Korean J Radiol.
2003 Sep;4(3):146-152. 10.3348/kjr.2003.4.3.146.
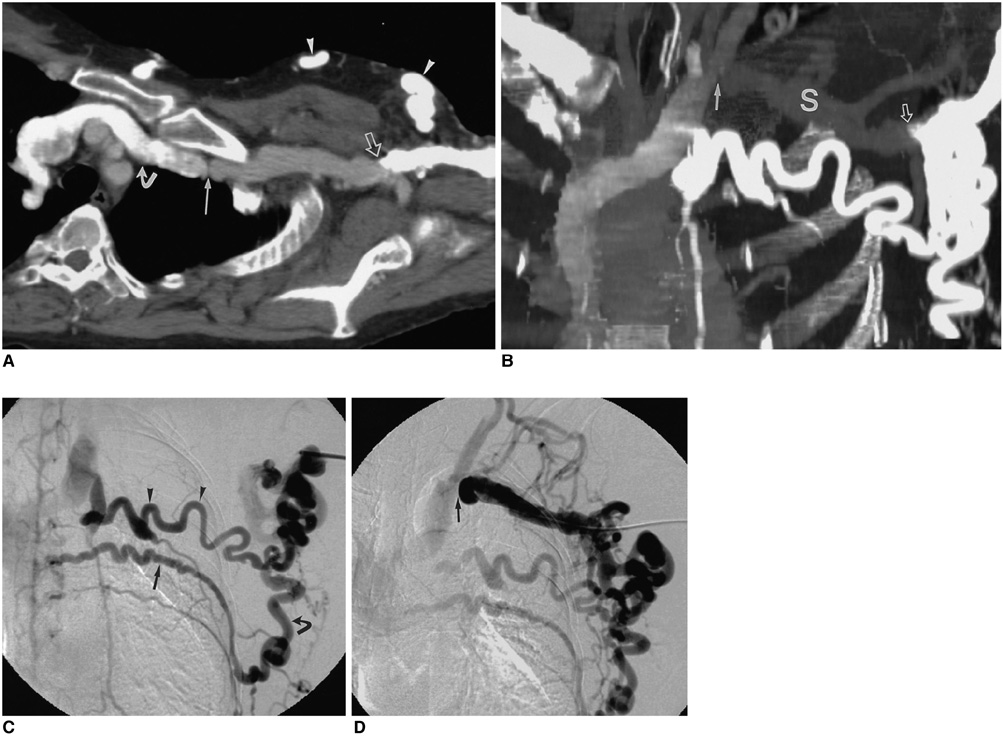
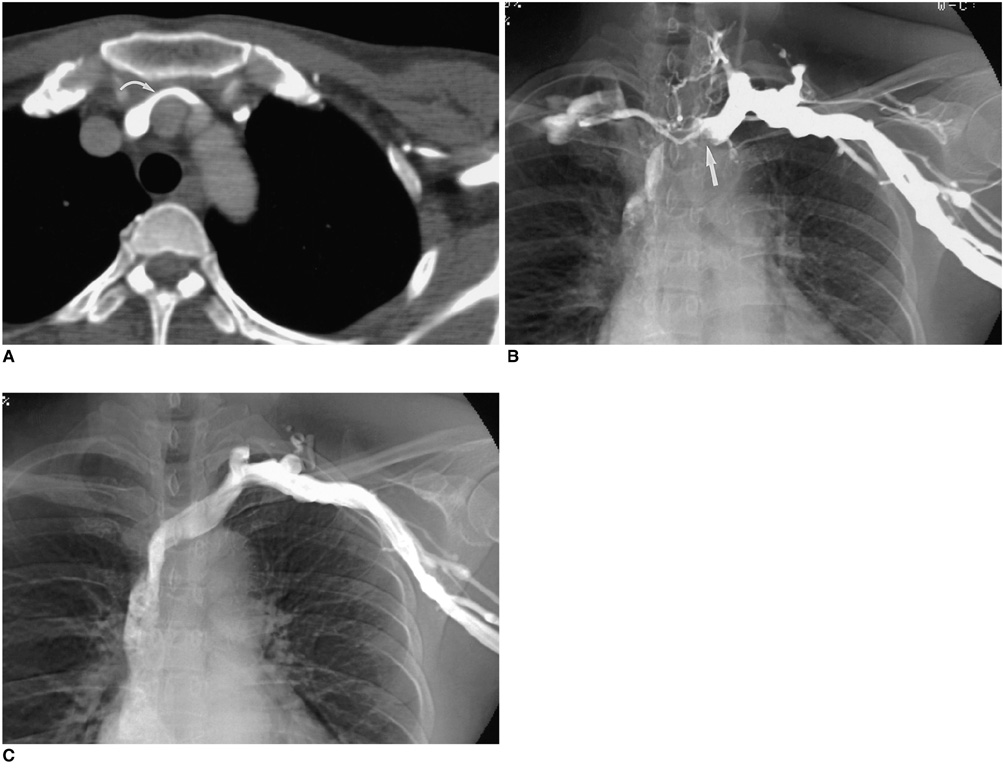
Role of CT Venography in the Diagnosis and Treatment of Benign Thoracic Central Venous Obstruction
- Affiliations
-
- 1Department of Radiology, Seoul National University College of Medicine; Institute of Radiation Medicine, SNUMRC; and Clinical Research Institute, Seoul National University Hospital. chungjw@radcom.snu.ac.kr
- KMID: 754017
- DOI: http://doi.org/10.3348/kjr.2003.4.3.146
Abstract
OBJECTIVE
To evaluate the role of CT venography in the diagnosis and treatment of benign thoracic central venous obstruction. MATERIALS AND METHODS: Eighteen patients who had undergone both CT venography and digital subtraction venography were prospectively enrolled in this study. The following features were analyzed by two observers: the cause, degree, and extent of venous obstruction; associated thrombosis; and implications for the planning of treatment. CT venography and digital subtraction venography were compared in defined venous segments, and the degree of obstruction, and correlation was expressed using Spearman's rank correlation coefficient. RESULTS: In all patients, CT venography depicted the causes of obstruction, including extrinsic compression of the left brachiocephalic vein, and mediastinal inflammatory pseudotumor. Interobserver agreement regarding classification of the degree of obstruction was judged as good for CT venography (k=0.864), and in evaluating this, there was significant correlation between CT venography and digital subtraction venography (reader 1: Rs = 0.58, p < 0.01; reader 2: Rs = 0.56, p < 0.01). In evaluating the status of central veins proximal to long segmental obstruction, and associated thrombosis, CT venography was superior to digital subtraction venography. In half of all patients, the findings of CT venography led to changes in the treatment plan. CONCLUSION: The findings of CT venography correlated closely with those of digital subtraction venography, and the former accurately depicted the degree and extent of benign venous obstruction.
Keyword
Figure
Cited by 1 articles
-
MDCT Application in the Vascular System
Hwan Seok Yong
J Korean Med Assoc. 2007;50(1):25-32. doi: 10.5124/jkma.2007.50.1.25.
