Cancer Res Treat.
2025 Apr;57(2):478-491. 10.4143/crt.2024.758.
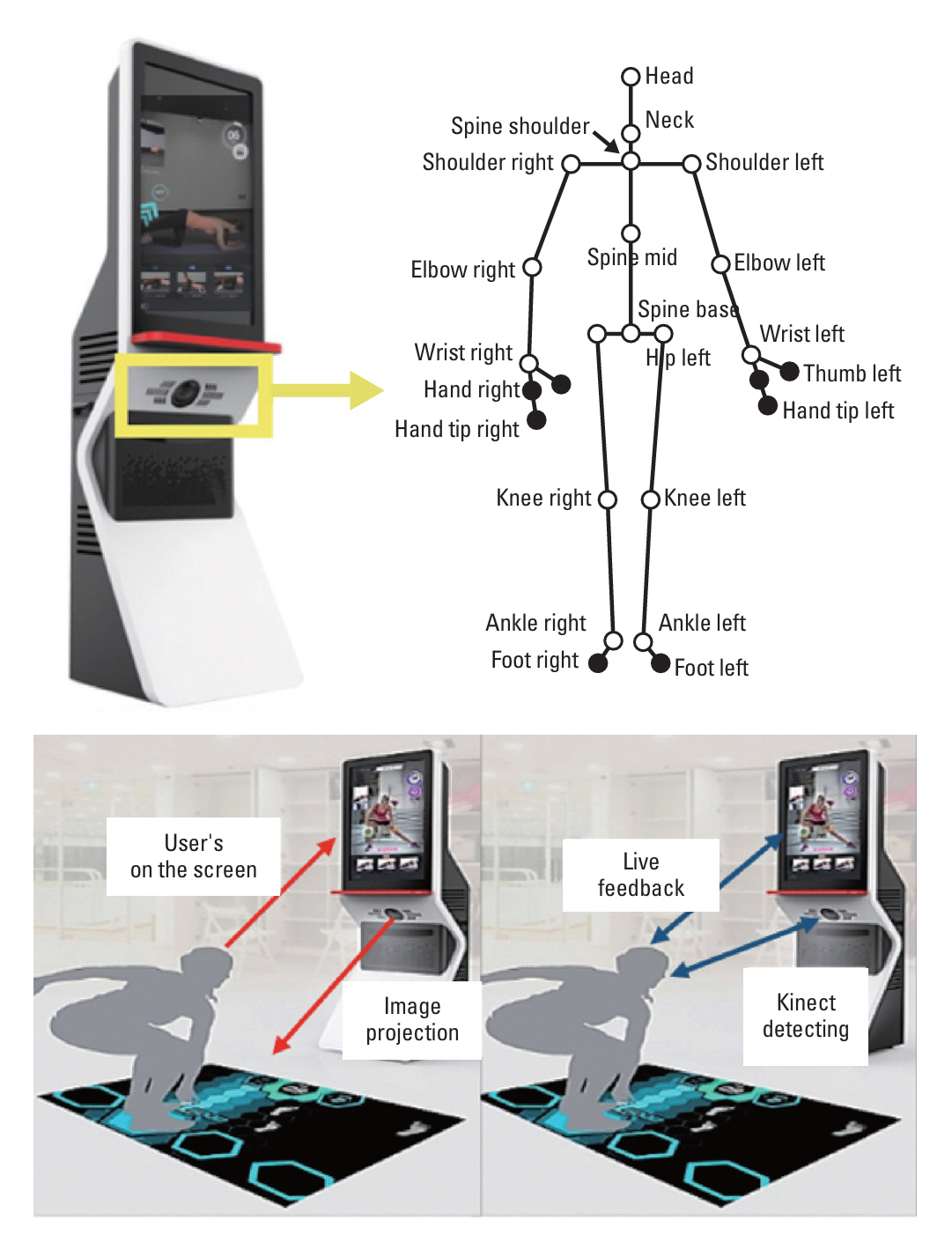
Kinect-Based Mixed Reality Exercise Program Improves Physical Function and Quality of Life in Breast Cancer Survivors: A Randomized Clinical Trial
- Affiliations
-
- 1Health and Exercise Science Laboratory, Department of Physical Education, Seoul National University, Seoul, Korea
- 2Institute on Aging, Seoul National University, Seoul, Korea
- 3Dr. Exsol, Inc., Research Institute, Seoul, Korea
- 4Institute of Sport Science, Seoul National University, Seoul, Korea
- KMID: 2566865
- DOI: http://doi.org/10.4143/crt.2024.758
Abstract
- Purpose
Exercise is an effective non-pharmacological approach for alleviating treatment-related adverse effects and enhancing physical fitness in breast cancer survivors. A Kinect-based mixed reality device (KMR), with real-time feedback and user data collection, is an innovative exercise intervention for breast cancer survivors. This study aimed to investigate the effect of KMR exercise program on quality of life (QOL) and physical function in breast cancer survivors.
