Korean J Radiol.
2009 Feb;10(1):12-20. 10.3348/kjr.2009.10.1.12.
Malignant Pure Pulmonary Ground-Glass Opacity Nodules: Prognostic Implications
- Affiliations
-
- 1Department of Radiology and Center for Imaging Science, Sungkyunkwan University School of Medicine, Seoul, Korea. kyungs.lee@samsung.com
- 2Department of Thoracic Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- KMID: 1088673
- DOI: http://doi.org/10.3348/kjr.2009.10.1.12
Abstract
OBJECTIVE
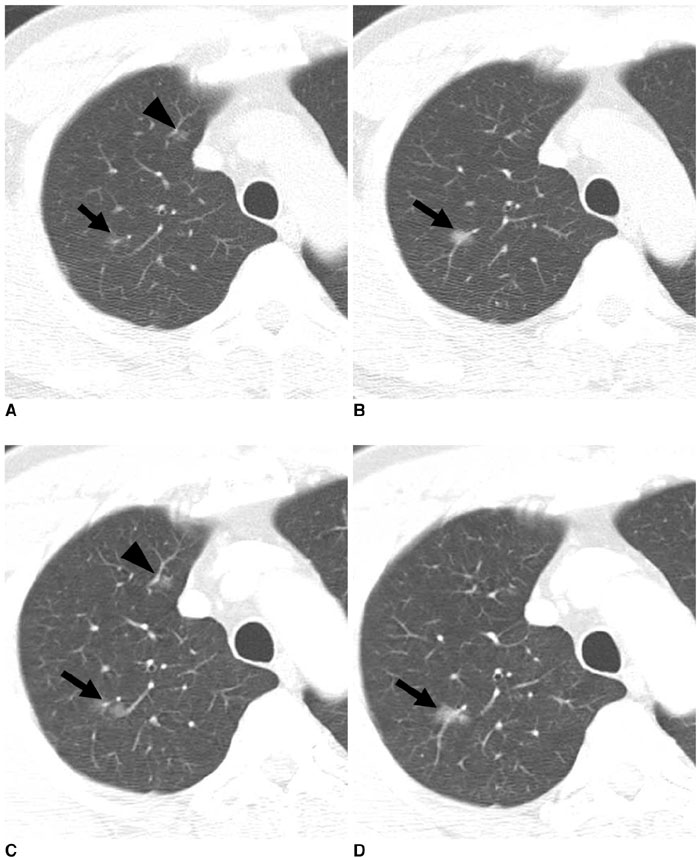
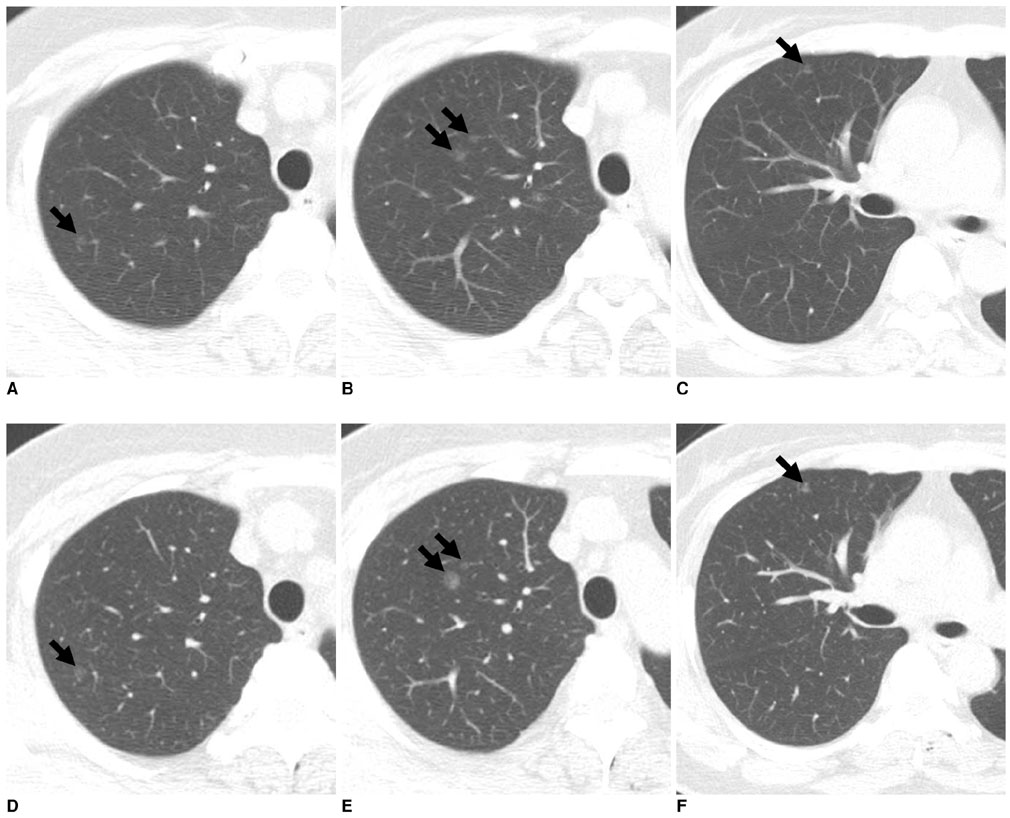
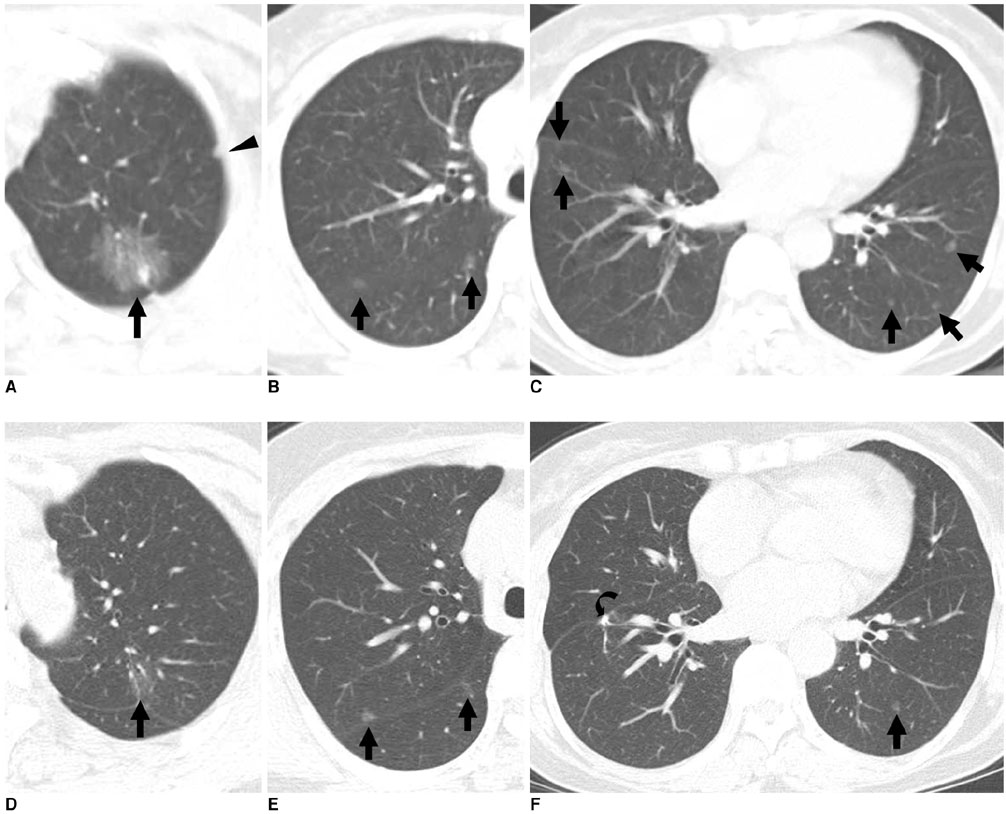
This study was designed to evaluate follow-up results in terms of patient prognosis for malignant pulmonary nodules depicted as pure ground-glass opacity (GGO) lesion observed at high-resolution CT (HRCT). MATERIALS AND METHODS: Surgical removal for malignant GGO nodules was accomplished in 58 patients (26 men, 32 women; mean age, 57 years; age range, 29-78 years). Patient prognoses were assessed by patient clinical status and the presence of changes in nodule size determined after a follow-up HRCT examination. Differences in patient prognoses were compared for nodule number, size, surgical method, change in size before surgical removal, and histopathological diagnosis by use of Fisher's exact test and Pearson's chi-squared test. RESULTS: Of the 58 patients, 40 patients (69%) were confirmed to have a bronchioloalveolar carcinoma (BAC) and 18 patients (31%) were confirmed to have an adenocarcinoma with a predominant BAC component. Irrespective of nodule size, number, treatment method, change in size before surgical removal and histopathological diagnosis, neither local recurrence nor a metastasis occurred in any of these patients as determined at a follow-up period of 24 months (range; 12-65 months). Of 14 patients with multiple GGO nodules, all of the nodules were resected without recurrence in six patients. In the remaining eight patients, the remaining nodules showed no change in size in seven cases and a decrease in size in one case as determined after a follow-up CT examination. CONCLUSION: Prognoses in patients with pure GGO malignant pulmonary nodules are excellent, and not significantly different in terms of nodule number, size, surgical method, presence of size change before surgical removal and histopathological diagnosis.
