Yonsei Med J.
2007 Jun;48(3):457-464. 10.3349/ymj.2007.48.3.457.
Early Clinical Experience with the Mobi-C Disc Prosthesis
- Affiliations
-
- 1Department of Neurosurgery, Ajou University, School of Medicine, Suwon, Korea.
- 2Department of Neurosurgery, Yonsei University College of Medicine, Seoul, Korea. ydoheum@yumc.yonsei.ac.kr
- KMID: 724101
- DOI: http://doi.org/10.3349/ymj.2007.48.3.457
Abstract
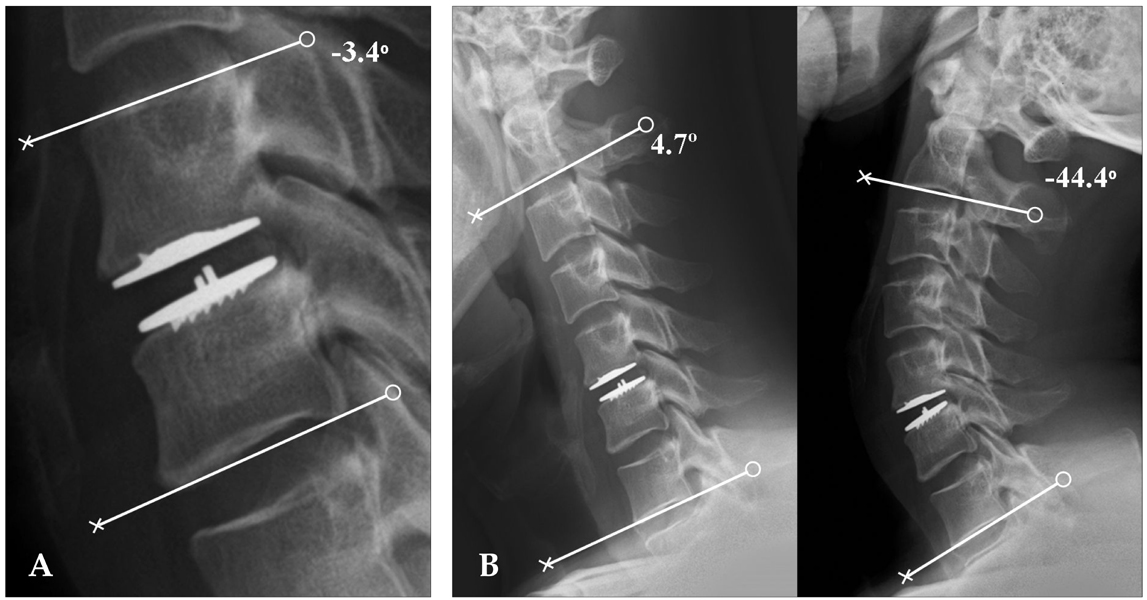
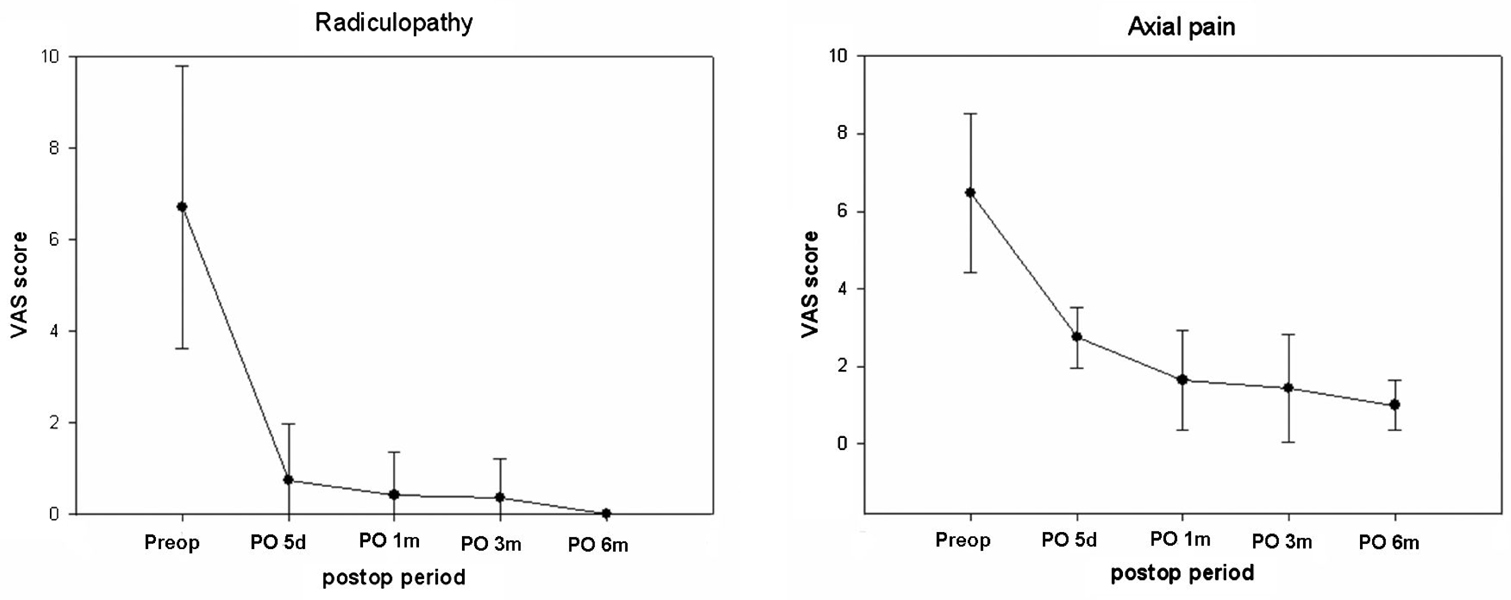
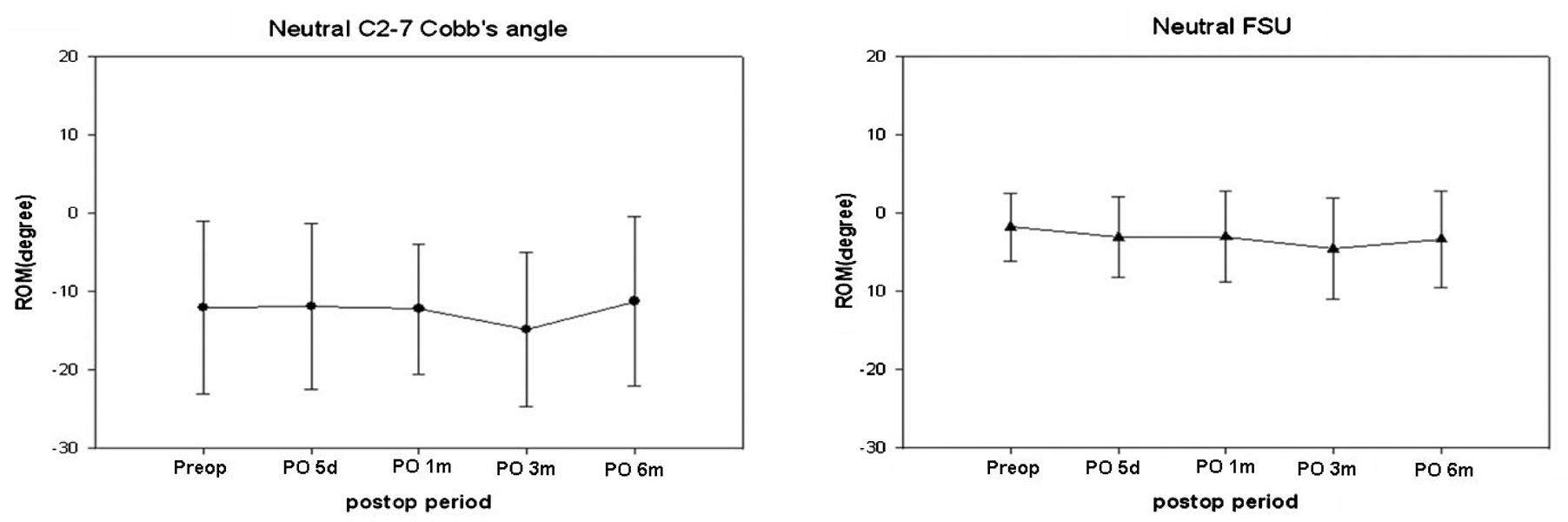
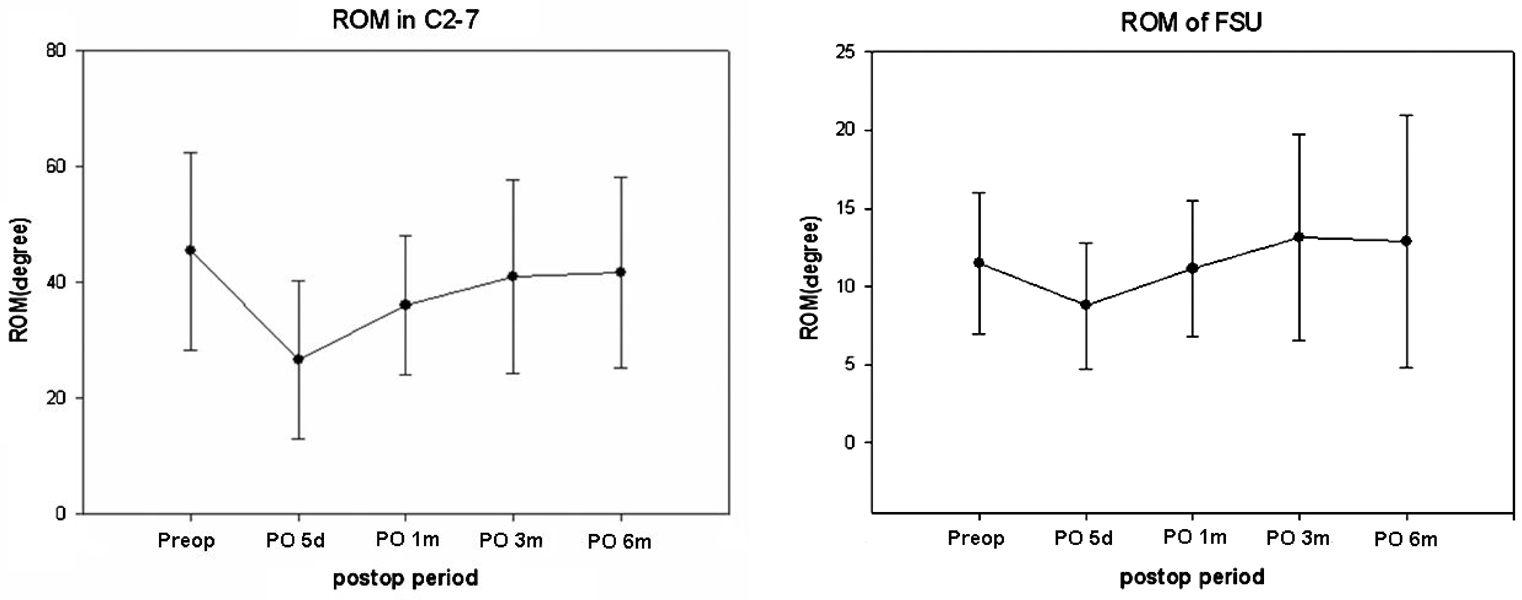
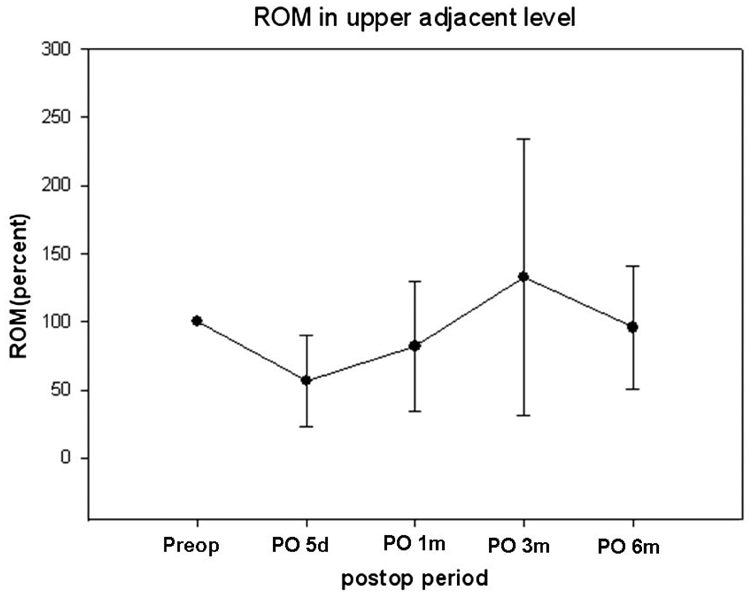
- PURPOSE
We have experienced 23 patients who had underwent cervical disc replacement with Mobi-C disc prosthesis and analyzed their radiological results to evaluate its efficacy. PATIENTS AND METHODS: This study was performed on 23 patients with degenerative cervical disc