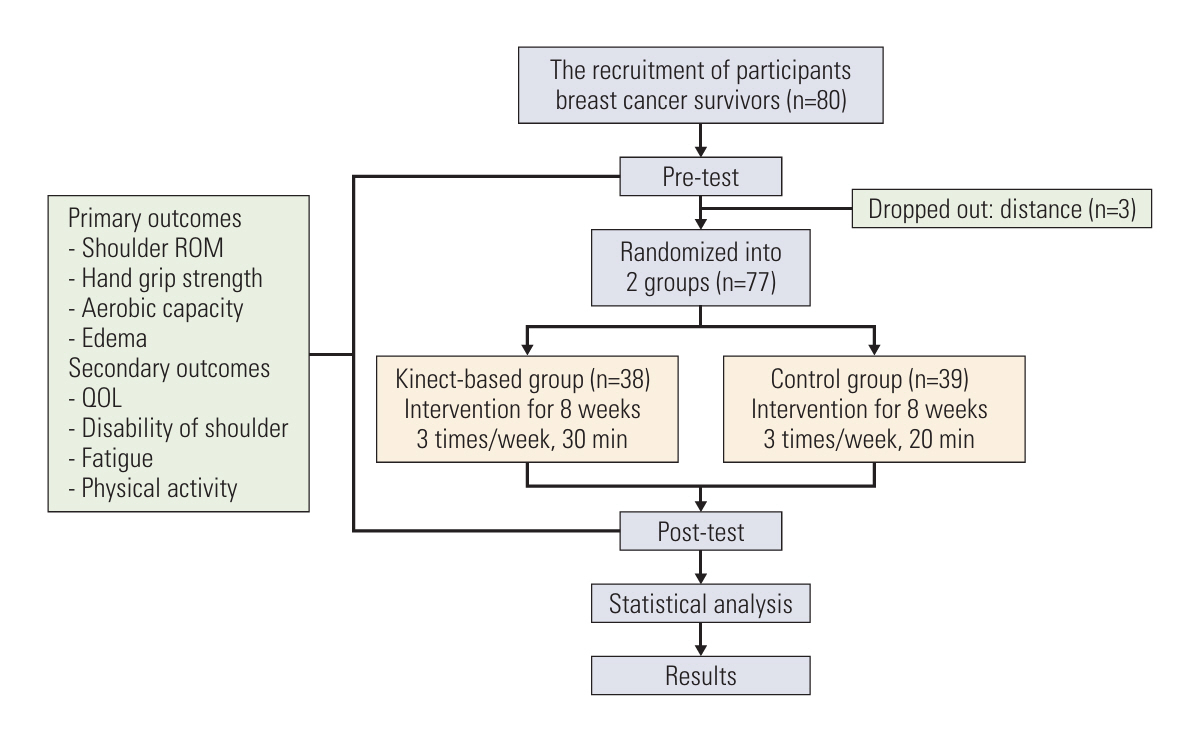
Materials and Methods
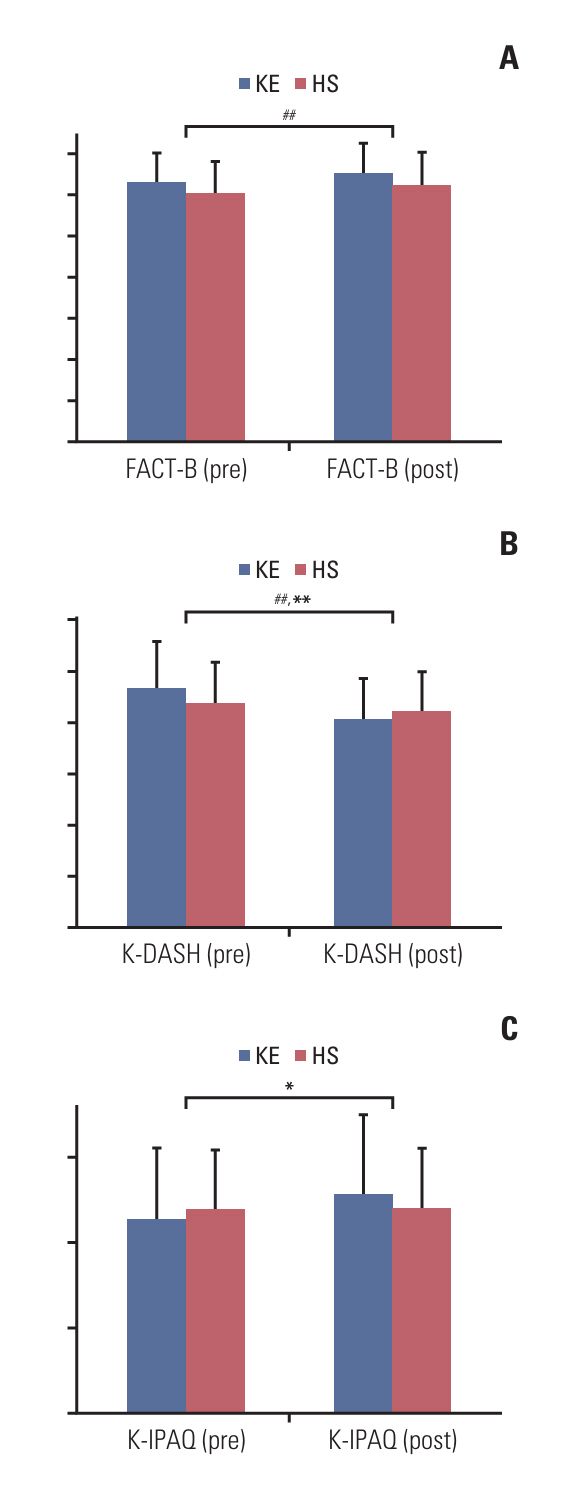
Seventy-seven participants were randomly assigned to either the KMR exercise group or home stretching group with an 8-week intervention. Physical function (shoulder range of motion, body composition, aerobic capacity, and hand grip strength) was evaluated before and after the intervention period. Participants completed questionnaires such as the Disabilities of the Arm, Shoulder, and Hand (DASH), Functional Assessment of Cancer Therapy-Breast, and International Physical Activity Questionnaire (IPAQ) to assess upper extremity disabilities, QOL, and physical activity levels.
Results
Significant group-by-time interaction was found for flexion of the operated arm (154.3±12.5 to 165.8±11.2), and the non-operated arm (158.2±13.8 to 166.5±12.2), abduction of the non-operated arm (154.8±31.6 to 161.1±28.1), and adduction of the operated arm (46.5±9.1 to 52.6±7.2). Significant improvements were also observed in DASH (46.8±9.1 to 40.8±9.3) and IPAQ (1,136.3±612.8 to 1,287±664.1).
Conclusion
The KMR exercise program effectively improved the physical function, alleviated edema, reduced upper extremity disability, and enhanced the QOL in breast cancer survivors. Coupled with significant group-by-time interactions for various outcomes, the results emphasize the potential benefits of incorporating the KMR exercise program to improve the QOL in breast cancer survivors.
