J Korean Neurosurg Soc.
2025 Mar;68(2):177-183. 10.3340/jkns.2024.0157.
Early Adequate Nutrition in ICU Is Associated with Survival Gain : Retrospective Cohort Study in Patient with Traumatic Brain Injury
- Affiliations
-
- 1Department of Pharmacy, Uijeongbu St. Mary’s Hospital, Uijeongbu, Korea
- 2Nutrition Team, Uijeongbu St. Mary’s Hospital, Uijeongbu, Korea
- 3Department of Neurosurgery, Uijeongbu St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 4Department of Surgery, Uijeongbu St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 5Department of Trauma Surgery, Uijeongbu St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- KMID: 2565275
- DOI: http://doi.org/10.3340/jkns.2024.0157
Abstract
Objective
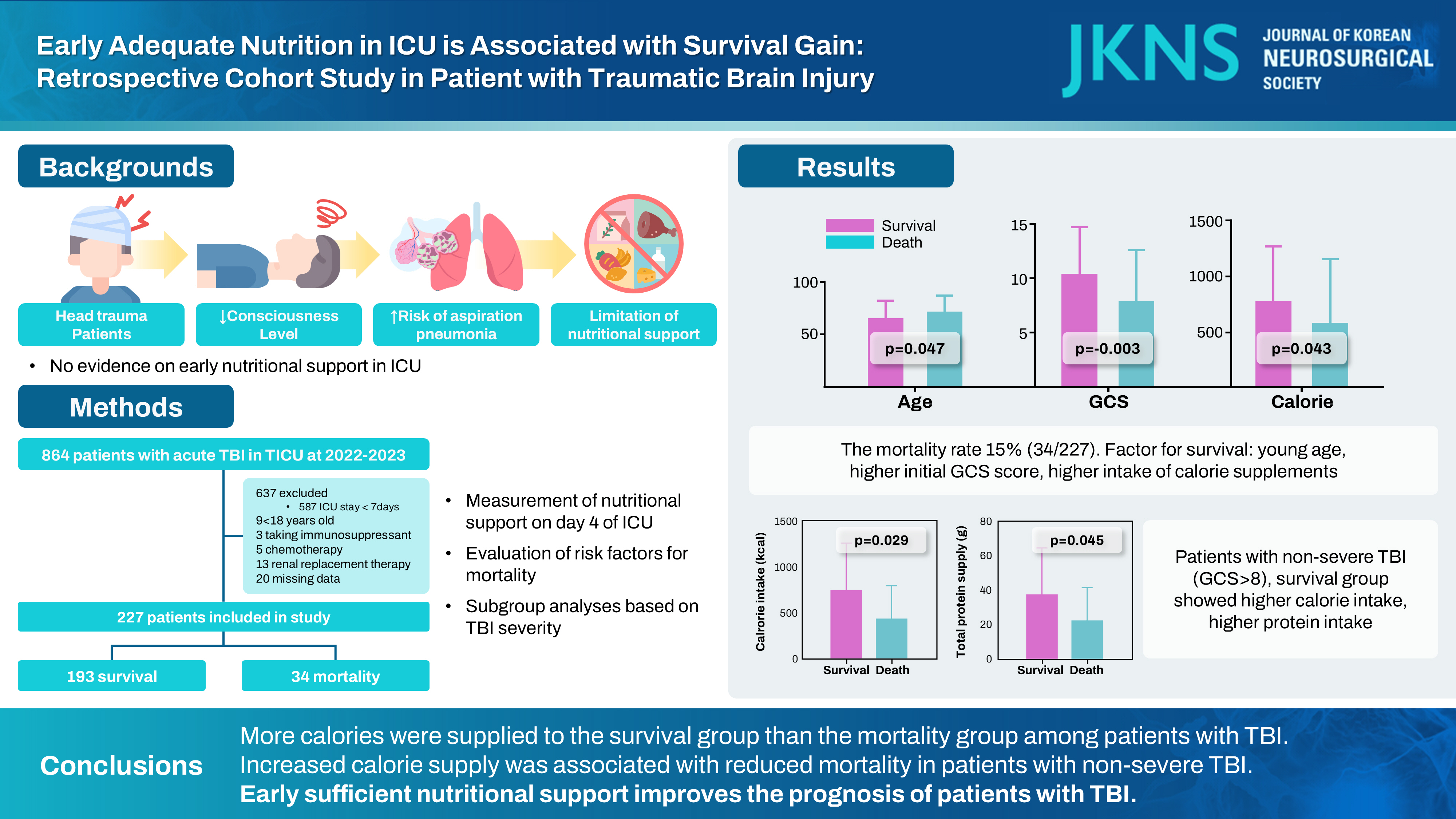
: Patients with traumatic brain injury (TBI) commonly exhibit a poor mental health status and can easily develop aspiration pneumonia. Thus, early proper nutrition through oral or tube feeding is difficult to achieve, leading to malnutrition. However, evidence regarding early nutritional support in the intensive care unit (ICU) is lacking. We aimed to assess the effect of early nutrition in patients with TBI admitted to the ICU.
