. Kim ED, Blackburn D, McVary KT. Post-radical prostatectomy penile blood flow: assessment with color flow Doppler ultrasound. J Urol. 1994. 152:2276–2279.11. Polascik TJ, Walsh PC. Radical retropubic prostatectomy: the influence of accessory pudendal arteries on the recovery of sexual function. J Urol. 1995. 154:150–152.12. Rogers CG, Trock BP, Walsh PC. Preservation of accessory pudendal arteries during radical retropubic prostatectomy: surgical technique and results. Urology. 2004. 64:148–151.13. Rosen MP, Greenfield AJ, Walker TG, Grant P, Guben JK, Dubrow J, et al. Arteriogenic impotence: findings in 195 impotent men examined with selective internal pudendal angiography. Young Investigator's Award. Radiology. 1990. 174:1043–1048.14. Secin FP, Karanikolas N, Kuroiwa K, Vickers A, Touijer K, Guillonneau B. Positive surgical margins and accessory pudendal artery preservation during laparoscopic radical prostatectomy. Eur Urol. 2005. 48:786–792.15. Matin SF. Recognition and preservation of accessory pudendal arteries during laparoscopic radical prostatectomy. Urology. 2006. 67:1012–1015.16. Graefen M, Walz J, Huland H. Open retropubic nerve-sparing radical prostatectomy. Eur Urol. 2006. 49:38–48.17. Touijer K, Guillonneau B. Laparoscopic radical prostatectomy: a critical analysis of surgical quality. Eur Urol. 2006. 49:625–632.18. Rassweiler J. Open vs. laparoscopic radical prostatectomy... and laparoscopy is better! Eur Urol. 2006. 50:26–28.19. Rassweiler J, Stolzenburg J, Sulser T, Deger S, Zumbe J, Hofmockel G, et al. Laparoscopic radical prostatectomy -- the experience of the German Laparoscopic Working Group. Eur Urol. 2006. 49:113–119.20. Guillonneau B, Vallancien G. Laparoscopic radical prostatectomy: the Montsouris technique. J Urol. 2000. 163:1643–1649.21. Guillonneau B, Vallancien G. Laparoscopic radical prostatectomy: the Montsouris experience. J Urol. 2000. 163:418–422.22. Abbou CC, Salomon L, Hoznek A, Antiphon P, Cicco A, Saint F, et al. Laparoscopic radical prostatectomy: preliminary results. Urology. 2000. 55:630–634.23. Rassweiler J, Safi KC, Subotic S, Teber D, Frede T. Robotics and telesurgery -- an update on their position in laparoscopic radical prostatectomy. Minim Invasive Ther Allied Technol. 2005. 14:109–122.24. Secin FP, Karanikolas N, Touijer AK, Salamanca JI, Vickers AJ, Guillonneau B. Anatomy of accessory pudendal arteries in laparoscopic radical prostatectomy. J Urol. 2005. 174:523–526.25. Gray RR, Keresteci AG, St Louis EL, Grosman H, Jewett MA, Rankin JT, et al. Investigation of impotence by internal pudendal angiography: experience with 73 cases. Radiology. 1982. 144:773–780.26. Breza J, Aboseif SR, Orvis BR, Lue TF, Tanagho EA. Detailed anatomy of penile neurovascular structures: surgical significance. J Urol. 1989. 141:437–443.27. Benoit G, Droupy S, Quillard J, Paradis V, Giuliano F. Supra and infralevator neurovascular pathways to the penile corpora cavernosa. J Anat. 1999. 195:605–615.28. Secin FP, Touijer K, Mulhall J, Guillonneau B. Anatomy and preservation of accessory pudendal arteries in laparoscopic radical prostatectomy. Eur Urol. 2007. 51:1229–1235.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Erratum: Robot-Assisted Laparoscopic Radical Prostatectomy
- A Case of Robot-Assisted Laparoscopic Radical Prostatectomy in Primary Small Cell Prostate Cancer
- Multidetector-row CT Angiography of Hepatic Artery: Comparison with Conventional Angiography
- Robot-Assisted Laparoscopic Radical Prostatectomy
- Floating Hem-o-Lok Clips in the Bladder without Stone Formation after Robot-Assisted Laparoscopic Radical Prostatectomy