Korean J Radiol.
2000 Sep;1(3):152-158. 10.3348/kjr.2000.1.3.152.
Effectiveness of MR Urography in the Evaluation of Kidney which Failed to Opacify during Excretory Urography: Comparison with Ultrasonography
- Affiliations
-
- 1Department of Radiology, Seoul National University Hospital, Seoul, Korea.
- KMID: 877075
- DOI: http://doi.org/10.3348/kjr.2000.1.3.152
Abstract
OBJECTIVE
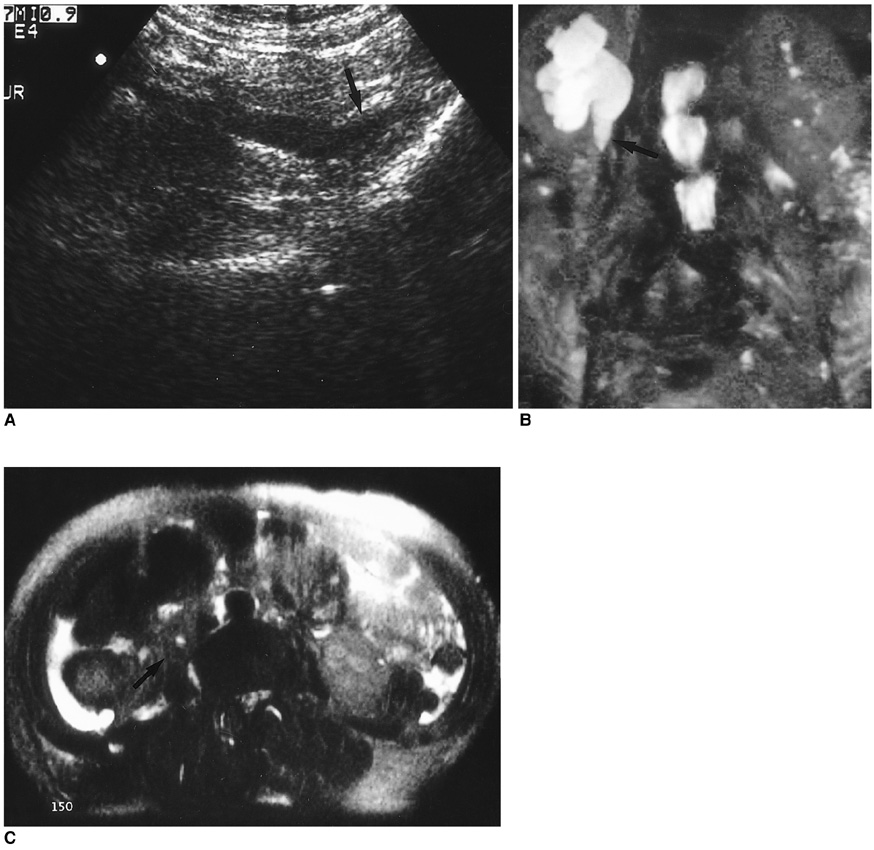
The purpose of this study was to compare the effectiveness of MR urography (MRU) with that of ultrasonography (US) in the evaluation of urinary tract when this failed to opacify during excretory urography (EXU). MATERIALS AND METHODS: Twelve urinary tracts in 11 patients were studied. In each case, during EXU, the urinary system failed to opacify within one hour of the injection of contrast media, and US revealed dilatation of the pelvocalyceal syytem. Patients underwent MRU, using a HASTE sequence with the breath-hold technique; multi-slice acquisition was then performed, and the images were reconstructed using maximal intensity projection. Each set of images was evaluated by three radiologists to determine the presence, level, and cause of urinary tract obstruction. RESULTS: Obstruction was present in all twelve cases, and in all of these, MRU accurately demonstrated its level. In this respect, however, US was successful in only ten. The cause of obstruction was determined by MRU in eight cases, but by US in only six. In all of these six, MRU also successfully demonstrated the cause. CONCLUSION: MRU is an effective modality for evaluation of the urinary tract when this fails to opacify during EXU, and appears to be superior to US in demon-strating the level and cause of obstruction.
Keyword
MeSH Terms
Figure
Reference
-
1. Cronan JJ. Contemporary concepts in imaging urinary tract obstruction. Radiol Clin North Am. 1991. 29:527–542.2. Webb JAW. Ultrasonography in the diagnosis of renal obstruction. Sensitive but not very specific. Br Med J. 1990. 301:944–946.3. Regan F, Bohlman ME, Khazan R, Rodriguez R, Schultze-Haakh H. MR urography using HASTE imaging in the assessment of ureteric obstruction. AJR. 1996. 1678:1115–1120.4. Tang Y, Yamashita Y, Namimoto T, et al. The value of MR urography that uses HASTE sequences to reveal urinary tract disorders. AJR. 1996. 167:1497–1502.5. O'Malley ME, Soto JA, Yucel EK, Hussain S. MR urography: evaluation of three-dimenstional fast spin-echo technique in patients with hydronephrosis. AJR. 1997. 168:387–392.6. Nolte-Ernsting CC, Bucker A, Adam GB, et al. Gadolinium-enhanced excretory MR urography after low-dose diuretic injection: comparison with conventional excretory urography. Radiology. 1998. 209:147–157.7. Rothpearl A, Frager D, Subramanian A, et al. MR urography: technique and application. Radiology. 1995. 194:125–130.8. Hattery RR, King BF. Technique and application of MR urography. Radiology. 1995. 194:25–27.9. Roy C, Saussine C, Guth S, et al. MR urography in the evaluation of urinary tract obstruction. Abdom Imaging. 1998. 23:27–34.10. Kiefer B, Grassner J, Hausman R. Image acquisition in a second with half-Fourier acquisition single shot turbo spin-echo. J Magn Reson Imaging. 1994. 4:Suppl. 86–87.11. Sigmund G, Stoever B, Zimmerhackl LB, Frankenschmidt A, Nitzsche E, Leititis JU. RARE-MR urography in the diagnosis of upper urinary tract abnormalities in children. Pediatr Radiol. 1991. 21:416–420.12. Kamholtz RG, Cronan JJ, Dorfman GS. Obstruction and the minimally dilated renal collecting system: US evaluation. Radiology. 1989. 170:51–53.13. Hill MC, Rich JI, Mardiat JG, Finder CA. Sonography vs. excretory urography in acute flank pain. AJR. 1985. 144:1235–1238.14. Malave SR, Neiman HL, Spies SM, Cisternino SJ, Adamo G. Diagnosis of hydronephrosis: comparision of radionuclide scanning and sonography. AJR. 1980. 135:1179–1185.15. Li W, Chavez D, Edelman RR, Prasad PV. Magnetic resonance urography by breath-hold contrast-enhanced three-dimenstional FISP. J Magn Reson Imaging. 1997. 7:309–311.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of Ultrasonography, Computed Tomography and Excretory Urography in Staging of Renal Cell Carcinoma
- The Diagnostic Efficacy of Abdominal Ultrasonography for Evaluation of Children with Urinary Tract Infection
- The evaluation of kidney scan: on comparison with excretory urography
- A Comparative Study of Excretory Urography and Renal Angiography on Blunt Renal Trauma
- Value of Excretory Urography in Chronic Epididymitis - Analysis of 60 Cases -