Ann Hepatobiliary Pancreat Surg.
2025 May;29(2):187-191. 10.14701/ahbps.24-217.
“Liver-loop”: A case report of an alternative modified liver hanging maneuver
- Affiliations
-
- 1HPB Surgery and Liver Transplantation Unit, Hospital de Alta Complejidad “El Cruce”, Buenos Aires, Argentina
- KMID: 2568267
- DOI: http://doi.org/10.14701/ahbps.24-217
Abstract
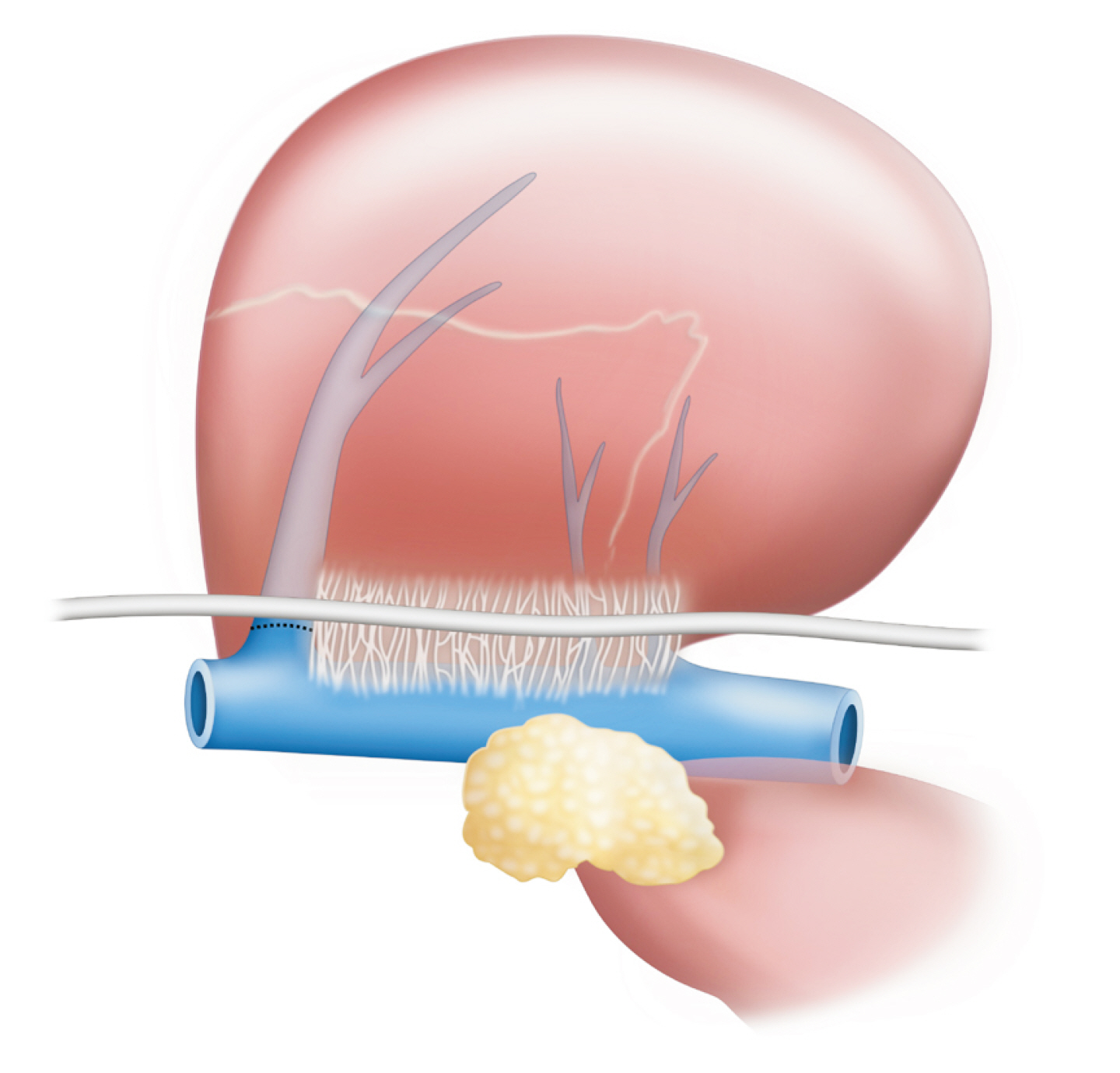
- The liver hanging maneuver (LHM), introduced by Belghiti et al. in 2001, has been widely adapted to various hepatectomy techniques to reduce blood loss and facilitate parenchymal transection. However, its primary limitation is the risk of vascular injury, particularly near the inferior vena cava (IVC). In this report, we describe a modified “Loop-Hanging” maneuver designed as an alternative to enhance exposure during parenchymal transection and improve the control of Glissonean pedicles. In this case, we employed the technique during an open right hemihepatectomy on a 47-year-old male patient with a complex bile duct injury following two unsuccessful Roux-en-Y hepaticojejunostomies (RYHJ). The patient was referred to our institution due to an RYHJ stricture. Imaging identified a right hepatic artery pseudoaneurysm and a fistula to the biliary limb. After two failed attempts at endovascular embolization, a surgical approach was determined through multidisciplinary discussions. During the surgery, the liver was looped with a nasogastric tube positioned anterior to the IVC, allowing gentle upward traction that facilitated the transection, minimized bleeding, and enhanced pedicle control. The LHM is known to reduce blood loss but carries risks for patients with anatomical variations, scarring, or cirrhosis. Our “Loop-Hanging” technique retains the core advantages of LHM, simplifies the process, and diminishes the risk of vascular injury. Further research is required to assess its safety and broader applicability.
