Blood Res.
2023 Dec;58(4):208-220. 10.5045/br.2023.2023208.
A retrospective analysis of ibrutinib outcomes in relapsed or refractory mantle cell lymphoma
- Affiliations
-
- 1Division of Hematology-Oncology, Department of Internal Medicine, Chungbuk National University Hospital, Cheongju, Korea
- 2Division of Hematology-Oncology ,Departments of Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 3Departments of Pathology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 4Health Sciences and Technology, Samsung Advanced Institute for Health Sciences and Technology, Sungkyunkwan University, Seoul, Korea
- KMID: 2550199
- DOI: http://doi.org/10.5045/br.2023.2023208
Abstract
- Background
While treatment strategies for mantle cell lymphoma (MCL) have evolved, patients often experience disease progression and require additional treatment therapies. Ibrutinib presents a promising option for relapsed or refractory MCL (RR-MCL). This study investigated real-world treatment outcomes of ibrutinib in patients with RR-MCL.
Methods
A single-center retrospective analysis investigated clinical characteristics and survival outcomes of patients with RR-MCL, treated with ibrutinib.
Results
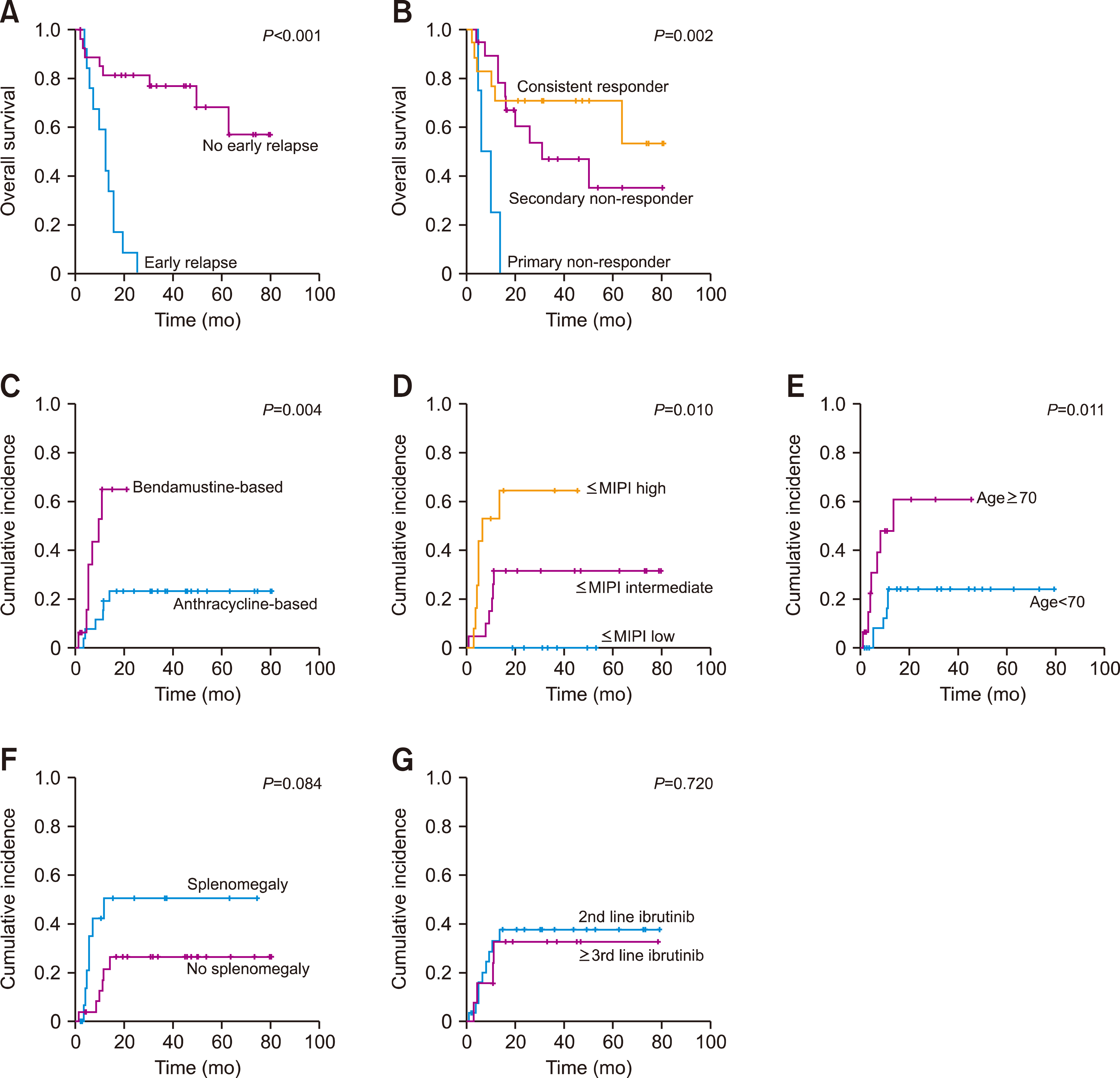
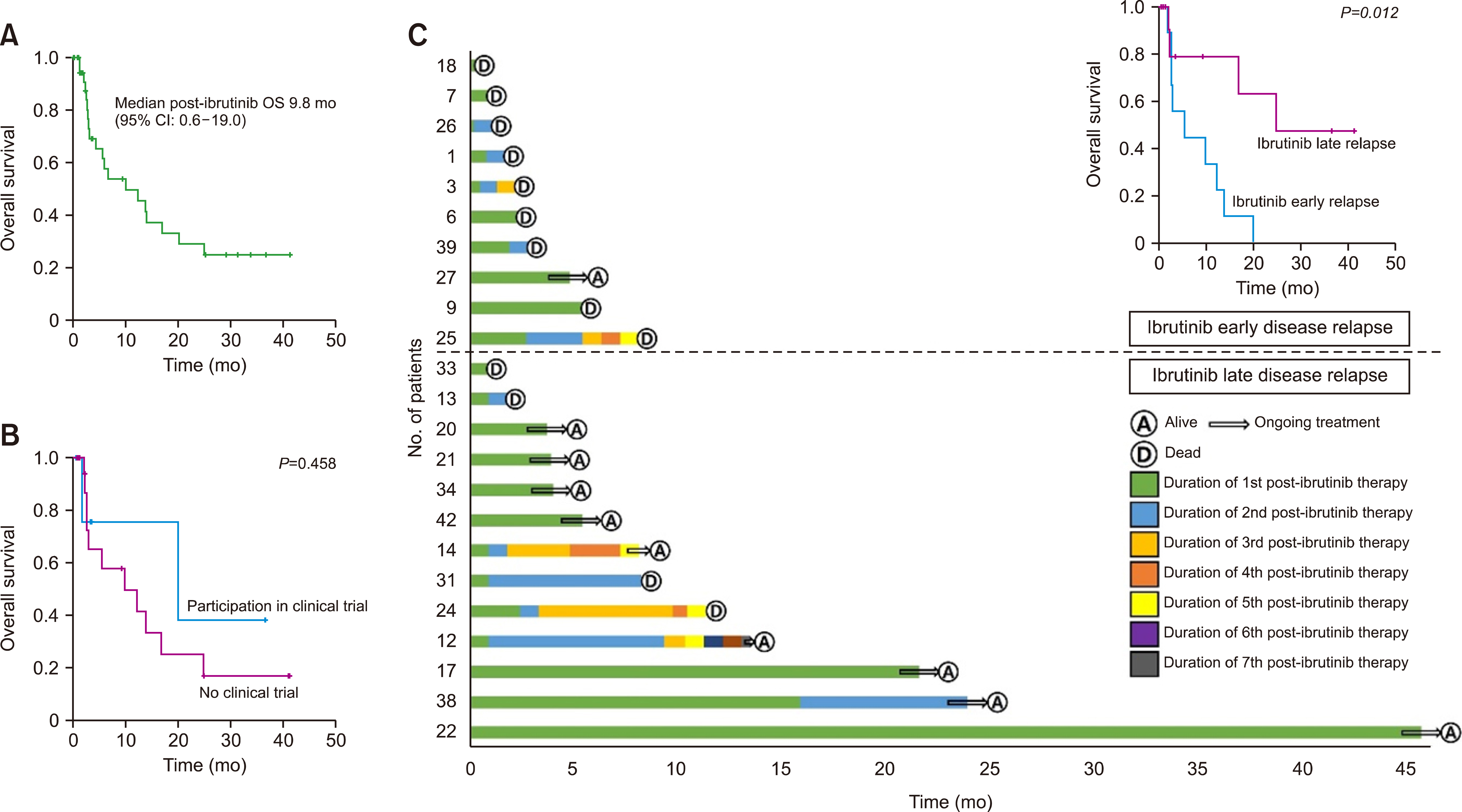
Forty-two patients were included, with 16 received rituximab and bendamustine, and 26 receiving anthracycline-based regimens as front-line treatment. During a median follow-up of 46.0 months, the response rate to ibrutinib was 69%, with 12 CRs and 8 partial responses. Disease progression (54.8%) and adverse events (11.9%) were the primary reasons for discontinuation. Median progression-free survival (PFS) and overall survival (OS) were approximately 16.4 and 50.1 months, respectively. Patients older than 70 years (P =0.044 and P =0.006), those with splenomegaly (P =0.022 and P=0.006), and those with a high-risk simplified Mantle Cell Lymphoma International Prognostic Index (sMIPI) (P<0.001 and P<0.001) exhibited siginificantly inferior PFS and OS. Notably, patients with a high-risk sMIPI relapsed earlier. Post-ibrutinib treatment yilded an OS of 12.2 months, while clinical trial participants demonstrated superior survival compared to those receiving chemotherapy alone.