Keyword
MeSH Terms
-
Adenocarcinoma/pathology/radiography/surgery
Adenocarcinoma, Bronchiolo-Alveolar/pathology/radiography/surgery
Adult
Female
Humans
Lung Neoplasms/pathology/*radiography/surgery
Male
Middle Aged
Multiple Pulmonary Nodules/pathology/*radiography/surgery
Prognosis
Solitary Pulmonary Nodule/pathology/*radiography/surgery
*Tomography, X-Ray Computed
Young Adult
Figure
Reference
-
1. Henschke CI, Yankelevitz DF, Mirtcheva R, McGuinness G, McCauley D, Miettinen OS. CT screening for lung cancer: frequency and significance of part-solid and nonsolid nodules. AJR Am J Roentgenol. 2002. 178:1053–1057.2. Kim HY, Shim YM, Lee KS, Han J, Yi CA, Kim YK. Persistent pulmonary nodular ground-glass opacity at thin-section CT: histopathologic comparisons. Radiology. 2007. 245:267–275.3. Lee HJ, Goo JM, Lee CH, Yoo CG, Kim YT, Im JG. Nodular ground-glass opacities on thin-section CT: size change during follow-up and pathological results. Korean J Radiol. 2007. 8:22–31.4. Asamura H, Suzuki K, Watanabe S, Matsuno Y, Maeshima A, Tsuchiya R. A clinicopathological study of resected subcentimeter lung cancers: a favorable prognosis for ground glass opacity lesions. Ann Thorac Surg. 2003. 76:1016–1022.5. Ohtsuka T, Watanabe K, Kaji M, Naruke T, Suemasu K. A clinicopathological study of resected pulmonary nodules with focal pure ground-glass opacity. Eur J Cardiothorac Surg. 2006. 30:160–163.6. Watanabe S, Watanabe T, Arai K, Kasai T, Haratake J, Urayama H. Results of wedge resection for focal bronchioloalveolar carcinoma showing pure ground-glass attenuation on computed tomography. Ann Thorac Surg. 2002. 73:1071–1075.7. Yoshida J, Nagai K, Yokose T, Nishimura M, Kakinuma R, Ohmatsu H, et al. Limited resection trial for pulmonary ground-glass opacity nodules: fifty-case experience. J Thorac Cardiovasc Surg. 2005. 129:991–996.8. Mun M, Kohno T. Efficacy of thoracoscopic resection for multifocal bronchioloalveolar carcinoma showing pure ground-glass opacities of 20 mm or less in diameter. J Thorac Cardiovasc Surg. 2007. 134:877–882.9. Gandara DR, West H, Chansky K, Davies AM, Lau DHM, Crowley J, et al. Bronchioloalveolar carcinoma: a model for investigating the biology of epidermal growth factor receptor inhibition. Clin Cancer Res. 2004. 10:S4205–S4209.10. Beasley MB, Brambilla E, Travis WD. The 2004 World Health Organization classification of lung tumors. Semin Roentgenol. 2005. 40:90–97.11. Penman D, Downie I, Roberts F. Positive immunostaining for thyroid transcription factor-1 in primary and metastatic colonic adenocarcinoma: a note of caution. J Clin Pathol. 2006. 59:663–664.12. Chhieng DC, Cangiarella JF, Zakowski MF, Goswami S, Cohen JM, Yee HT. Use of thyroid transcription factor 1, PE-10, and cytokeratins 7 and 20 in discriminating between primary lung carcinomas and metastatic lesions in fine-needle aspiration biopsy specimens. Cancer. 2001. 93:330–336.13. Kodama K, Higashiyama M, Yokouchi H, Takami K, Kuriyama K, Kusunoki Y, et al. Natural history of pure ground-glass opacity after long-term follow-up of more than 2 years. Ann Thorac Surg. 2002. 73:386–392.14. Lindell RM, Hartman TE, Swensen SJ, Jett JR, Midthun DE, Tazelaar HD, et al. Five-year lung cancer screening experience: CT appearance, growth rate, location, and histologic features of 61 lung cancers. Radiology. 2007. 242:555–562.15. Hasegawa M, Sone S, Takashima S, Li F, Yang ZG, Maruyama Y, et al. Growth rate of small lung cancers detected on mass CT screening. Br J Radiol. 2000. 73:1252–1259.16. Suzuki K, Kusumoto M, Watanabe S, Tsuchiva R, Asamura H. Radiologic classification of small adenocarcinoma of the lung: radiologic-pathologic correlation and its prognostic impact. Ann Thorac Surg. 2006. 81:413–419.17. Kakinuma R, Ohmatsu H, Kaneko M, Kusumoto M, Yoshida J, Nagai K, et al. Progression of focal pure ground-glass opacity detected by low-dose helical computed tomography screening for lung cancer. J Comput Assist Tomogr. 2004. 28:17–23.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Clinical Approach to Nodular Ground Glass Opacity in the Lung
- Primary Pulmonary Malignant Melanoma Presenting as Bilateral Multiple Subsolid Nodules: A Case Report
- Cryoablation of a Small Pulmonary Nodule with Pure Ground-Glass Opacity: A Case Report
- Radiographic Findings of Miliary Tuberculosis: Difference in Patients with and those without Associated Acute Respiratory Failure
- Guidelines for the Investigation and Management of Ground Glass Nodules