Keyword
Figure
Reference
-
References
1. Siegel RL, Miller KD, Wagle NS, Jemal A. Cancer statistics, 2023. CA Cancer J Clin. 2023; 73:17–48.
Article2. Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021; 71:209–49.
Article3. Stout NL, Baima J, Swisher AK, Winters-Stone KM, Welsh J. A systematic review of exercise systematic reviews in the cancer literature (2005-2017). PM R. 2017; 9:S347–84.
Article4. Dieli-Conwright CM, Parmentier JH, Sami N, Lee K, Spicer D, Mack WJ, et al. Adipose tissue inflammation in breast cancer survivors: effects of a 16-week combined aerobic and resistance exercise training intervention. Breast Cancer Res Treat. 2018; 168:147–57.
Article5. Baumann FT, Reike A, Reimer V, Schumann M, Hallek M, Taaffe DR, et al. Effects of physical exercise on breast cancer-related secondary lymphedema: a systematic review. Breast Cancer Res Treat. 2018; 170:1–13.
Article6. Mijwel S, Backman M, Bolam KA, Jervaeus A, Sundberg CJ, Margolin S, et al. Adding high-intensity interval training to conventional training modalities: optimizing health-related outcomes during chemotherapy for breast cancer: the OptiTrain randomized controlled trial. Breast Cancer Res Treat. 2018; 168:79–93.
Article7. Panchik D, Masco S, Zinnikas P, Hillriegel B, Lauder T, Suttmann E, et al. Effect of exercise on breast cancer-related lymphedema: what the lymphatic surgeon needs to know. J Reconstr Microsurg. 2019; 35:37–45.
