Korean J Gastroenterol.
2011 Sep;58(3):144-148. 10.4166/kjg.2011.58.3.144.
A Case of a Neuroendocrine Carcinoma in the Minor Papilla
- Affiliations
-
- 1Department of Internal Medicine, Pusan National University School of Medicine, Busan, Korea. doc0224@pusan.ac.kr
- 2Department of Pathology, Pusan National University School of Medicine, Busan, Korea.
- 3Department of Surgery, Pusan National University School of Medicine, Busan, Korea.
- KMID: 1018402
- DOI: http://doi.org/10.4166/kjg.2011.58.3.144
Abstract
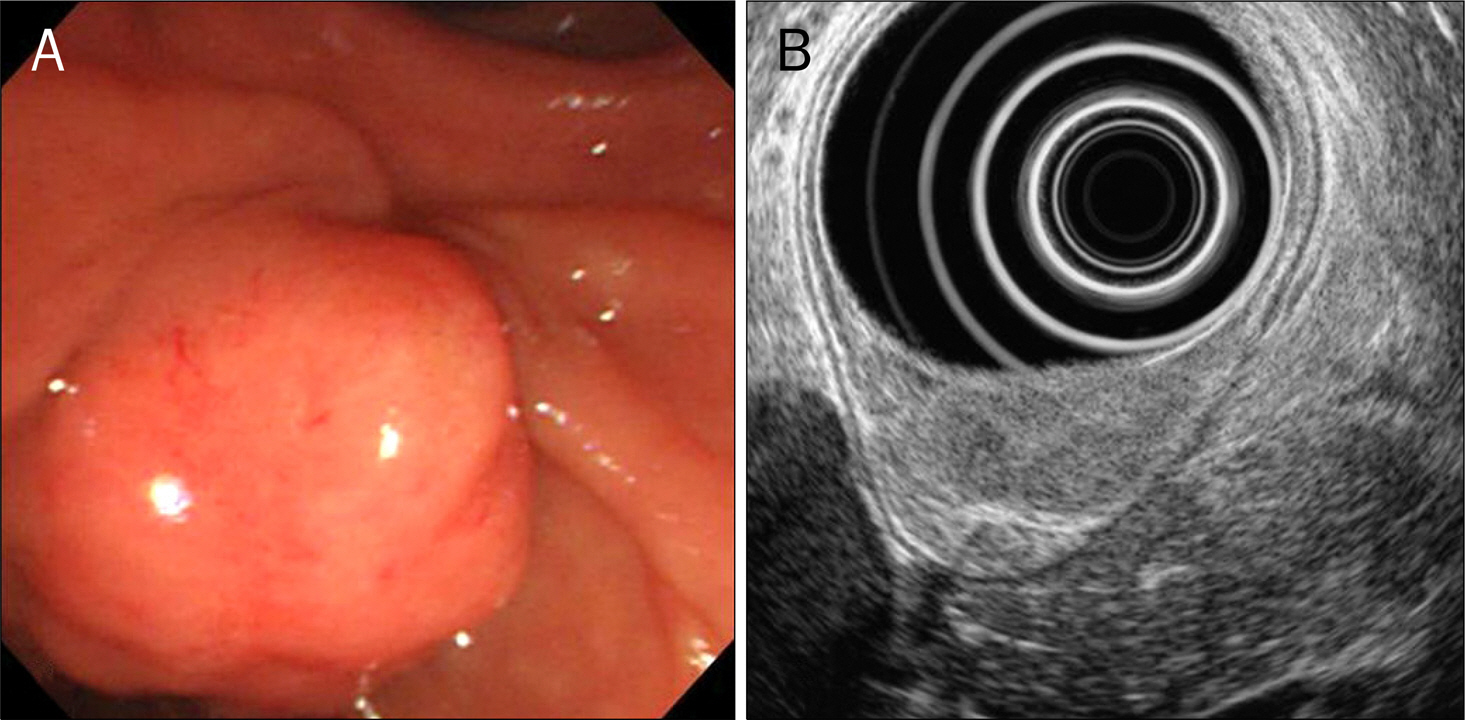
- Neuroendocrine tumors are usually found in the ileum, appendix, rectum, colon and stomach. Ampullary neuroendocrine tumor is extremely rare and only a few cases of neuroendocrine carcinoma of the minor papilla have been reported. The preoperative diagnosis is very challenging because either asymptomatic or manifests as nonspecific abdominal pain. The tumor is relatively small and located at the deep mucosa and submucosa. Endoscopy with deep biopsy, endoscopic retrograde cholangiopancreatography and endoscopic ultrasonography are good diagnostic tools. The best therapeutic choice is surgery. We report an unusual case of a 55-year-old woman who underwent endoscopy as part of a regular health checkup and was diagnosed a neuroendocrine carcinoma in the minor papilla, which was successfully resected by pancreaticoduodenectomy.
