Korean J Radiol.
2001 Sep;2(3):145-150. 10.3348/kjr.2001.2.3.145.
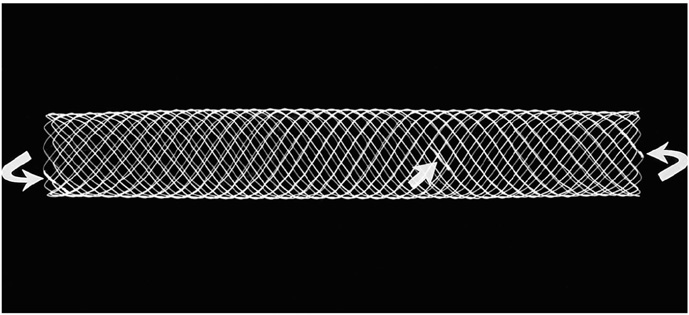
A Newly Designed Nitinol Stent: Early Clinical Experience in the Treatment of Iliac Artery Stenoses and Occlusions
- Affiliations
-
- 1Department of Radiology, Seoul National University College of Medicine, Seoul, Korea. parkjh@radcom.snu.ac.kr
- KMID: 754099
- DOI: http://doi.org/10.3348/kjr.2001.2.3.145
Abstract
OBJECTIVE
To investigate the effectiveness of the newly designed Niti-S stent in the management of iliac arterial stenoses and occlusions. MATERIALS AND METHODS: Stenoses (n=25) or occlusions (n=5) in the iliac arteries of 25 patients (30 limbs) were treated. The site of the lesions was the common (n=15) or external (n=11) iliac artery, or both (n=4). Eight limbs were treated for diffuse disease, six for highly eccentric lesion, five for occlusive lesion, and 11 for failed angioplasty. RESULTS: In all patients, technical success was achieved without major complications. One death, not procedure-related, occurred within 30 days. Ankle-brachial indexes improved from 0.63 +/- 0.30 to 0.99 +/- 0.21, and ischemic symptoms showed improvement in 22 patients (88%). Fontaine classifications before stenting, namely IIa(n=3), IIb(n=16), III(n=2), and IV(n=4) improved to I(n=17), IIa(n=5), and IV(n=3). Follow-up over a 27 (mean, 19.8 +/- 8)-month period showed that cumulative patency rates were 95.8% at 1 year and 86.2% at 2 and 3 years. No significant decrease in the mean ankle-brachial index was observed. CONCLUSION: The Niti-S stent appears to be a safe and effective device for the treatment of iliac stenoses and occlusions. These preliminary results require confirmation with a larger series.
MeSH Terms
Figure
Reference
-
1. Murphy KD, Encarnacion CE, Le VA, Palmaz JC. Iliac artery stent placement with the Palmaz stent; follow-up study. J Vasc Interv Radiol. 1995. 6:321–329.2. Liermann D, Strecker EP, Peters J. The Strecker stent: indications and results in iliac and femoropopliteal arteries. Cardiovasc Intervent Radiol. 1992. 1:298–305.3. Murphy TP, Webb MS, Lambiase RE, et al. Percutaneous revascularization of complex iliac artery stenoses and occlusions with use of Wallstents: three-year experience. J Vasc Interv Radiol. 1996. 7:21–27.4. Yedlich JW, Ferral H, Bjarnason H, Hunter DW, Castaneda-Zuniga WR, Amplatz K. Chronic iliac artery occlusion: primary recanalization with endovascular stents. J Vasc Interv Radiol. 1994. 5:843–847.5. Bosch JL, Hunink MGM. Meta-analysis of the results of percutaneous transluminal angioplasty and stent placement for aortoiliac occlusive disease. Radiology. 1997. 204:87–96.6. Dotter CT, Buschmann RW, McKinney MK, Rosch J. Transluminal expandable nitinol coil stent grafting: preliminary report. Radiology. 1983. 147:259–260.7. Cragg AH, Dejong S, Barnhart W, Landas S, Smith TP. Preliminary evaluation of the Cragg stent (abstr). Radiology. 1992. 185(P):162.8. Cragg AH, Lund G, Rysavy JA, Salomonowitz E, Castaneda-Zuniga WR, Amplatz K. Percutaneous arterial grafting. Radiology. 1984. 150:45–49.9. Foelich JJ, Alfke H, Wilke A, et al. Effects of nitinol Strecker stent placement on vascular response in normal and stenotic porcine iliac arteries. J Vasc Interv Radiol. 1999. 10:329–338.10. Shaw JW. Management of aortoiliac occlusive vascular disease with the Memotherm self-expanding nitinol stent. J Intervent Radiol. 1996. 11:119–127.11. Maynar M, Reyes R, Ferral H, et al. Cragg endopro system I: early experience. I. Femoral arteries. J Vasc Interv Radiol. 