Clin Orthop Surg.
2011 Mar;3(1):62-68. 10.4055/cios.2011.3.1.62.
Complication Rate and Pitfalls of Temporary Bridging External Fixator in Periarticular Communited Fractures
- Affiliations
-
- 1Department of Orthopaedic Surgery, Korea University School of Medicine, Seoul, Korea.
- 2Department of Orthopaedic Surgery, Yonsei University College of Medicine, Seoul, Korea. osjinho@naver.com
- 3Department of Orthopaedic Surgery, Konkuk University School of Medicine, Seoul, Korea.
- KMID: 999462
- DOI: http://doi.org/10.4055/cios.2011.3.1.62
Abstract
- BACKGROUND
A second staged operation using temporary bridging external fixation (TBEF) has been widely used in patients with periarticular complex fracture, yet few papers have been published on the related complications. The purpose of this study was to report the complication rate and pitfalls directly related to TBEF through a retrospective study and to suggest some solutions.
METHODS
Fifty-nine cases that were treated by using TBEF were studied among 195 periarticular complex fractures. We retrospectively collected the clinical and radiological data and then the study data was evaluated for 1) cases with unsatisfactory restoration of length, 2) cases with deep infection caused by half pins invading the zone of definitive fixation, and 3) neurovascular injuries related to half pins.
RESULTS
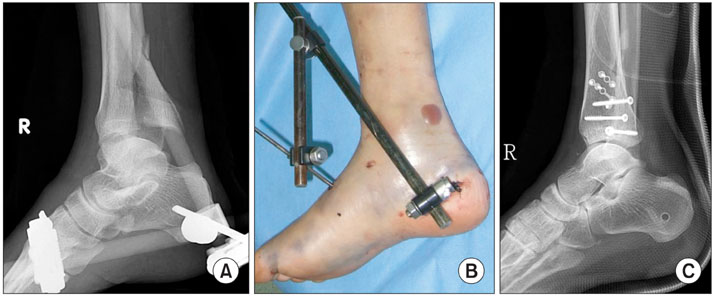
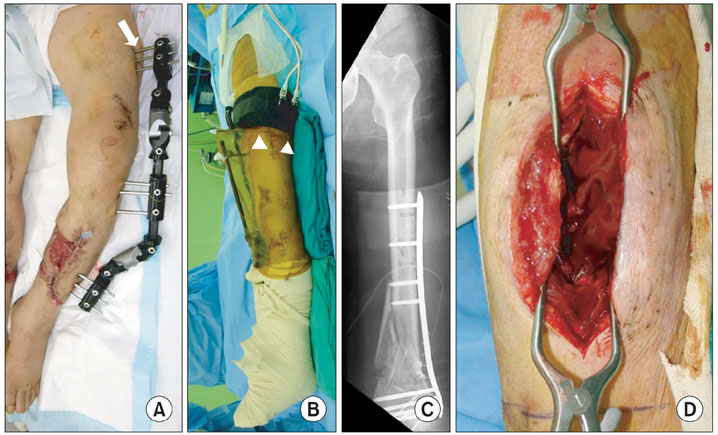
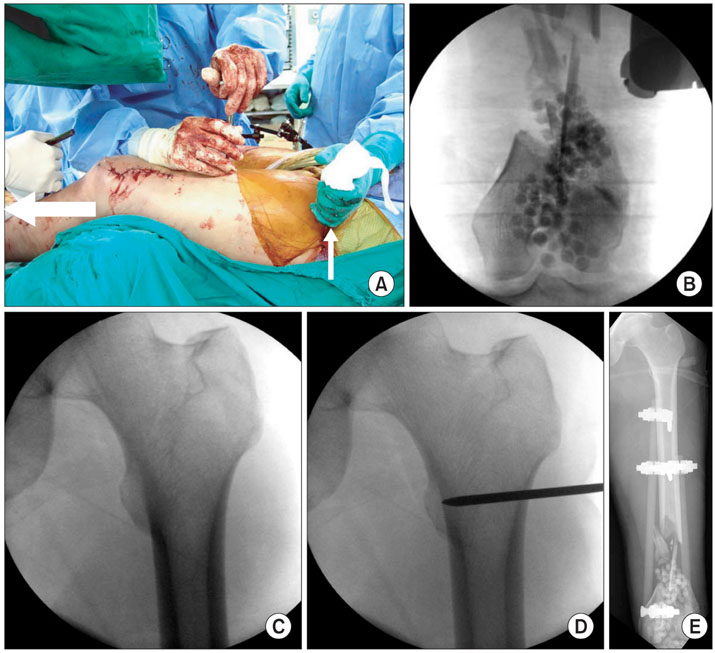
Complications were observed in 7/59 cases (11%). Problems related to the achievement of length were observed in one case of distal tibia fracture and 2 cases of distal femur fracture. Half pin related infection was observed in 2 cases of distal femur fracture. Neurovascular injury (medial calcaneal nerve injury in a distal tibia fracture) was observed in 2 cases. Among 7 complications, four were related to using TBEF in distal femur fracture. This is because the abundant leg muscles have strong deforming force and infection might be increased due to frequent irritation by the half pins.
