Korean J Radiol.
2000 Sep;1(3):162-164. 10.3348/kjr.2000.1.3.162.
Teratoma with Malignant Transformation in the Anterior Mediastinum: A Case Report
- Affiliations
-
- 1Department of Radiology, St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea. jijung@cmc.cuk.ac.kr
- KMID: 877077
- DOI: http://doi.org/10.3348/kjr.2000.1.3.162
Abstract
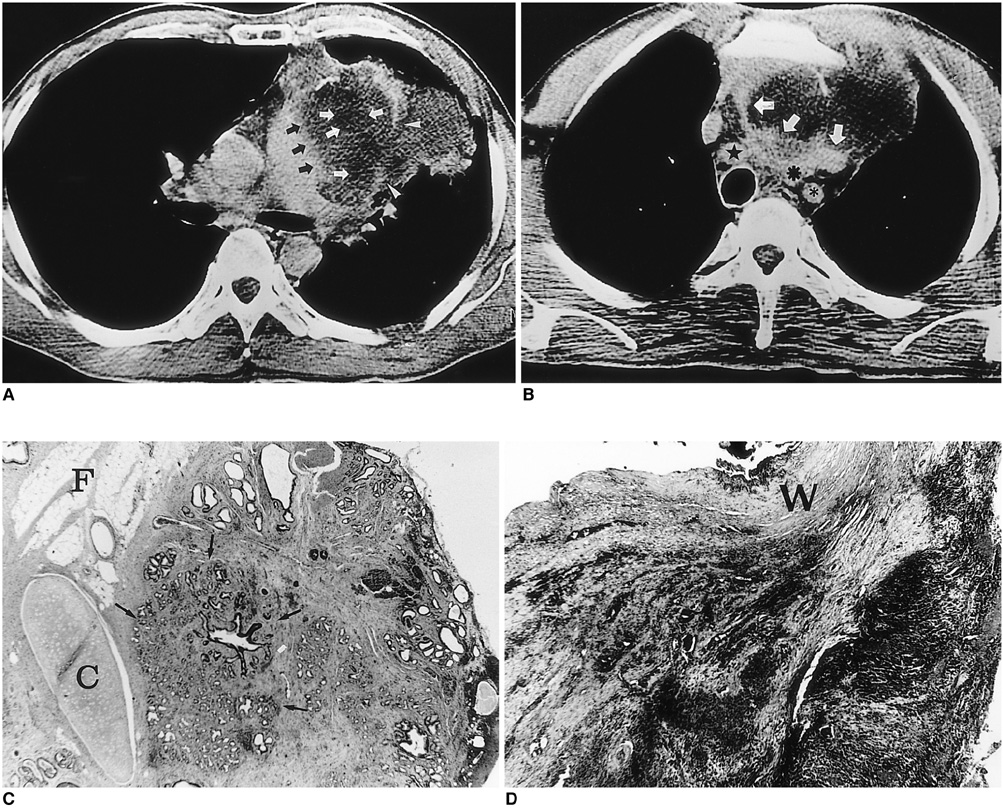
- Malignant transformation of teratoma in the anterior mediastinum is rare; the mass usually has a long history and is seen in older patients. We report a case of teratoma with malignant transformation in the anterior mediastinum, complicated by rupture. CT revealed a lobulated, inhomogeneous cystic mass with a fat com-ponent and wall calcifications. The lateral wall was disrupted and consolidation in the adjacent left upper lobe was noted, suggesting rupture. A heterogeneously enhanced solid portion, obliterating the fat plane between the mass and the great vessels was present in the medial aspect of the mass, and pathologic examina-tion demonstrated the presence of adenocarcinoma.
MeSH Terms
Figure
Reference
-
1. Ulbright TM, Loehrer PJ, Roth LM, Einhorn LH, Williams SD, Clark SA. The development of non-germ cell malignancies within germ cell tumors. A clinicopathologic study of 11 cases. Cancer. 1984. 54:1824–1833.2. Ahmed T, Bosl GJ, Hajdu SI. Teratoma with malignant transformation in germ cell tumors in men. Cancer. 1985. 56:860–863.3. Morinaga S, Nomori H, Kobayashi R, Atsumi Y. Well-differentiated adenocarcinoma arising from mature cystic teratoma of the mediastinum (teratoma with malignant transformation): Report of a surgical case. Am J Clin Pathol. 1994. 101:531–534.4. Sasaka K, Kurihara Y, Nakajima Y, et al. Spontaneous rupture: a complication of benign mature teratomas of the mediastinum. AJR. 1998. 170:323–328.5. Chadha S, Schaberg A. Malignant transformation in benign cystic teratomas: dermoids of the ovary. Eur J Obstet Gynecol Reprod Biol. 1988. 19:329–338.6. Curling OM, Potsides PN, Hudson CN. Malignant change in benign cystic teratoma of the ovary. Br J Obstet Gynecol. 1979. 86:399–402.7. Knapp RH, Hurt RD, Payne WS, et al. Malignant germ cell tumors of the mediastinum. J Thorac Cardiovasc Surg. 1985. 89:82–89.8. Moeller KH, Rosado-de-Christenson ML, Templeton PA. Mediastinal mature teratoma: imaging features. AJR. 1997. 169:985–990.9. Choi S, Lee JS, Song KS, Lim T. Mediastinal teratoma: CT differentiation of ruptured and unruptured tumors. AJR. 1998. 171:591–594.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Adenocarcinoma Arising in benign Teratoma of Mediastinum: A case report
- Naturally Occurring Mediastinal Teratoma with Malignant Transformation in an Adult Male
- Malignant Teratoma of Prostatic Gland
- Rapidly Growing Mature Teratoma in the Anterior Mediastinum: Case Report
- Teratoma of the Pleura: A Case Report