Article8. Knowlton SE, O’Donnell EK, Horick N, Perez GK, Park E, Rabin J, et al. Moving forward on all fronts: impact, patterns, and barriers to exercise in cancer survivors and patients living with advanced disease. Support Care Cancer. 2020; 28:4979–88.
Article9. Ng AH, Ngo-Huang A, Vidal M, Reyes-Garcia A, Liu DD, Williams JL, et al. Exercise barriers and adherence to recommendations in patients with cancer. JCO Oncol Pract. 2021; 17:e972–81.
Article10. Hardcastle SJ, Maxwell-Smith C, Kamarova S, Lamb S, Millar L, Cohen PA. Factors influencing non-participation in an exercise program and attitudes towards physical activity amongst cancer survivors. Support Care Cancer. 2018; 26:1289–95.
Article11. Yeon S, Jeong A, Min J, Byeon J, Yoon YJ, Heo J, et al. Tearing down the barriers to exercise after mastectomy: a qualitative inquiry to facilitate exercise among breast cancer survivors. BMJ Open. 2022; 12:e055157.
Article12. Fernandes CS, Baldaia C, Ferreira LM. Impact of exergames in women with breast cancer after surgery: a systematic review. SN Compr Clin Med. 2023; 5:5.
Article13. Basha MA, Aboelnour NH, Alsharidah AS, Kamel FH. Effect of exercise mode on physical function and quality of life in breast cancer-related lymphedema: a randomized trial. Support Care Cancer. 2022; 30:2101–10.
Article14. Feyzioglu O, Dincer S, Akan A, Algun ZC. Is Xbox 360 Kinect-based virtual reality training as effective as standard physiotherapy in patients undergoing breast cancer surgery? Support Care Cancer. 2020; 28:4295–303.
Article15. Winters L, Post K, Flanagan J. A web-streamed yoga intervention for breast cancer survivors. Creat Nurs. 2020; 26:e70–6.
Article16. Lim BG, Li X, Sung YH, Lee SW, Kim HJ, Song W. Effects of Kinect-based mixed reality device on physical function and quality of life in breast cancer survivors: a randomized controlled trial. J Korean Soc Integr Med. 2023; 11:49–60.17. Sietsema KE, Stringer WW, Sue DY, Ward SA. Wasserman & Whipp’s principles of exercise testing and interpretation. 6th ed. Lippincott Williams & Wilkins;2020.18. Lee JY, Lim JY, Oh JH, Ko YM. Cross-cultural adaptation and clinical evaluation of a Korean version of the disabilities of arm, shoulder, and hand outcome questionnaire (K-DASH). J Shoulder Elbow Surg. 2008; 17:570–4.
Article19. Chun MY. Validity and reliability of korean version of international physical activity questionnaire short form in the elderly. Korean J Fam Med. 2012; 33:144–51.
Article20. Kim H, Song KH, Ambegaonkar JP, Chung S, Jeon K, Jiang FL, et al. Two-megahertz impedance index prediction equation for appendicular lean mass in Korean older people. BMC Geriatr. 2022; 22:385.
Article21. Yasunaga Y, Kondoh S, Nakajima Y, Mimura S, Kobayashi M, Yuzuriha S, et al. Extracellular water ratio as an indicator of the development and severity of leg lymphedema using bioelectrical impedance analysis. Lymphat Res Biol. 2021; 19:223–30.
Article22. Cohen J. Statistical power analysis for the behavioral sciences. Academic Press;2013.23. Reis AD, Pereira P, Diniz RR, de Castro Filha JGL, Dos Santos AM, Ramallo BT, et al. Effect of exercise on pain and functional capacity in breast cancer patients. Health Qual Life Outcomes. 2018; 16:58.
Article24. Sagarra-Romero L, Butragueno J, Gomez-Bruton A, Lozano-Berges G, Vicente-Rodriguez G, Morales JS. Effects of an online home-based exercise intervention on breast cancer survivors during COVID-19 lockdown: a feasibility study. Support Care Cancer. 2022; 30:6287–97.
Article25. Friedenreich CM, Stone CR, Cheung WY, Hayes SC. Physical activity and mortality in cancer survivors: a systematic review and meta-analysis. JNCI Cancer Spectr. 2020; 4:pkz080.
Article26. Aydin M, Kose E, Odabas I, Meric Bingul B, Demirci D, Aydin Z. The effect of exercise on life quality and depression levels of breast cancer patients. Asian Pac J Cancer Prev. 2021; 22:725–32.