CONCLUSIONS
TBEF is a simple procedure with several advantages. However, complications might be observed if certain principles are not followed. It is thought that many complications due to TBEF can be reduced if the half pins are not inserted in the zone of injury, restoration of length is fully achieved and the neurovascular characteristics are carefully considered. In particular, much more caution is needed in the distal femur, which has abundant muscles surrounding it.
MeSH Terms
-
Adult
Aged
External Fixators/*adverse effects
Female
Femoral Fractures/*surgery
Fracture Fixation/*adverse effects/methods
Fractures, Comminuted/*surgery
Humans
Leg Length Inequality/etiology
Male
Middle Aged
Peripheral Nerves/injuries
Retrospective Studies
Surgical Wound Infection/*etiology
Tibial Fractures/*surgery
Young Adult
Figure
Cited by 2 articles
-
Selection and Recommended Usage Guide of Temporary External Fixator
Seung-Jae Lim, Ki-Sun Sung, Chang-Wug Oh
J Korean Fract Soc. 2013;26(2):164-169. doi: 10.12671/jkfs.2013.26.2.164.Diagnosis and Management of Posttraumatic Chronic Osteomyelitis
Jong Hoon Kim, Yong Cheol Yoon, Young Woo Kim, Sung Ho Jung, Jong Keon Oh
J Korean Fract Soc. 2014;27(1):88-104. doi: 10.12671/jkfs.2014.27.1.88.
Reference
-
1. Watson JT, Coufal C. Treatment of complex lateral plateau fractures using Ilizarov techniques. Clin Orthop Relat Res. 1998. (353):97–106.
Article2. Watson JT, Moed BR, Karges DE, Cramer KE. Pilon fractures. Treatment protocol based on severity of soft tissue injury. Clin Orthop Relat Res. 2000. (375):78–90.3. Behrens F. General theory and principles of external fixation. Clin Orthop Relat Res. 1989. (241):15–23.
Article4. Casey D, McConnell T, Parekh S, Tornetta P 3rd. Percutaneous pin placement in the medial calcaneus: is anywhere safe? J Orthop Trauma. 2002. 16(1):26–29.
Article5. Blauth M, Bastian L, Krettek C, Knop C, Evans S. Surgical options for the treatment of severe tibial pilon fractures: a study of three techniques. J Orthop Trauma. 2001. 15(3):153–160.
Article6. Collinge C, Sanders R, DiPasquale T. Treatment of complex tibial periarticular fractures using percutaneous techniques. Clin Orthop Relat Res. 2000. (375):69–77.
Article7. Sirkin MS, Bono CM, Reilly MC, Behrens FF. Percutaneous methods of tibial plateau fixation. Clin Orthop Relat Res. 2000. (375):60–68.
Article8. Santi MD, Botte MJ. External fixation of the calcaneus and talus: an anatomical study for safe pin insertion. J Orthop Trauma. 1996. 10(7):487–491.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Clinical Analysis on Treatment of Tibial Fractures Using Ex-Fi-Re External Fixator
- Treatment of Wrist Frarture-Disluation using the Mini-External Fixator and Internal Fixation
- The Biomechanics of Hybrid External Fixator: Effectiveness of Bar to Ring Connection
- Treatment of a Difficult Periarticular Fracture of the Knee with a Circular External Fixator
- Treatment of periarticular open fractures of the tibia with ilizarov external fixator