Korean J Radiol.
2007 Feb;8(1):22-31. 10.3348/kjr.2007.8.1.22.
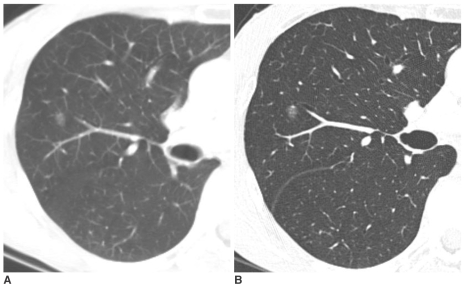
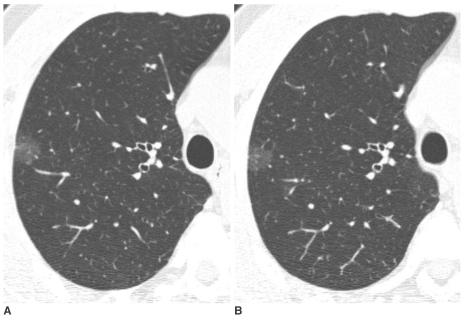
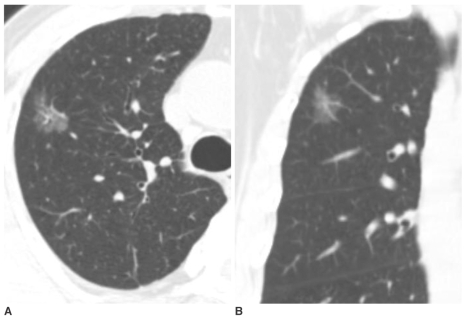
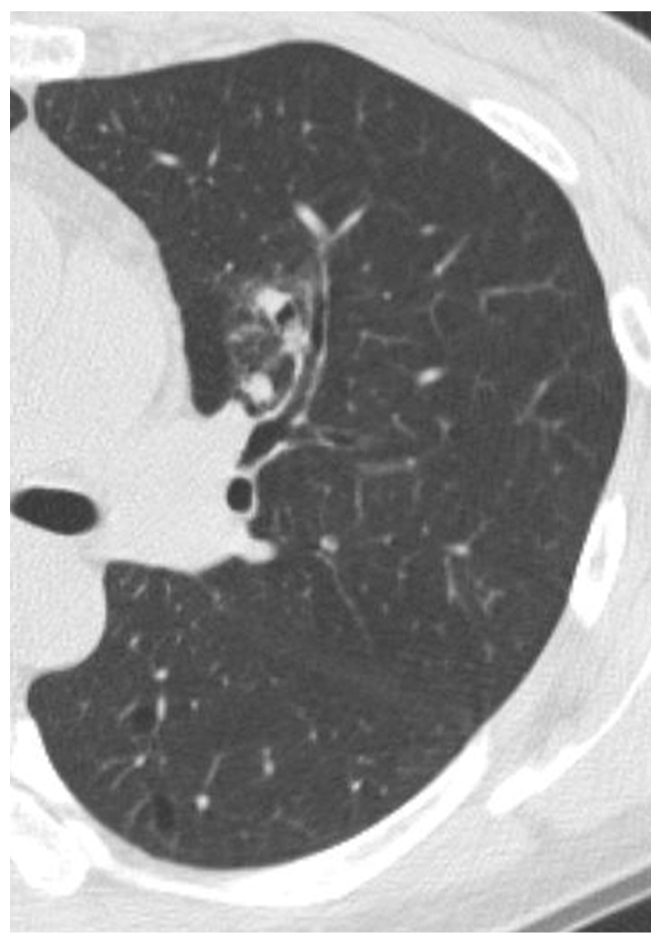
Nodular Ground-Glass Opacities on Thin-section CT: Size Change during Follow-up and Pathological Results
- Affiliations
-
- 1Department of Radiology, Seoul National University College of Medicine and the Institute of Radiation Medicine, Seoul National University Medical Research Center, Seoul, Korea. jmgoo@plaza.snu.ac.kr
- 2Department of Internal Medicine, Seoul National University College of Medicine, Seoul, Korea.
- 3Department of Thoracic and Cardiovascular Surgery, Seoul National University College of Medicine, Seoul, Korea.