Conclusion
This study underscores the importance of considering patient characteristics before administering ibrutinib as salvage therapy. Early relapse was associated with poor outcomes, highlighting the need for novel therapeutic strategies.
Keyword
Figure
Reference
-
1. Armitage JO, Longo DL. 2022; Mantle-cell lymphoma. N Engl J Med. 386:2495–506. DOI: 10.1056/NEJMra2202672. PMID: 35767440.2. Lee H, Park HJ, Park EH, et al. 2018; Nationwide statistical analysis of lymphoid malignancies in Korea. Cancer Res Treat. 50:222–38. DOI: 10.4143/crt.2017.093. PMID: 28361523. PMCID: PMC5784621.3. Merolle MI, Ahmed M, Nomie K, Wang ML. 2018; The B cell receptor signaling pathway in mantle cell lymphoma. Oncotarget. 9:25332–41. DOI: 10.18632/oncotarget.25011. PMID: 29861875. PMCID: PMC5982769.4. Gu D, Tang H, Wu J, Li J, Miao Y. 2021; Targeting Bruton tyrosine kinase using noncovalent inhibitors in B cell malignancies. J Hematol Oncol. 14:40. DOI: 10.1186/s13045-021-01049-7. PMID: 33676527. PMCID: PMC7937220. PMID: 557fae3ccc224792b23426e77330dc47.5. Wang ML, Rule S, Martin P, et al. 2013; Targeting BTK with ibrutinib in relapsed or refractory mantle-cell lymphoma. N Engl J Med. 369:507–16. DOI: 10.1056/NEJMoa1306220. PMID: 23782157. PMCID: PMC4513941.6. Wang ML, Blum KA, Martin P, et al. 2015; Long-term follow-up of MCL patients treated with single-agent ibrutinib: updated safety and efficacy results. Blood. 126:739–45. DOI: 10.1182/blood-2015-03-635326. PMID: 26059948. PMCID: PMC4528064.7. Dreyling M, Jurczak W, Jerkeman M, et al. 2016; Ibrutinib versus temsirolimus in patients with relapsed or refractory mantle-cell lymphoma: an international, randomised, open-label, phase 3 study. Lancet. 387:770–8. DOI: 10.1016/S0140-6736(15)00667-4. PMID: 26673811.8. Epperla N, Hamadani M, Cashen AF, et al. 2017; Predictive factors and outcomes for ibrutinib therapy in relapsed/refractory mantle cell lymphoma-a "real world" study. Hematol Oncol. 35:528–35. DOI: 10.1002/hon.2380. PMID: 28066928.9. Maruyama D, Nagai H, Fukuhara N, et al. 2016; Efficacy and safety of ibrutinib in Japanese patients with relapsed or refractory mantle cell lymphoma. Cancer Sci. 107:1785–90. DOI: 10.1111/cas.13076. PMID: 27616553. PMCID: PMC5198949.10. Jeon YW, Yoon S, Min GJ, et al. 2019; Clinical outcomes for ibrutinib in relapsed or refractory mantle cell lymphoma in real-world experience. Cancer Med. 8:6860–70. DOI: 10.1002/cam4.2565. PMID: 31560165. PMCID: PMC6853811. PMID: 36694bde129a4c0885fe2877f438723f.11. Tucker D, Morley N, MacLean P, et al. 2021; The 5-year follow-up of a real-world observational study of patients in the United Kingdom and Ireland receiving ibrutinib for relapsed/refractory mantle cell lymphoma. Br J Haematol. 192:1035–8. DOI: 10.1111/bjh.16739. PMID: 32445482.12. Yi JH, Kim SJ, Yoon DH, et al. 2021; Real-world outcomes of ibrutinib therapy in Korean patients with relapsed or refractory mantle cell lymphoma: a multicenter, retrospective analysis. Cancer Commun (Lond). 41:275–8. DOI: 10.1002/cac2.12150. PMID: 33626235. PMCID: PMC7968880. PMID: 5d08eb39eacb428a89867494569557f4.13. McCulloch R, Lewis D, Crosbie N, et al. 2021; Ibrutinib for mantle cell lymphoma at first relapse: a United Kingdom real-world analysis of outcomes in 211 patients. Br J Haematol. 193:290–8. DOI: 10.1111/bjh.17363. PMID: 33620106.14. Obr A, Benesova K, Janikova A, et al. 2023; Ibrutinib in mantle cell lymphoma: a real-world retrospective multi-center analysis of 77 patients treated in the Czech Republic. Ann Hematol. 