Korean J Radiol.
2009 Oct;10(5):455-463. 10.3348/kjr.2009.10.5.455.
Feasibility of Automated Quantification of Regional Disease Patterns Depicted on High-Resolution Computed Tomography in Patients with Various Diffuse Lung Diseases
- Affiliations
-
- 1Department of Radiology and Research Institute of Radiology, University of Ulsan College of Medicine, Asan Medical Center, Seoul 138-736, Korea. joonbeom.seo@gmail.com
- 2Department of Radiology, Wonkwang University Hospital, Jeonbuk 570-749, Korea.
- 3Department of Radiology, East-West Neo Medical Center of Kyunghee University, Seoul 134-727, Korea.
- 4Department of Digital Media, The Catholic University of Korea, Seoul 150-101, Korea.
- 5Department of Industrial Engineering, Engineering College, Seoul National University, Seoul 151-742, Korea.
- KMID: 1093960
- DOI: http://doi.org/10.3348/kjr.2009.10.5.455
Abstract
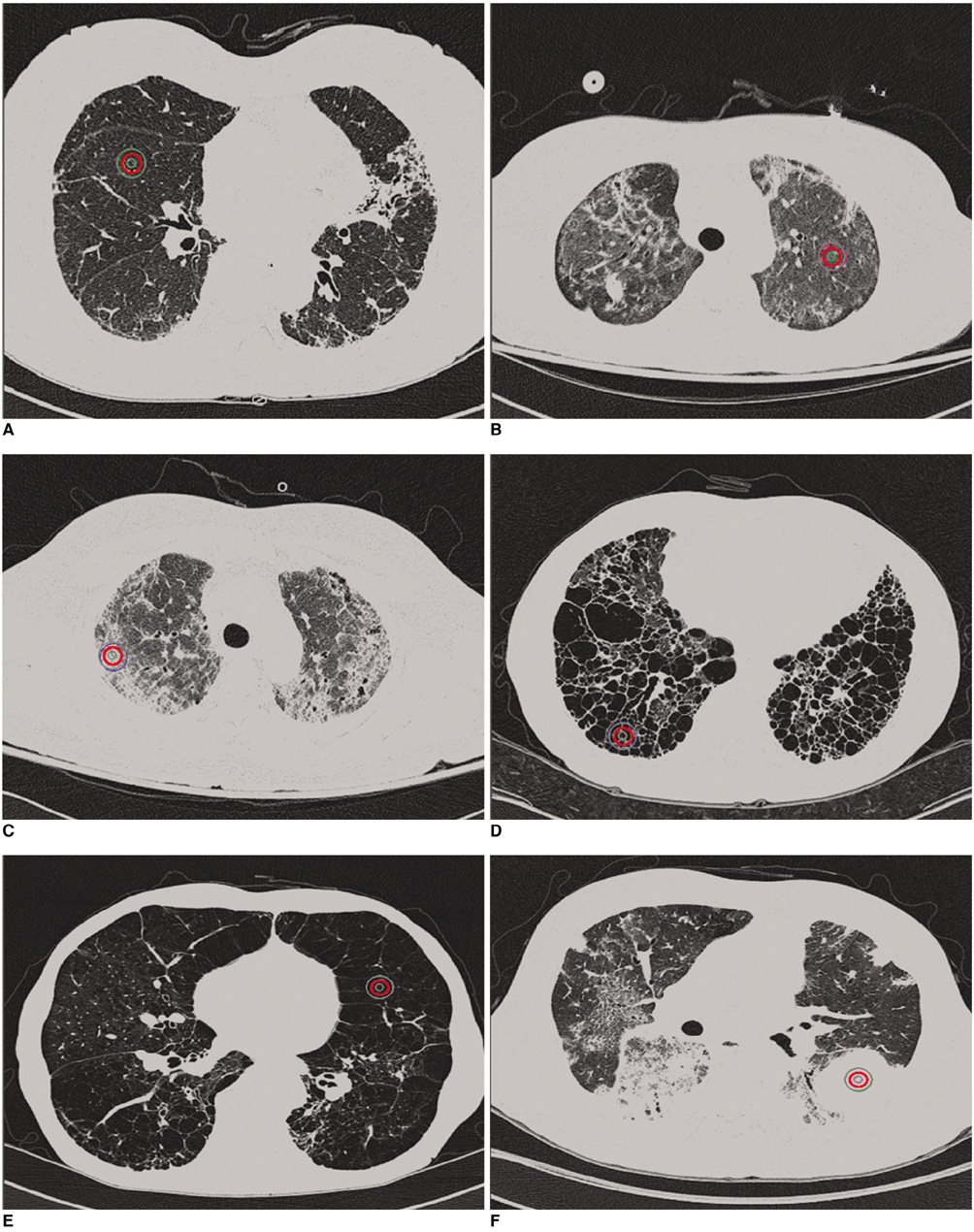
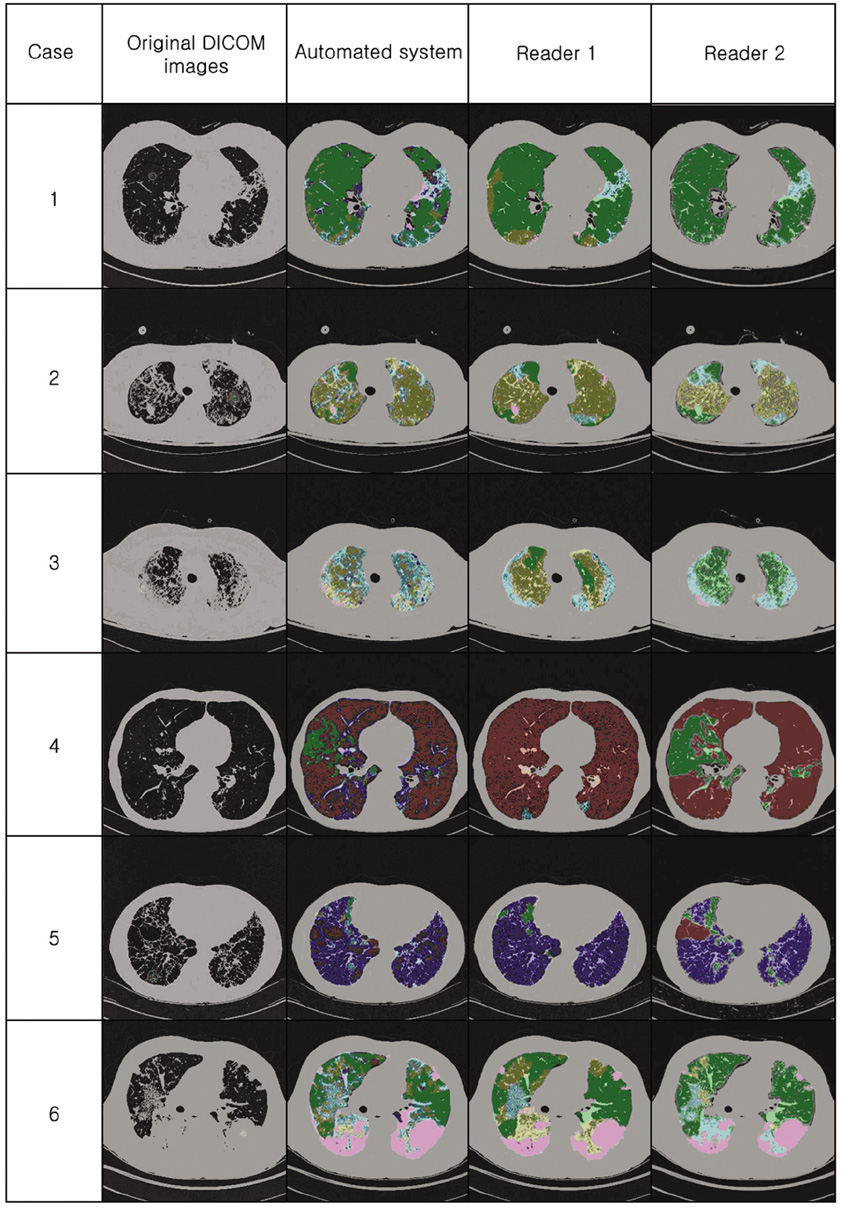
OBJECTIVE
This study was designed to develop an automated system for quantification of various regional disease patterns of diffuse lung diseases as depicted on high-resolution computed tomography (HRCT) and to compare the performance of the automated system with human readers. MATERIALS AND METHODS: A total of 600 circular regions-of-interest (ROIs), 10 pixels in diameter, were utilized. The 600 ROIs comprised 100 ROIs that represented six typical regional patterns (normal, ground-glass opacity, reticular opacity, honeycombing, emphysema, and consolidation). The ROIs were used to train the automated classification system based on the use of a Support Vector Machine classifier and 37 features of texture and shape. The performance of the classification system was tested with a 5-fold cross-validation method. An automated quantification system was developed with a moving ROI in the lung area, which helped classify each pixel into six categories. A total of 92 HRCT images obtained from patients with different diseases were used to validate the quantification