Reference
-
1. Yim CD, Sane SS, Bjarnason H. Superior vena cava stenting. Radiol Clin North Am. 2000. 38:409–424.2. Parish JM, Marschke RF Jr, Dines DE, Lee RE. Etiologic considerations in superior vena cava syndrome. Mayo Clin Proc. 1981. 56:407–413.3. Qanadli SD, el-Hajjam M, Bruckert F, et al. Helical CT phlebography of the superior vena cava: diagnosis and evaluation of venous obstruction. AJR Am J Roentgenol. 1999. 172:1327–1333.4. Glanz S, Gordon DH, Lipkowitz GS, Butt KM, Hong J, Sclafani SJ. Axillary and subclavian vein stenosis: percutaneous angioplasty. Radiology. 1988. 168:371–373.5. Schwab SJ, Quarles LD, Middleton JP, Cohan RH, Saeed M, Dennis VW. Hemodialysis-associated subclavian vein stenosis. Kidney Int. 1988. 33:1156–1159.6. Surratt RS, Picus D, Hicks ME, Darcy MD, Kleinhoffer M, Jendrisak M. The importance of preoperative evaluation of the subclavian vein in dialysis access planning. AJR Am J Roentgenol. 1991. 156:623–625.7. el-Shahawy MA, Gadallah MF, Teitelbaum GP, Kaptein E, Akmal M. Compression of the left brachiocephalic vein by the innominate artery resulting in massive arm edema in a hemodialysis patient. Am J Nephrol. 1992. 12:108–110.8. Glanz S, Gordon DH, Butt KM, Hong J, Lipkowitz GS. The role of percutaneous angioplasty in the management of chronic hemodialysis fistulas. Ann Surg. 1987. 206:777–781.9. Gray RJ, Horton KM, Dolmatch BL, et al. Use of Wallstents for hemodialysis access-related venous stenoses and occlusions untreatable with balloon angioplasty. Radiology. 1995. 195:479–484.10. Haage P, Vorwerk D, Piroth W, Schuermann K, Guenther RW. Treatment of hemodialysis-related central venous stenosis or occlusion: results of primary Wallstent placement and follow-up in 50 patients. Radiology. 1999. 212:175–180.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Spiral CT Venography in Central Venous Obstruction
- Central Venous Catheter Induced Thrombotic Obstruction of the Superior Vena Cava
- Significance of Contrast Enhanced Rapid MR Sequence(True FISP) in Deep Vein Thrombosis
- The Interobserver Agreement between Residents and Experienced Radiologists for Detecting Pulmonary Embolism and DVT with Using CT Pulmonary Angiography and Indirect CT Venography
- Reassessment of the Diagnostic Role of Technetium-99m-RBC Venography for Leg Venous Diseases