- KMID: 753862
- DOI: http://doi.org/10.3348/kjr.2007.8.1.22
Abstract
OBJECTIVE
To evaluate the inter-group differences in growth and the pathological results of nodular ground-glass opacities (GGOs) according to their size and focal solid portions. MATERIALS AND METHODS: Ninety-six nodular GGOs in 55 individuals followed by CT for at least one month from an initial chest CT were included. Forty nodular GGOs in 30 individuals were pathologically confirmed to be: adenocarcinoma (n = 15), bronchioloalveolar carcinoma (BAC) (n = 11), atypical adenomatous hyperplasia (AAH) (n = 8), focal interstitial fibrosis (n = 5) and aspergillosis (n = 1). Lesions were categorized based on high-resolution CT findings: pure nodular GGO (PNGGO) < or = 10 mm, PNGGO > 10 mm, mixed nodular GGO (MNGGO) < or = 10 mm, and MNGGO > 10 mm. In each group, the change in size during the follow-up period, the pathological results and the rate of malignancy were evaluated. RESULTS: Three MNGGO lesions, and none of the PNGGO, grew during the follow-up period. Resected PNGGOs < or = 10 mm were AAH (n = 6), BAC (n = 5), and focal interstitial fibrosis (n = 1). Resected PNGGOs > 10 mm were focal interstitial fibrosis (n = 4), AAH (n = 2), BAC (n = 2), and adenocarcinoma (n = 2). Resected MNGGOs < or = 10 mm were adenocarcinoma (n = 2), and BAC (n = 1). Resected MNGGOs > 10 mm were adenocarcinoma (n = 11), BAC (n = 3), and aspergillosis (n = 1). CONCLUSION: Mixed nodular GGOs (MNGGOs) had the potential for growth; most were pathologically adenocarcinoma or BAC. By contrast, PNGGOs were stable for several months to years; most were AAH, BAC, or focal interstitial fibrosis.
MeSH Terms
Figure
Cited by 2 articles
-
Assessing the Blood Supply Status of the Focal Ground-Glass Opacity in Lungs Using Spectral Computed Tomography
Guanfu Liu, Mengying Li, Guosheng Li, Zhiyong Li, Ailian Liu, Renwang Pu, Huizhi Cao, Yijun Liu
Korean J Radiol. 2018;19(1):130-138. doi: 10.3348/kjr.2018.19.1.130.A New Method of Measuring the Amount of Soft Tissue in Pulmonary Ground-Glass Opacity Nodules: a Phantom Study
Kyung Won Lee, Jung-Gi Im, Tae Jung Kim, Chang Min Dae
Korean J Radiol. 2008;9(3):219-225. doi: 10.3348/kjr.2008.9.3.219.
Reference
-
1. Henschke CI, Yankelevitz DF, Mirtcheva R, McGuinness G, McCauley D, Miettinen OS; ELCAP Group. CT screening for lung cancer: frequency and significance of part-solid and nonsolid nodules. AJR Am J Roentgenol. 2002; 178:1053–1057. PMID: 11959700.2. Nakata M, Saeki H, Takata I, Segawa Y, Mogami H, Mandai K, et al. Focal ground-glass opacity detected by low-dose helical CT. Chest. 2002; 121:1464–1467. PMID: 12006429.
Article3. Hasegawa M, Sone S, Takashima S, Li F, Yang ZG, Maruyama Y, et al. Growth rate of small lung cancers detected on mass CT screening. Br J Radiol. 2000; 73:1252–1259. PMID: 11205667.
Article4. Aoki T, Nakata H, Watanabe H, Nakamura K, Kasai T, Hashimoto H, et al. Evolution of peripheral lung adenocarcinomas: CT findings correlated with histology and tumor doubling time. AJR Am J Roentgenol. 2000; 174:763–768. PMID: 10701622.5. Noguchi M, Morikawa A, Kawasaki M, Matsuno Y, Yamada T, Hirohashi S, et al. Small adenocarcinoma of the lung. Histologic characteristics and prognosis. Cancer. 1995; 75:2844–2852. PMID: 7773933.
Article6. Kodama K, Higashiyama M, Yokouchi H, Takami K, Kuriyama K, Kusunoki Y, et al. Natural history of pure ground-glass opacity after long-term follow-up of more than 2 years. Ann Thorac Surg. 2002; 73:386–392. PMID: 11845847.
Article7. Kakinuma R, Ohmatsu H, Kaneko M, Kusumoto M, Yoshida J, Nagai K, et al. Progression of focal pure ground-glass opacity detected by low-dose helical computed tomography screening for lung cancer. J Comput Assist Tomogr. 2004; 28:17–23. PMID: 14716227.
Article8. Nakajima R, Yokose T, Kakinuma R, Nagai K, Nishiwaki Y, Ochiai A. Localized pure ground-glass opacity on high-resolution CT: histologic characteristics. J Comput Assist Tomogr. 2002; 26:323–329. PMID: 12016356.
