J Korean Soc Magn Reson Med.
2013 Sep;17(3):181-191. 10.13104/jksmrm.2013.17.3.181.
Serial MR Imaging of Magnetically Labeled Humen Umbilical Vein Endothelial Cells in Acute Renal Failure Rat Model
- Affiliations
-
- 1Department of Radiology, College of Medicine, Inje University, Busan Paik Hospital, Busan, Korea.
- 2Department of Diagnostic Radiology, Chonbuk National University Hospital & Medical School, Jeonbuk, Korea. sangyleekr@gmail.com
- 3Department of Internal Medicine Chonbuk National University Hospital & Medical School, Jeonbuk, Korea.
- KMID: 2206916
- DOI: http://doi.org/10.13104/jksmrm.2013.17.3.181
Abstract
- PURPOSE
To evaluate the usefulness of in vivo magnetic resonance (MR) imaging for tracking intravenously injected superparamagnetic iron oxide (SPIO)-labeled human umbilical vein endothelial cells (HUVECs) in an acute renal failure (ARF) rat model.
MATERIALS AND METHODS
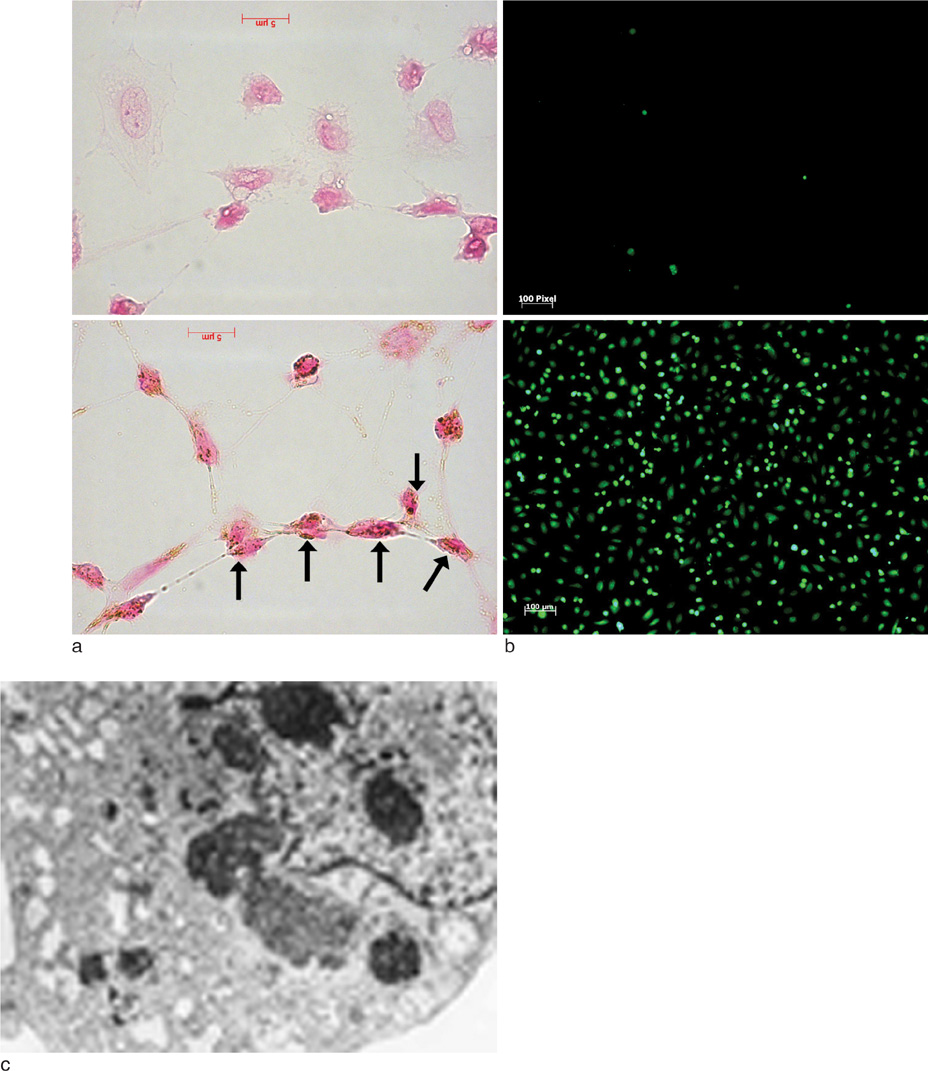
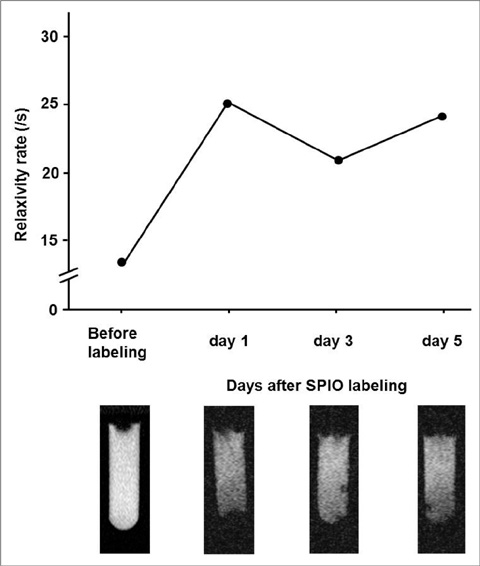
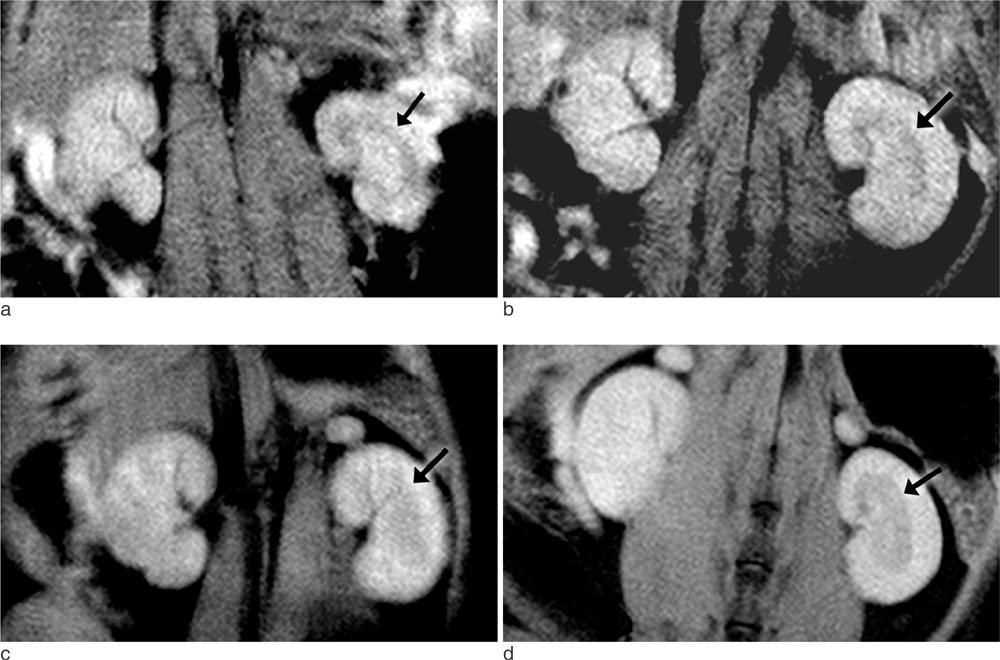