disease who underwent CDR with Mobi-C disc prosthesis from March 2006 to June 2006. RESULTS: The age of the study population ranged from 31 to 62 years with mean of 43 years, and 16 male and 7 female cases. Regarding axial pain, the average preoperative VAS score was 6.47 +/- 1.4, while at final follow-up it was 1.4 +/- 0.7 (p < 0.001). The preoperatively VAS score for radiculopathy was 6.7 +/- 0.7 compared with an average score of 0 +/- 0 at the final follow-up (p < 0.001). At postoperative 6th month, Odom's criteria were excellent, good, or fair for all 23 patients (100%). 7 patients (30.4%) were classified as excellent, 15 patients (65.2%) as good, and 1 patients (4.4%) as fair. Prolo economic and functional rating scale was average 8.9 +/- 0.7 at postoperative 6th month. ROM in C2-7, ROM of FSU, and ROM in upper adjacent level were well preserved after CDR. CONSLUSION: This report would be the first document about the CDR with Mobi-C disc prosthesis in the treatment of degenerative cervical disc disease. CDR with Mobi-C disc prosthesis provided a favorable clinical and radiological outcome in this study. However, Long-term follow-up studies are required to prove its efficacy and ability to prevent adjacent segment disease.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
Radiological Analysis of Ponticulus Posticus in Koreans
Yong Jae Cho
Yonsei Med J. 2009;50(1):45-49. doi: 10.3349/ymj.2009.50.1.45.Clinical and Radiological Analysis of Cervical Arthroplasty Compared to Anterior Cervical Discectomy and Fusion in Cervical Disc Disease
Eun-Suk Park, Sung-Woo Roh, Jin-Hoon Park, Sang-Ryong Jeon, Seung-Chul Rhim, Chang-Jin Kim
J Korean Neurotraumatol Soc. 2009;5(2):83-88. doi: 10.13004/jknts.2009.5.2.83.
Reference
-
1. Yoon DH, Yi S, Shin HC, Kim KN, Kim SH. Clinical and radiological results following cervical arthroplasty. Acta Neurochir (Wien). 2006. 148:943–950.
Article2. Hilibrand AS, Robbins M. Adjacent segment degeneration and adjacent segment disease: the consequences of spinal fusion? Spine J. 2004. 4(6 Suppl):190S–194S.
Article3. Hilibrand AS, Carlson GD, Palumbo MA, Jones PK, Bohlman HH. Radiculopathy and myelopathy at segments adjacent to the site of a previous anterior cervical arthrodesis. J Bone Joint Surg Am. 1999. 81:519–528.
Article4. Robertson JT, Papadopoulos SM, Traynelis VC. Assessment of adjacent-segment disease in patients treated with cervical fusion or arthroplasty: a prospective 2-year study. J Neurosurg Spine. 2005. 3:417–423.
Article5. Hilibrand AS, Yoo JU, Carlson GD, Bohlman HH. The success of anterior cervical arthrodesis adjacent to a previous fusion. Spine. 1997. 22:1574–1579.