Article9. Takashima S, Sone S, Li F, Maruyama Y, Hasegawa M, Matsushita T, et al. Small solitary pulmonary nodules (< or =1 cm) detected at population-based CT screening for lung cancer: Reliable high-resolution CT features of benign lesions. AJR Am J Roentgenol. 2003; 180:955–964. PMID: 12646435.10. Colby TV, Noguchi M, Henschke C, Vazquez MF, Geiniger K , Yokosa T, et al. Travis WD, Brambilla E, Muller-Hermelink HK, Harris CC, editors. Adenocarcinoma. World Health Organization classification of tumours: Tumors of the lung, pleura, thymus and heart. 2004. 1st ed. Lyon: IARC Press;p. 35–44.11. Shimosato Y, Suzuki A, Hashimoto T, Nishiwaki Y, Kodama T, Yoneyama T, et al. Prognostic implications of fibrotic focus (scar) in small peripheral lung cancers. Am J Surg Pathol. 1980; 4:365–373. PMID: 7425202.
Article12. Miller R. Bronchioloalveolar cell adenomas. Am J Surg Pathol. 1990; 14:904–912. PMID: 2403196.
Article13. Mori M, Tezuka F, Chiba R, Funae Y, Watanabe M, Nukiwa T, et al. Atypical adenomatous hyperplasia and adenocarcinoma of the human lung: their heterology in form and analogy in immunohistochemical characteristics. Cancer. 1996; 77:665–674. PMID: 8616758.
Article14. Suzuki K, Nagai K, Yoshida J, Yokose T, Kodama T, Takahashi K, et al. The prognosis of resected lung carcinoma associated with atypical adenomatous hyperplasia: a comparison of the prognosis of well-differentiated adenocarcinoma associated with atypical adenomatous hyperplasia and intrapulmonary metastasis. Cancer. 1997; 79:1521–1526. PMID: 9118033.15. Suzuki K, Takahashi K, Yoshida J, Nishimura M, Yokose T, Nishiwaki Y, et al. Synchronous double primary lung carcinomas associated with multiple atypical adenomatous hyperplasia. Lung Cancer. 1998; 19:131–139. PMID: 9567250.
Article16. Park CM, Goo JM, Lee HJ, Lee CH, Chung DH, Kim HC, et al. CT findings of atypical adenomatous hyperplasia of the lung. Korean J Radiol. 2006; 7:80–86. PMID: 16799268.17. Kodama K, Doi O, Higashiyama M, Yokouchi H. Intentional limited resection for selected patients with T1 N0 M0 non-small cell lung cancer: a single-institution study. J Thorac Cardiovasc Surg. 1997; 114:347–353. PMID: 9305186.18. Pastorino U, Valente M, Bedini V, Infante M, Tavecchio L, Ravasi G. Limited resection for stage 1 lung cancer. Eur J Surg Oncol. 1991; 17:42–46. PMID: 1995356.19. Nakamura H, Saji H, Ogata A, Saijo T, Okada S, Kato H. Lung cancer patients showing pure ground-glass opacity on computed tomography are good candidates for wedge resection. Lung Cancer. 2004; 44:61–68. PMID: 15013584.
Article20. Watanabe S, Watanabe T, Arai K, Kasai T, Haratake J, Urayama H. Results of wedge resection for focal bronchioloalveolar carcinoma showing pure ground-glass attenuation on computed tomography. Ann Thorac Surg. 2002; 73:1071–1075. PMID: 11996243.
Article21. Nakata M, Sawada S, Yamashita M, Saeki H, Kurita A, Takashima S, et al. Objective radiologic analysis of ground-glass opacity aimed at curative limited resection for small peripheral non-small cell lung cancer. J Thorac Cardiovasc Surg. 2005; 129:1226–1231. PMID: 15942561.
Article22. Yoshida J, Nagai K, Yokose T, Nishimura M, Kakinuma R, Ohmatsu H, et al. Limited resection trial for pulmonary ground-glass opacity nodules: fifty-case experience. J Thorac Cardiovasc Surg. 2005; 129:991–996. PMID: 15867771.
Article23. Kim KG, Goo JM, Kim JH, Lee HJ, Min BG, Bae KT, et al. Computer-aided diagnosis of localized ground-glass opacity in the lung at CT: initial experience. Radiology. 2005; 237:657–661. PMID: 16192320.
Article24. Nagao M, Murase K, Yasuhara Y, Ikezoe J, Eguchi K, Mogami H, et al. Measurement of localized ground-glass attenuation on thin-section computed tomography images: correlation with the progression of bronchioloalveolar carcinoma of the lung. Invest Radiol. 2002; 37:692–697. PMID: 12447003.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pulmonary Manifestations of Fat Embolism on Thin-section CT: A Case Report
- Squalene Aspiration Pneumonia: Thin-Section CT and Histopathologic Findings
- Thin-Section CT Findings of Arc-Welders' Pneumoconiosis
- Comparison of the CT and Pathologic Findings of Pulmonary Fat Embolism Induced by Triolein and Oleic Acid in Rabbits
- The Clinical Approach to Nodular Ground Glass Opacity in the Lung