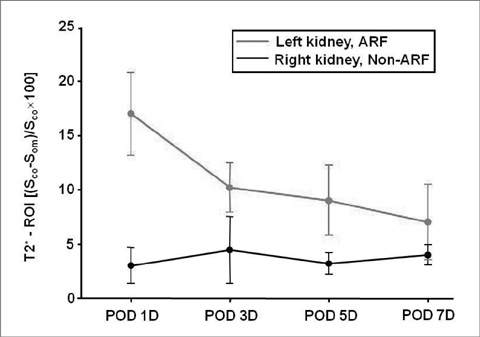
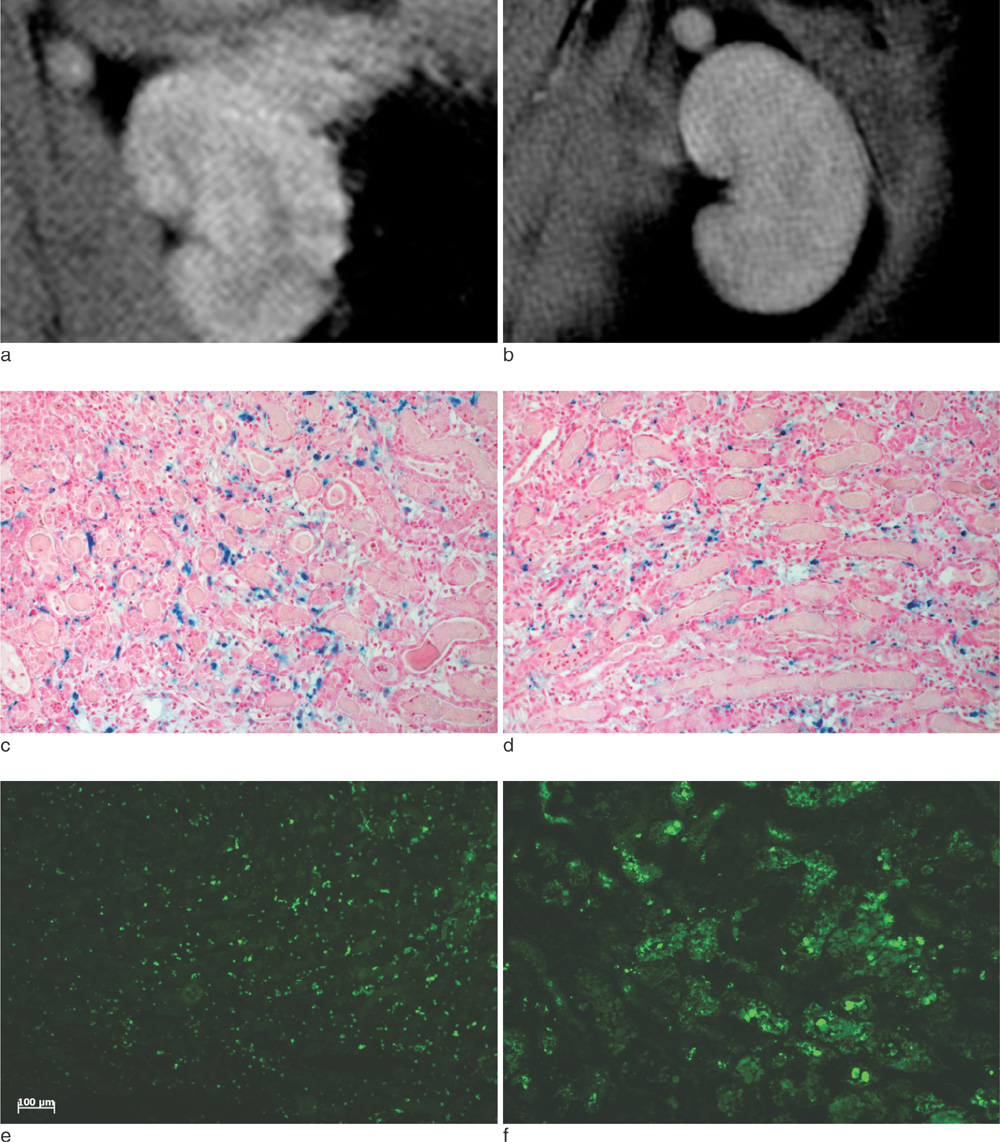
HUVECs were labeled with SPIO and poly-L-lysine (PLL) complex. Relaxation rates at 1.5-T MR, cell viability, and labeling stability were assessed. HUVECs were injected into the tail vein of ARF rats (labeled cells in 10 rats, unlabeled cells in 2 rats). Follow-up serial T2*-weighted gradient-echo MR imaging was performed at 1, 3, 5 and 7 days after injection, and the MR findings were compared with histologic findings.
