Korean J Radiol.
2009 Oct;10(5):441-446. 10.3348/kjr.2009.10.5.441.
Ultrasound-Guided Fine-Needle Aspiration Biopsy of Thyroid Nodules: is it Necessary to Use Local Anesthesia for the Application of One Needle Puncture?
- Affiliations
-
- 1Department of Radiology, Busan Paik Hospital, Inje University College of Medicine, Pusan 614-735, Korea.
- 2Department of Radiology, Myongji Hospital, Kwandong University College of Medicine, Kyunggi 412-270, Korea. rmh96@dreamwiz.com
- 3Department of Radiology, College of Medicine, Dong-A University, Pusan 602-715, Korea.
- KMID: 1093958
- DOI: http://doi.org/10.3348/kjr.2009.10.5.441
Abstract
OBJECTIVE
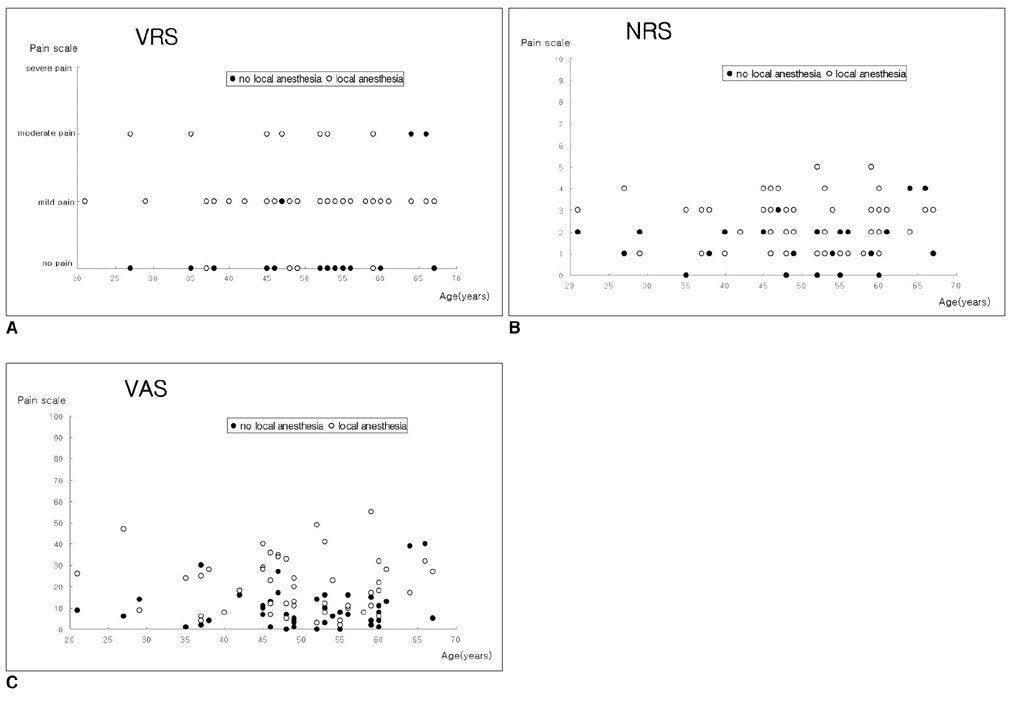
This study was designed to evaluate the difference in the degree of patient pain for an ultrasound-guided fine-needle aspiration biopsy (USFNAB) of a thyroid nodule with one needle puncture with and without local anesthesia. MATERIALS AND METHODS: A total of 50 patients participated in the study. We examined prospective patients who would undergo US-FNABs of two thyroid nodules (larger than 10 mm maximum diameter), which were located in separate thyroid lobes. For one of these thyroid nodules, US-FNAB was performed following the administration of local anesthesia; for the other nodule, no anesthesia was administered. The application of anesthesia was alternatively administered between patients (either prior to the first US-FNAB procedure or prior to the second procedure). For all patients, the degree of pain during and after each US-guided FNAB was evaluated according to a 4-category verbal rating scale (VRS), an 11-point numeric rating scale (NRS) and a 100-mm visual analogue scale (VAS). RESULTS: The mean maximum diameters of thyroid nodules examined by US-FNAB with the use of local anesthesia and with no local anesthesia were 13.6 mm and 13.0 mm, respectively. There was no significant difference in nodule size (p > 0.05) between two groups. For the VRS, there were 27 patients with a higher pain score when local anesthesia was used and four patients with a higher pain score when no local anesthesia was administered. Nineteen patients had equivalent pain score for both treatments. This finding was statistically significant (p < 0.001). For the NRS, there were 33 patients with a higher pain score when local anesthesia was used and 10 patients with a higher pain score when no local anesthesia was administered. Seven patients had an equivalent pain score for each treatment. This finding was statistically significant (p < 0.001). For the VAS, there were 35 patients with a higher pain score when local anesthesia was used and 11 patients with a higher pain score where no local anesthesia was administered. Four patients had an equivalent pain score for both treatments. This finding was also statistically significant (p = 0.001). CONCLUSION: In our study, patient pain scales were significantly lower when no local anesthesia was used prior to US-FNABs of thyroid nodules as compared to when local anesthesia was administered. Therefore, we believe that when one needle puncture is used, US-FNAB should be performed without administering local anesthesia.