Figure
Reference
-
References
1. Belghiti J, Guevara OA, Noun R, Saldinger PF, Kianmanesh R. 2001; Liver hanging maneuver: a safe approach to right hepatectomy without liver mobilization. J Am Coll Surg. 193:109–111. DOI: 10.1016/S1072-7515(01)00909-7. PMID: 11442247.
Article2. Ishii T, Iwaki K, Nakakura A, Uchida Y, Ito T, Hatano E. 2024; Is the anterior approach recommended for liver resection of hepatocellular carcinoma? A systematic review and meta-analysis. J Hepatobiliary Pancreat Sci. 31:133–142. DOI: 10.1002/jhbp.1393. PMID: 37984829.
Article3. Granieri S, Frassini S, Torre B, Bonomi A, Paleino S, Bruno F, et al. 2024; Anterior approach with or without liver hanging maneuver versus conventional approach in major liver resections. A systematic review and meta-analysis of randomized controlled trials. Eur J Surg Oncol. 50:108535. DOI: 10.1016/j.ejso.2024.108535. PMID: 39083883.
Article4. Rahbari NN, Birgin E, Bork U, Mehrabi A, Reißfelder C, Weitz J. 2021; Anterior approach vs conventional hepatectomy for resection of colorectal liver metastasis: a randomized clinical trial. JAMA Surg. 156:31–40. DOI: 10.1001/jamasurg.2020.5050. PMID: 33147332. PMCID: PMC7643041.
Article5. Li H, Zhu B, Huang J, Chen X, Wang J, Wu H. 2019; Liver hanging maneuver versus conventional approach for open hepatectomy: a meta-analysis. HPB (Oxford). 21:802–809. DOI: 10.1016/j.hpb.2018.09.019. PMID: 30606685.
Article6. Tzedakis S, Jeddou H, Boudjema K, Gaujoux S. 2020; Hanging and modified liver hanging maneuver. J Visc Surg. 157:511–518. DOI: 10.1016/j.jviscsurg.2020.08.008. PMID: 32912751.
Article7. Fleres F, Piardi T, Sommacale D. 2018; How to do: technique of liver hanging maneuver-step by step. J Vis Surg. 4:213. DOI: 10.21037/jovs.2018.09.16.
Article8. Liddo G, Buc E, Nagarajan G, Hidaka M, Dokmak S, Belghiti J. 2009; The liver hanging manoeuvre. HPB (Oxford). 11:296–305. DOI: 10.1111/j.1477-2574.2009.00068.x. PMID: 19718356. PMCID: PMC2727082.
Article9. Ogata S, Belghiti J, Varma D, Sommacale D, Maeda A, Dondero F, et al. Two hundred liver hanging maneuvers for major hepatectomy: a single-center experience. Ann Surg. 2007; 245:31–35. DOI: 10.1097/01.sla.0000224725.40979.0a. PMID: 17197962. PMCID: PMC1867932.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Technical Evolution in Living Donor Liver Transplantation
- Clinical Application of Hepatic Resection Using Glissonean Pedicle Transection Method and Hanging Maneuver
- Significance of liver hanging maneuver for anatomical hepatectomy in patients with a large hepatocellular carcinoma compressing intrahepatic vasculatures
- The Pringle maneuver in the modern era: A review of techniques for hepatic inflow occlusion in minimally invasive liver resection
- A Case of Malabsorption Induced by Blind Loop Syndrome in a Patient with Liver Cirrhosis