102:107–15. DOI: 10.1007/s00277-022-05023-2. PMID: 36369497. PMCID: PMC9807478.15. Rule S, Dreyling M, Goy A, et al. 2019; Ibrutinib for the treatment of relapsed/refractory mantle cell lymphoma: extended 3.5-year follow up from a pooled analysis. Haematologica. 104:e211–4. DOI: 10.3324/haematol.2018.205229. PMID: 30442728. PMCID: PMC6518912.16. Wang M, Munoz J, Goy A, et al. 2020; KTE-X19 CAR T-cell therapy in relapsed or refractory mantle-cell lymphoma. N Engl J Med. 382:1331–42. DOI: 10.1056/NEJMoa1914347. PMID: 32242358. PMCID: PMC7731441.17. Wang M, Munoz J, Goy A, et al. 2023; Three-year follow-up of KTE-X19 in patients with relapsed/refractory mantle cell lymphoma, including high-risk subgroups, in the ZUMA-2 study. J Clin Oncol. 41:555–67. DOI: 10.1200/JCO.21.02370. PMID: 35658525. PMCID: PMC9870225.18. Swerdlow SH, Campo E, Pileri SA, et al. 2016; The 2016 revision of the World Health Organization classification of lymphoid neoplasms. Blood. 127:2375–90. DOI: 10.1182/blood-2016-01-643569. PMID: 26980727. PMCID: PMC4874220.19. Cheson BD, Fisher RI, Barrington SF, et al. 2014; Recommendations for initial evaluation, staging, and response assessment of Hodgkin and non-Hodgkin lymphoma: the Lugano classification. J Clin Oncol. 32:3059–68. DOI: 10.1200/JCO.2013.54.8800. PMID: 25113753. PMCID: PMC4979083.20. Dreyling M, Goy A, Hess G, et al. 2022; Long-term outcomes with ibrutinib treatment for patients with relapsed/refractory mantle cell lymphoma: a pooled analysis of 3 clinical trials with nearly 10 years of follow-up. Hemasphere. 6:e712. DOI: 10.1097/HS9.0000000000000712. PMID: 35441128. PMCID: PMC9010121. PMID: 89d6d5174cfe41b2b75b096c51736769.21. Bond DA, Switchenko JM, Maddocks KJ, et al. 2019; Outcomes following early relapse in patients with mantle cell lymphoma. Blood (ASH Annual Meeting Abstracts). 134(Suppl 1):753. DOI: 10.1182/blood-2019-128415.22. Lew TE, Minson A, Dickinson M, et al. 2023; Treatment approaches for patients with TP53-mutated mantle cell lymphoma. Lancet Haematol. 10:e142–54. DOI: 10.1016/S2352-3026(22)00355-6. PMID: 36725119.23. Eskelund CW, Dahl C, Hansen JW, et al. 2017; TP53 mutations identify younger mantle cell lymphoma patients who do not benefit from intensive chemoimmunotherapy. Blood. 130:1903–10. DOI: 10.1182/blood-2017-04-779736. PMID: 28819011.24. Wang ML, Jurczak W, Zinzani PL, et al. 2023; Pirtobrutinib in covalent bruton tyrosine kinase inhibitor pretreated mantle-cell lymphoma. J Clin Oncol. 41:3988–97. DOI: 10.1200/JCO.23.00562. PMID: 37192437. PMCID: PMC10461952.25. Palomba ML, Gordon LI, Siddiqi T, et al. 2020; Safety and preliminary efficacy in patients with relapsed/refractory mantle cell lymphoma receiving lisocabtagene maraleucel in transcend NHL 001. Blood (ASH Annual Meeting Abstracts). 136(Suppl 1):10–1. DOI: 10.1182/blood-2020-136158.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Mantle cell lymphoma relapsed after autologous stem cell transplantation: a single-center experience
- Safety and efficacy analysis of ibrutinib in 32 patients with CLL and various B-cell lymphomas: real-world data from a single-center study in Turkey
- Patient profiles and outcomes of lymphoma patients who underwent autologous stem cell transplant in National Kidney and Transplant Institute: a single-center analysis
- Mantle cell lymphoma: a model for risk-adapted treatment approach
- A Case of Primary Mantle Cell Lymphoma on the Conjunctiva