system. Two radiologists independently classified lung areas of the same CT images into six patterns using the manual drawing function of dedicated software. Agreement between the automated system and the readers and between the two individual readers was assessed. RESULTS: The overall accuracy of the system to classify each disease pattern based on the typical ROIs was 89%. When the quantification results were examined, the average agreement between the system and each radiologist was 52% and 49%, respectively. The agreement between the two radiologists was 67%. CONCLUSION: An automated quantification system for various regional patterns of diffuse interstitial lung diseases can be used for objective and reproducible assessment of disease severity.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
An Engineering View on Megatrends in Radiology: Digitization to Quantitative Tools of Medicine
Namkug Kim, Jaesoon Choi, Jaeyoun Yi, Seungwook Choi, Seyoun Park, Yongjun Chang, Joon Beom Seo
Korean J Radiol. 2013;14(2):139-153. doi: 10.3348/kjr.2013.14.2.139.
Reference
-
1. Hoffman EA, Reinhardt JM, Sonka M, Simon BA, Guo J, Saba O, et al. Characterization of the interstitial lung diseases via density-based and texture-based analysis of computed tomography images of lung structure and function. Acad Radiol. 2003. 10:1104–1118.2. Scatarige JC, Diette GB, Haponik EF, Merriman B, Fishman EK. Utility of high-resolution CT for management of diffuse lung disease: results of a survey of U.S. pulmonary physicians. Acad Radiol. 2003. 10:167–175.3. Gay SE, Kazerooni EA, Toews GB, Lynch JP 3rd, Gross BH, Cascade PN, et al. Idiopathic pulmonary fibrosis: predicting response to therapy and survival. Am J Respir Crit Care Med. 1998. 157:1063–1072.4. Delorme S, Keller-Reichenbecher MA, Zuna I, Schlegel W, Van Kaick G. Usual interstitial pneumonia. Quantitative assessment of high-resolution computed tomography findings by computer-assisted texture-based image analysis. Invest Radiol. 1997. 