MeSH Terms
Figure
Reference
-
References
1. Capella C, Heitz PU, Höfler H, Solcia E, Klöppel G. Revised classification of neuroendocrine tumors of the lung, pancreas and gut. Digestion. 1994; 55(Suppl 3):11–23.
Article2. Donadon M, Torzilli G, Palmisano A, et al. Liver resection for primary hepatic neuroendocrine tumours: report of three cases and review of the literature. Eur J Surg Oncol. 2006; 32:325–328.
Article3. Sun JM, Jung HC. Gastrointestinal carcinoid tumor. Korean J Gastroenterol. 2004; 44:59–65.4. Lee DH, Chin HM, Kim JG, Lee YB, Park WB, Chun CS. Clinical analysis of carcinoid tumors. J Korean Surg Soc. 1997; 53:315–323.5. Soga J. Endocrinocarcinomas (carcinoids and their variants) of the duodenum. An evaluation of 927 cases. J Exp Clin Cancer Res. 2003; 22:349–363.6. Waisberg J, de Matos LL, Waisberg DR, dos Santos HV, Fernezlian SM, Capelozzi VL. Carcinoid of the minor duodenal papilla associated with pancreas divisum: Case report and review of the literature. Clinics (Sao Paulo). 2006; 61:365–368.
Article7. Choi YH, Park DH, Kim SJ, et al. Two cases of endoscopic resection of submucosal tumor of the minor papilla. Korean J Gastrointest Endosc. 2007; 34:164–169.8. Noda Y, Watanabe H, Iwafuchi M, et al. Carcinoids and endocrine cell micronests of the minor and major duodenal papillae. Their incidence and characteristics. Cancer. 1992; 70:1825–1833.
Article9. Makhlouf HR, Burke AP, Sobin LH. Carcinoid tumors of the ampulla of Vater: a comparison with duodenal carcinoid tumors. Cancer. 1999; 85:1241–1249.10. Walton GF, Gibbs ER, Spencer GO, Laws HL. Carcinoid tumors of the ampulla of Vater. Am Surg. 1997; 63:302–304.11. Bisceglia M, Giordano M, Bosman C. Argyrophil-negative G-cell duodenal carcinoid. Am J Gastroenterol. 1992; 87:534–537.12. Burke AP, Sobin LH, Federspiel BH, Shekitka KM, Helwig EB. Carcinoid tumors of the duodenum. A clinicopathologic study of 99 cases. Arch Pathol Lab Med. 1990; 114:700–704.13. Hatzitheoklitos E, Büchler MW, Friess H, et al. Carcinoid of the ampulla of Vater: clinical characteristics and morphologic features. Cancer. 1994; 73:1580–1588.
Article14. Malone MJ, Silverman ML, Braasch JW, Jin GL, Dayal Y. Early somatostatinoma of the papilla of the duct of Santorini. Arch Surg. 1985; 120:1381–1383.
Article15. Wang HY, Chen MJ, Yang TL, Chang MC, Chan YJ. Carcinoid tumor of the duodenum and accessory papilla associated with poly-cythemia vera. World J Gastroenterol. 2005; 11:3794–3796.
Article16. Burke AP, Sobin LH, Federspiel BH, Shekitka KM, Helwig EB. Carcinoids of the duodenum: a histologic and immunohistochemical study of 65 tumors. Am J Surg Pathol. 1989; 13:828–837.17. Lucena JF, Alvarez OA, Gross GW. Endoscopic resection of heterotopic pancreas of the minor duodenal papilla: case report and review of the literature. Gastrointest Endosc. 1997; 46:69–72.
Article18. Nakamura T, Ozawa T, Kitagawa M, et al. Endoscopic resection of gangliocytic paraganglioma of the minor duodenal papilla: case report and review. Gastrointest Endosc. 2002; 55:270–273.
Article19. Modlin IM, Oberg K, Chung DC, et al. Gastroenteropancreatic neuroendocrine tumours. Lancet Oncol. 2008; 9:61–72.
Article20. Cook MR, Pinchot SN, Jaskula-Sztul R, Luo J, Kunnimalaiyaan M, Chen H. Identification of a novel Raf-1 pathway activator that inhibits gastrointestinal carcinoid cell growth. Mol Cancer Ther. 2010; 9:429–437.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Two Cases of Endoscopic Papillectomy for Neuroendocrine Tumor Arising from Minor Papilla
- Endoscopic Papillectomy for Synchronous Major and Minor Duodenal Papilla Neuroendocrine Tumors
- Endoscopic Approach via the Minor Papilla for the Treatment of Pancreatic Stones
- Neuroendocrine Tumor with Metachronous Gastrointestinal Stromal Tumor in a Patient: A Case Report
- Two Cases of Endoscopic Resection of Submucosal Tumor of the Minor Papilla