1997. 8:203–207.12. Hausegger KA, Cragg AH, Lammer J, et al. Iliac artery stent placement: clinical experience with a nitinol stent. Radiology. 1994. 190:199–202.13. Wakloo AK, Tio FO, Lieber BB, et al. Self-expandable nitinol stents in canine vertebral arteries: hemodynamics and tissue response. Am J Neuroradiol. 1995. 16:1043–1051.14. Schwarzenberg H, Muller-Hulsbeck S, Gluer CC, Steffens JC, Heller M. Evaluation of maximum neointima proliferation and plaque morphology in iliac self-expanding nitinol stents with intravascular sonography. AJR. 1998. 171:1627–1630.15. Lee KW, Park JH, Chung JW, Kim WS, Lee W, Yeon KM. Short-term effects of a new intravascular nitinol stent in canine arteries. Invest Radiol. 1999. 34:367–373.16. Pentecost MJ, Criqui MH, Dorros G, et al. Guidelines for peripheral percutaneous transluminal angioplasty of the abdominal aorta and lower extremity vessels. Circulation. 1994. 89:511–531.17. Rutherford RB, Necker GJ. Standards for evaluating and reporting the results of surgical and percutaneous therapy for peripheral arterial disease. J Vasc Interv Radiol. 1991. 2:169.18. McLean GK, Cekirge S, Weiss JP, Foster RG. Stent placement for iliac artery occlusions: modified "wire-loop" technique with use of the goose-neck loop snare. J Vasc Interv Radiol. 1994. 5:701–703.19. Palmaz JC, Laborde JC, Rivera FJ, et al. Stenting of the iliac arteries with the Palmaz stent: experience from a multicenter trial. Cardiovasc Intervent Radiol. 1992. 15:291–297.20. Schurmann K, Vorwerk D, Kulisch A, et al. Neointimal hyperplasia in low-profile nitinol stents, Palmaz stents, and Wallstents: a comparative experimental study. Cardiovasc Intervent Radiol. 1996. 19:248–254.21. Ballard JL, Sparks SR, Taylor FC, et al. Complications of iliac artery stent deployment. J Vasc Surg. 1996. 24:545–555.22. Blum U, Gabelmann A, Redecker M, et al. Percutaneous recanalization of iliac artery occlusions: results of a prospective study. Radiology. 1993. 189:536–540.23. Laborde JC, Dougherty S, Rivera FJ, Encarnacion CE, Palmaz JC. Influence of anatomic distribution of atherosclerosis in the outcome of iliac revascularization (abstract). J Vasc Interv Radiol. 1992. 3:31.24. Stokes KR, Strunk HM, Campbell DR, Gibbons GW, Wheeler HG, Clouse ME. Five-year result in iliac and femoropopliteal angioplasty in diabetic patients. Radiology. 1990. 174:977–982.25. Gunther RW, Vorwerk D, Bohndorf K, Peters I, el-Din A, Messmer B. Iliac and femoral artery stenoses and occlusions: treatment with intravascular stents. Radiology. 1989. 172:725–730.26. Long AL, Page PE, Raynaud AC, et al. Percutaneous iliac artery stent: angiographic long-term follow-up. Radiology. 1991. 180:771–778.27. Fitzgerald GA. Dipyridamole. N Engl J Med. 1987. 316:1247–1257.28. Montalescot G. Value of antiplatelet therapy in preventing thrombotic events in generalized vascular disease. Clin Cardiol. 2000. 23:18–22.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Efficacy and Safety of a Newly Developed Self- Expanding Open-Cell Type Nitinol Stent for Peripheral Arteries: A Preclinical Study in Minipigs
- Endovascular Stent Placement for the Treatment of Superficial Femoral Artery Stenoses and Occlusions
- Placement of Balloon-Expandable Intraluminal Stent in Recurrent Iliac Artery Stenosis
- A Case of Complex Restenosis of Aortoiliac Stent Mimicking Downward Stent Migration
- Treatment of Malignant Gastroduodenal Obstruction with Using a Newly Designed Complex Expandable Nitinol Stent: Initial Experiences