32:566–574.5. Sluimer IC, van Waes PF, Viergever MA, van Ginneken B. Computer-aided diagnosis in high resolution CT of the lungs. Med Phys. 2003. 30:3081–3090.6. Sumikawa H, Johkoh T, Yamamoto S, Takahei K, Ueguchi T, Ogata Y, et al. Quantitative analysis for computed tomography findings of various diffuse lung diseases using volume histogram analysis. J Comput Assist Tomogr. 2006. 30:244–249.7. Uchiyama Y, Katsuragawa S, Abe H, Shiraishi J, Li F, Li Q, et al. Quantitative computerized analysis of diffuse lung disease in high-resolution computed tomography. Med Phys. 2003. 30:2440–2454.8. Uppaluri R, Hoffman EA, Sonka M, Hartley PG, Hunninghake GW, McLennan G. Computer recognition of regional lung disease patterns. Am J Respir Crit Care Med. 1999. 160:648–654.9. Uppaluri R, Hoffman EA, Sonka M, Hunninghake GW, McLennan G. Interstitial lung disease: a quantitative study using the adaptive multiple feature method. Am J Respir Crit Care Med. 1999. 159:519–525.10. Xu Y, van Beek EJ, Hwanjo Y, Guo J, McLennan G, Hoffman EA. Computer-aided classification of interstitial lung diseases via MDCT: 3D adaptive multiple feature method (3D AMFM). Acad Radiol. 2006. 13:969–978.11. Park YS, Seo JB, Kim N, Chae EJ, Oh YM, Lee SD, et al. Texture-based quantification of pulmonary emphysema on high-resolution computed tomography: comparison with density-based quantification and correlation with pulmonary function test. Invest Radiol. 2008. 43:395–402.12. Kim N, Seo JB, Lee Y, Lee JG, Kim SS, Kang SH. Development of an automatic classification system for differentiation of obstructive lung disease using HRCT. J Digit Imaging. 2009. 22:136–148.13. Lee Y, Seo JB, Lee JG, Kim SS, Kim N, Kang SH. Performance testing of several classifiers for differentiating obstructive lung diseases based on texture analysis at high-resolution computerized tomography (HRCT). Comput Methods Programs Biomed. 2009. 93:206–215.14. Nishimura K, Izumi T, Kitaichi M, Nagai S, Itoh H. The diagnostic accuracy of high-resolution computed tomography in diffuse infiltrative lung diseases. Chest. 