Article27. Lang AE, Dickerson CR, Kim SY, Stobart J, Milosavljevic S. Impingement pain affects kinematics of breast cancer survivors in work-related functional tasks. Clin Biomech (Bristol, Avon). 2019; 70:223–30.
Article28. Fisher MI, Capilouto G, Malone T, Bush H, Uhl TL. Comparison of upper extremity function in women with and women without a history of breast cancer. Phys Ther. 2020; 100:500–8.
Article29. De Groef A, Van Kampen M, Dieltjens E, Christiaens MR, Neven P, Geraerts I, Devoogdt N. Effectiveness of postoperative physical therapy for upper-limb impairments after breast cancer treatment: a systematic review. Arch Phys Med Rehabil. 2015; 96:1140–53.
Article30. Galantino ML, Stout NL. Exercise interventions for upper limb dysfunction due to breast cancer treatment. Phys Ther. 2013; 93:1291–7.
Article31. da Silva Alves R, de Carvalho JM, Borges JBC, Nogueira DA, Iunes DH, Carvalho LC. Effect of exergaming on quality of life, fatigue, and strength and endurance muscle in cancer patients: a randomized crossover trial. Games Health J. 2023; 12:358–65.
Article32. Chirico A, Maiorano P, Indovina P, Milanese C, Giordano GG, Alivernini F, et al. Virtual reality and music therapy as distraction interventions to alleviate anxiety and improve mood states in breast cancer patients during chemotherapy. J Cell Physiol. 2020; 235:5353–62.
Article33. Bani Mohammad E, Ahmad M. Virtual reality as a distraction technique for pain and anxiety among patients with breast cancer: a randomized control trial. Palliat Support Care. 2019; 17:29–34.
Article34. van der Kruk SR, Zielinski R, MacDougall H, Hughes-Barton D, Gunn KM. Virtual reality as a patient education tool in healthcare: a scoping review. Patient Educ Couns. 2022; 105:1928–42.
Article35. Lee K, Kang I, Mack WJ, Mortimer J, Sattler F, Salem G, et al. Feasibility of high intensity interval training in patients with breast cancer undergoing anthracycline chemotherapy: a randomized pilot trial. BMC Cancer. 2019; 19:653.
Article36. Frydenberg H, Bettum TJ, Lofterød T, Edvardsen E, Flote VG, Finstad SE, et al. Abstract P6-08-37: cardiorespiratory fitness (VO2max) before, during and after adjuvant treatment in breast cancer patients. Cancer Res. 2015; 75(9 Suppl):P6-08-37.
Article37. Fukushima T, Nakano J, Hashizume K, Ueno K, Matsuura E, Ikio Y, et al. Effects of aerobic, resistance, and mixed exercises on quality of life in patients with cancer: a systematic review and meta-analysis. Complement Ther Clin Pract. 2021; 42:101290.
Article38. Odynets T, Briskin Y, Todorova V. Effects of different exercise interventions on quality of life in breast cancer patients: a randomized controlled trial. Integr Cancer Ther. 2019; 18:1534735419880598.
Article39. Roine E, Sintonen H, Kellokumpu-Lehtinen PL, Penttinen H, Utriainen M, Vehmanen L, et al. Health-related quality of life of breast cancer survivors attending an exercise intervention study: a five-year follow-up. In Vivo. 2020; 34:667–74.
Article40. Piraux E, Caty G, Aboubakar Nana F, Reychler G. Effects of exercise therapy in cancer patients undergoing radiotherapy treatment: a narrative review. SAGE Open Med. 2020; 8:2050312120922657.
Article41. Schumacher O, Luo H, Taaffe DR, Galvao DA, Tang C, Chee R, et al. Effects of exercise during radiation therapy on physical function and treatment-related side effects in men with prostate cancer: a systematic review and meta-analysis. Int J Radiat Oncol Biol Phys. 2021; 111:716–31.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Development and Evaluation of an App-Based Self-Management Program for Exercise Practice of Breast Cancer Survivors: A Non-Randomized Controlled Trial
- Effect of Applying Exercise Movement Technique by Physical Therapist on Quality of Life in Breast Cancer Survivors: Meta-analysis
- Effects of an Exercise Program on Physical Functions and Quality of Life for Mastectomy Patients
- Effects of Self-Lymph Massage Method among Breast Cancer Survivors
- Effects of a 4-Week Multimodal Rehabilitation Program on Quality of Life, Cardiopulmonary Function, and Fatigue in Breast Cancer Patients