RESULTS
There was an average of 98.4+/-2.4% Prussian blue stain-positive cells after labeling with SPIO-PLL complex. Relaxation rates (R2*) of all cultured HUVECs at day 3 and 5 were not markedly decreased compared with that at day 1. The stability of SPIO in HUVECs was maintained during the proliferation of HUVECs in culture media. In the presence of left unilateral renal artery ischemia, T2*-weighted MR imaging performed 1 day after the intravenous injection of labeled HUVECs revealed a significant signal intensity (SI) loss exclusively in the left renal outer medulla regions, but not in the right kidney. The MR imaging findings at days 3, 5 and 7 after intravenous injection of HUVECs showed a SI loss in the outer medulla regions of the ischemically injured kidney, but the SI progressively recovered with time and the right kidney did not have a significant change in SI in the same period. Upon histologic analysis, the SI loss on MR images was correspondent to the presence of Prussian blue stained cells, primarily in the renal outer medulla.
CONCLUSION
MR imaging appears to be useful for in vivo monitoring of intravenously injected SPIO-labeled HUVECs in an ischemically injured rat kidney.
Keyword
MeSH Terms
-
Acute Kidney Injury
Animals
Cell Survival
Cell Tracking
Culture Media
Endothelial Cells
Ferric Compounds
Ferrocyanides
Follow-Up Studies
Human Umbilical Vein Endothelial Cells
Injections, Intravenous
Iron
Ischemia
Kidney
Magnetic Resonance Spectroscopy
Magnets
Rats
Relaxation
Renal Artery
Track and Field
Umbilical Veins
Veins
Culture Media
Ferric Compounds
Ferrocyanides
Iron
Figure
Reference
-
1. Thadhani R, Pascual M, Bonventre JV. Acute renal failure. N Engl J Med. 1996; 334:1448–1460.2. Rookmaaker MB, Verhaar MC, van Zonneveld AJ, Rabelink TJ. Progenitor cells in the kidney: biology and therapeutic perspectives. Kidney Int. 2004; 66:518–522.3. Brodsky SV, Yamamoto T, Tada T, et al. Endothelial dysfunction in ischemic acute renal failure: rescue by transplanted endothelial cells. Am J Physiol Renal Physiol. 2002; 282:F1140–F1149.4. Sun R, Dittrich J, Le-Huu M, et al. Physical and biological characterization of superparamagnetic iron oxide- and ultrasmall superparamagnetic iron oxide-labeled cells: a comparison. Invest Radiol. 2005; 40:504–513.5. Frank JA, Anderson SA, Kalsih H, et al. Methods for magnetically labeling stem and other cells for detection by in vivo magnetic resonance imaging. Cytotherapy. 2004; 6:621–625.6. Zhang Z, van den Bos EJ, Wielopolsk PA, et al. In vitro imaging of single living human umbilical vein endothelial cells with a clinical 3.0-T MRI scanner. Magma. 2005; 18:175–185.7. Bulte JW, Zhang S, van Gelderen P, et al. Neurotransplantation of magnetically labeled oligodendrocyte progenitors: magnetic resonance tracking of cell migration and myelination. Proc Natl Acad Sci USA. 1999; 96:15256–15261.8. Bulte JW, Arbab AS, Douglas T, Frank JA. Preparation of magnetically labeled cells for cell tracking by magnetic resonance imaging. Methods Enzymol. 2004; 386:275–299.9. Kraitchman DL, Heldman AW, Atalar E, et al. In vivo magnetic resonance imaging of mesenchymal stem cells in myocardial infarction. Circulation. 2003; 107:2290–2293.10. Magnitsky S, Watson DJ, Walton RM, et al. In vivo and ex vivo MRI detection of localized and disseminated neural stem cell grafts in the mouse brain. Neuroimage. 