MeSH Terms
-
Adult
Aged
Anesthesia, Local/*utilization
Biopsy, Fine-Needle/*adverse effects
Female
Humans
Male
Middle Aged
Pain Measurement
Prospective Studies
Punctures/adverse effects
Statistics, Nonparametric
Thyroid Neoplasms/*pathology/ultrasonography
Thyroid Nodule/*pathology/ultrasonography
*Ultrasonography, Interventional
Figure
Reference
-
1. Yokozawa T, Miyauchi A, Kuma K, Sugawara M. Accurate and simple method of diagnosing thyroid nodules the modified technique of ultrasound-guided fine needle aspiration biopsy. Thyroid. 1995. 5:141–145.2. Danese D, Sciacchitano S, Farsetti A, Andreoli M, Pontecorvi A. Diagnostic accuracy of conventional versus sonography-guided fine-needle aspiration biopsy of thyroid nodules. Thyroid. 1998. 8:15–21.3. Rausch P, Nowels K, Jeffrey RB Jr. Ultrasonographically guided thyroid biopsy: a review with emphasis on technique. J Ultrasound Med. 2001. 20:79–85.4. O'Malley ME, Weir MM, Hahn PF, Misdraji J, Wood BJ, Mueller PR. US-guided fine-needle aspiration biopsy of thyroid nodules: adequacy of cytologic material and procedure time with and without immediate cytologic analysis. Radiology. 2002. 222:383–387.5. Brau ME, Nau C, Hempelmann G, Vogel W. Local anesthetics potently block a potential insensitive potassium channel in myelinated nerve. J Gen Physiol. 1995. 105:485–505.6. Donald MJ, Derbyshire S. Lignocaine toxicity; a complication of local anaesthesia administered in the community. Emerg Med J. 2004. 21:249–250.7. McKay W, Morris R, Mushlin P. Sodium bicarbonate attenuates pain on skin infiltration with lidocaine, with or without epinephrine. Anesth Analg. 1987. 66:572–574.8. Christoph RA, Buchanan L, Begalla K, Schwartz S. Pain reduction in local anaesthetic administration through pH buffering. Ann Emerg Med. 1988. 17:117–120.9. Dire DJ, Hogan DE. Double-blinded comparison of diphenhydramine versus lidocaine as a local anesthetic. Ann Emerg Med. 1993. 22:1419–1422.10. Xia Y, Chen E, Tibbits DL, Reilley TE, McSweeney TD. Comparison of effects of lidocaine hydrochloride, buffered lidocaine, diphenhydramine, and normal saline after intradermal injection. J Clin Anesth. 2002. 14:339–343.11. Porter JC, Frizelle FA. Use of local anesthetic agents among New Zealand plastic surgeons - their practices and philosophies. Med Sci Monit. 2000. 6:194–197.12. Bainbridge LC. Comparison of room temperature and body temperature local anaesthetic solutions. Br J Plast Surg. 1991. 44:147–148.13. Davidson JA, Boom SJ. Warming lignocaine to reduce pain associated with injection. BMJ. 1992. 305:617–618.14. Bell RW, Butt ZA. Warming lignocaine reduces the pain of injection during peribulbar local anaesthesis for cataract surgery. Br J Ophthalmol. 1995. 79:1015–1017.15. Allen MJ, Bunce C, Presland AH. The effect of warming local anaesthetic on the pain of injection during sub-Tenon's anaesthesia for cataract surgery. Anaesthesia. 2008. 63:276–278.16. Jensen MP, Chen C, Brugger AM. Interpretation of visual analog scale ratings and change scores: a reanalysis of two clinical trials of postoperative pain. J Pain. 2003. 4:407–414.17. Kim DW, Lee EJ, Kim SH, Kim TH, Lee SH, Kim DH, et al. Ultrasound-guided fine-needle aspiration biopsy of thyroid nodules: comparison in efficacy according to nodule size. Thyroid. 2009. 19:27–31.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Ultrasound-guided Fine-needle Aspiration Biopsy of Thyroid Nodules: Comparison of the Pain Scale according to the Application of Local Anesthesia
- Indications for Fine Needle Aspiration in Thyroid Nodules
- Diagnosis of Parathyroid Adenoma Detected during Thyroid Ultrasound: The Role of Parathormone Measurement in Fine-Needle Aspiration Washout
- Thyroid Nodules with Nondiagnostic FNA Results: Role of Core Needle Biopsy
- Fine-Needle Biopsy: Should This Be the First Choice in Endoscopic Ultrasound-Guided Tissue Acquisition?