1993. 104:1149–1155.15. Padley SP, Hansell DM, Flower CD, Jennings P. Comparative accuracy of high resolution computed tomography and chest radiography in the diagnosis of chronic diffuse infiltrative lung disease. Clin Radiol. 1991. 44:222–226.16. Collins CD, Wells AU, Hansell DM, Morgan RA, MacSweeney JE, du Bois RM, et al. Observer variation in pattern type and extent of disease in fibrosing alveolitis on thin section computed tomography and chest radiography. Clin Radiol. 1994. 49:236–240.17. Remy-Jardin M, Remy J, Wallaert B, Bataille D, Hatron PY. Pulmonary involvement in progressive systemic sclerosis: sequential evaluation with CT, pulmonary function tests, and bronchoalveolar lavage. Radiology. 1993. 188:499–506.18. Ko JP, Naidich DP. Computer-aided diagnosis and the evaluation of lung disease. J Thorac Imaging. 2004. 19:136–155.19. Ashizawa K, Ishida T, MacMahon H, Vyborny CJ, Katsuragawa S, Doi K. Artificial neural networks in chest radiography: application to the differential diagnosis of interstitial lung disease. Acad Radiol. 1999. 6:2–9.20. Hartley PG, Galvin JR, Hunninghake GW, Merchant JA, Yagla SJ, Speakman SB, et al. High-resolution CT-derived measures of lung density are valid indexes of interstitial lung disease. J Appl Physiol. 1994. 76:271–277.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- DILD (diffuse infiltrative lung disease); Radiologic Diagnostic Approach According to High-Resolution CT Pattern
- Radiologic Approach to Diffuse Infiltrative Lung Disease
- The Role of Open Lung Biopsy in Diagnosis and Treatment of Diffuse Interstitial Lung Disease in High-resolution Computed Tomography Era
- Application and Interpretation of High-Resolution Computed Tomography for the Diagnosis of Interstitial Lung Disease (ILD): ILD Protocol
- Comparison of Usual Interstitial Pneumonia and Nonspecific Interstitial Pneumonia: Quantification of Disease Severity and Discrimination between Two Diseases on HRCT Using a Texture-Based Automated System