2005; 26:744–754.11. Hauger O, Frost EE, van Heeswijk R, et al. MR evaluation of the glomerular homing of magnetically labeled mesenchymal stem cells in a rat model of nephropathy. Radiology. 2006; 238:200–210.12. Arbab AS, Yocum GT, Wilson LB, et al. Comparison of transfection agents in forming complexes with ferumoxides, cell labeling efficiency, and cellular viability. Mol Imaging. 2004; 3:24–32.13. Himes N, Min JY, Lee R, et al. In vivo MRI of embryonic stem cells in a mouse model of myocardial infarction. Magn Reson Med. 2004; 52:1214–1219.14. Ho C, Hitchens TK. A non-invasive approach to detecting organ rejection by MRI: monitoring the accumulation of immune cells at the transplanted organ. Curr Pharm Biotechnol. 2004; 5:551–566.15. Kircher MF, Allport JR, Graves EE, et al. In vivo high resolution three-dimensional imaging of antigen-specific cytotoxic T-lymphocyte trafficking to tumors. Cancer Res. 2003; 63:6838–6846.16. Sung MJ, Kim W, Ahn SY, et al. Protective effect of alpha-lipoic acid in lipopolysaccharide-induced endothelial fractalkine expression. Circ Res. 2005; 97:880–890.17. Arbab AS, Bashaw LA, Miller BR, et al. Characterization of biophysical and metabolic properties of cells labeled with superparamagnetic iron oxide nanoparticles and transfection agent for cellular MR imaging. Radiology. 2003; 229:838–846.18. Bos C, Delmas Y, Desmoulière A, et al. In vivo MR imaging of intravascularly injected magnetically labeled mesenchymal stem cells in rat kidney and liver. Radiology. 2004; 233:781–789.19. Jung CW, Jacobs P. Physical and chemical properties of superparamagnetic iron oxide MR contrast agents: ferumoxides, ferumoxtran, ferumoxsil. Magn Reson Imaging. 1995; 13:661–674.20. Artemov D. Molecular magnetic resonance imaging with targeted contrast agents. J Cell Biochem. 2003; 90:518–524.21. Thorek DL, Chen AK, Czupryna J, Tsourkas A. Superparamagnetic iron oxide nanoparticle probes for molecular imaging. Ann Biomed Eng. 2006; 34:23–38.22. Basile DP, Donohoe D, Roethe K, Osborn JL. Renal ischemic injury results in permanent damage to peritubular capillaries and influences long-term function. Am J Physiol Renal Physiol. 2001; 281:F887–F899.23. Sutton TA, Fisher CJ, Molitoris BA. Microvascular endothelial injury and dysfunction during ischemic acute renal failure. Kidney Int. 2002; 62:1539–1549.24. Takahashi T, Kalka C, Masuda H, et al. Ischemia- and cytokine-induced mobilization of bone marrow-derived endothelial progenitor cells for neovascularization. Nat Med. 1999; 5:434–438.25. Crosby JR, Kaminski WE, Schatteman G, et al. Endothelial cells of hematopoietic origin make a significant contribution to adult blood vessel formation. Circ Res. 2000; 87:728–730.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effects of Endothelial Progenitor Cells Used for Autograft Transplantation in Acute Myocardial Infarction Pig Model
- Zerumbone, Sesquiterpene Photochemical from Ginger, Inhibits Angiogenesis
- In Vivo MR Imaging of Magnetically Labeled Mesenchymal Stem Cells in a Rat Model of Renal Ischemia
- In Vitro Culture of Endothelial Cell and Smooth Muscle Cell for Studying Vascular Diseases
- Hantaan Virus Reduces the von Willebrand Factor in Human Umbilical Vein Endothelial Cells