Article6. Goffin J, Casey A, Kehr P, Liebig K, Lind B, Logroscino C, et al. Preliminary clinical experience with the Bryan Cervical Disc Prosthesis. Neurosurgery. 2002. 51:840–847.
Article7. Durbhakula MM, Ghiselli G. Cervical total disc replacement, part I: rationale, biomechanics, and implant types. Orthop Clin North Am. 2005. 36:349–354.
Article8. Duggal N, Pickett GE, Mitsis DK, Keller JL. Early clinical and biomechanical results following cervical arthroplasty. Neurosurg Focus. 2004. 17:E9.
Article9. Wang Y, Xiao SH, Lu N, Zhang XS. Clinical report of cervical arthroplasty in management of spondylotic myelopathy. Zhonghua Wai Ke Za Zhi. 2004. 42:1333–1337.10. Tian W, Liu B, Li Q, Hu L, Li ZY, Yuan Q, et al. Early clinical outcome of cervical artificial disc replacement. Zhonghua Yi Xue Za Zhi. 2005. 85:37–40.11. Sekhon LH. Cervical arthroplasty in the management of spondylotic myelopathy: 18-month results. Neurosurg Focus. 2004. 17:E8.
Article12. Dmitriev AE, Cunningham BW, Hu N, Sell G, Vigna F, McAfee PC. Adjacent level intradiscal pressure and segmental kinematics following a cervical total disc arthroplasty: an in vitro human cadaveric model. Spine. 2005. 30:1165–1172.
Article13. Anderson PA, Sasso RC, Rouleau JP, Carlson CS, Goffin J. The Bryan Cervical Disc: wear properties and early clinical results. Spine J. 2004. 4(6 Suppl):303S–309S.
Article14. Bertagnoli R, Duggal N, Pickett GE, Wigfield CC, Gill SS, Karg A, et al. Cervical total disc replacement, part two: clinical results. Orthop Clin North Am. 2005. 36:355–362.
Article15. Pickett GE, Mitsis DK, Sekhon LH, Sears WR, Duggal N. Effects of a cervical disc prosthesis on segmental and cervical spine alignment. Neurosurg Focus. 2004. 17:E5.
Article16. Johnson JP, Lauryssen C, Cambron HO, Pashman R, Regan JJ, Anand N, et al. Sagittal alignment and the Bryan cervical artificial disc. Neurosurg Focus. 2004. 17:E14.
Article17. Vernon H, Mior S. The Neck Disability Index: a study of reliability and validity. J Manipulative Physiol Ther. 1991. 14:409–415.18. Prolo DJ, Oklund SA, Butcher M. Toward uniformity in evaluating results of lumbar spine operations. A paradigm applied to posterior lumbar interbody fusions. Spine. 1986. 11:601–606.
Article19. Goffin J, van Loon J, Van Calenbergh F, Plets C. Long- term results after anterior cervical fusion and osteosynthetic stabilization for fractures and/or dislocations of the cervical spine. J Spinal Disord. 1995. 8:499–508.20. Gore DR, Gardner GM, Sepic SB. Roentgenographic findings following anterior cervical fusion. Skeletal Radiol. 1986. 15:556–559.
Article21. Baba H, Furusawa N, Imura S, Kawahara N, Tsuchiya H, Tomita K. Late radiographic findings after anterior cervical fusion for spondylotic myeloradiculopathy. Spine. 1993. 18:2167–2173.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Early Radiological Analysis of Cervical Arthroplasty with Bryan and Mobi-C Cervical Disc Prosthesis
- Comparative Analysis of Cervical Disc Arthroplasty Using Two Types of Artificial Cervical Discs: Bryan(R) versus Mobi-C(R)
- Atypical Heterotopic Bone Formation Rear to the Functioning Cervical Artificial Disc Prosthesis Causing Cervical Spondylotic Myelopathy
- Acute Paraplegia Due to Nucleus Herniation of a Mobi-C Implant without Trauma: Case Report of a Rare Complication
- A Comparison Study of Four Cervical Disk Arthroplasty Devices Using Finite Element Models