Methods
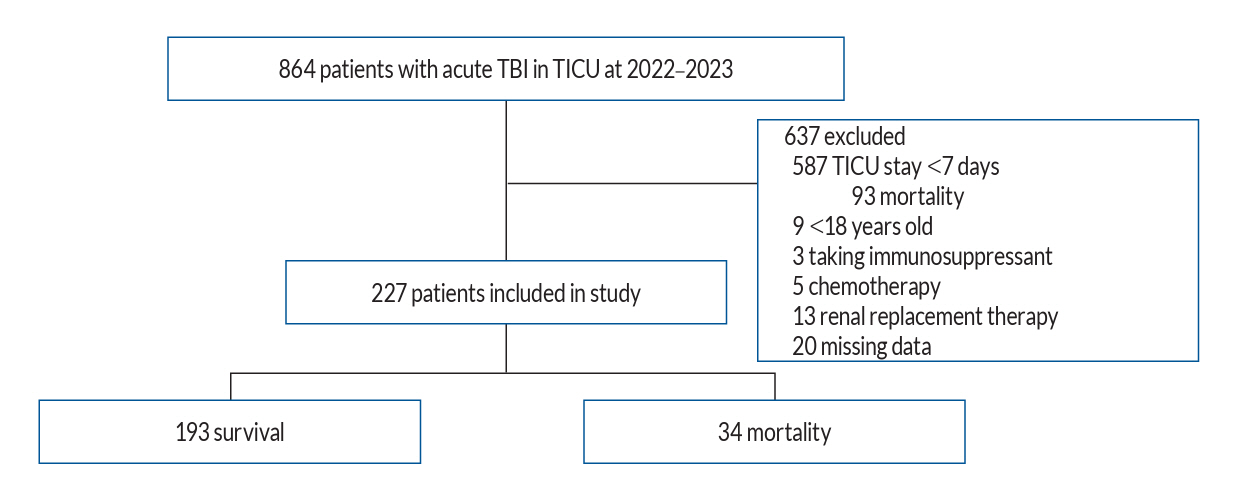
: Data of adult patients with TBI admitted to the trauma ICU of a regional trauma center in Korea between 2022 and 2023 were retrospectively analyzed. Those with ICU stay <7 days, younger than 18 years, and with underlying diseases that could alter baseline metabolism, were excluded. Nutritional support on day 4 of ICU admission was measured. The patients were classified into mortality and survival groups, and risk factors for mortality were evaluated. Subgroup analyses were performed based on TBI severity.
Results
: Overall, 864 patients were diagnosed with acute TBI, of whom 227 were included in this study. The mortality rate in the study population was 15% (n=34). Those in the survival group were younger, had longer hospital stays, had a higher initial Glasglow coma scale (GCS) score, and had a higher intake of calorie supplements than those in the mortality group. In a subgroup analysis of patients with non-severe TBI (GCS >8), total calorie intake (751.4 vs. 434.2 kcal, p=0.029), total protein intake (37.5 vs. 22.1 g, p=0.045), and ratio of supplied to target calories (0.49 vs. 0.30, p=0.047) were higher in the survival group than in the mortality group. Logistic regression analysis revealed that calorie intake (B=-0.002, p=0.040) and initial hemoglobin level (B=-0.394, p=0.005) were risk factors for mortality in patients with non-severe TBI.
Conclusion
: More calories were supplied to the survival group than the mortality group among patients with TBI. Additionally, logistic regression analysis showed that increased calorie supply was associated with reduced mortality in patients with non-severe TBI. The mortality group had low protein intake; however, this did not emerge as a risk factor for mortality. Early sufficient nutritional support improves the prognosis of patients with TBI.
Figure
Cited by 1 articles
-
Editors’ Pick in March 2025
Hee-Jin Yang
J Korean Neurosurg Soc. 2025;68(2):111-112. doi: 10.3340/jkns.2025.0046.
Reference
-
References
1. Compher C, Bingham AL, McCall M, Patel J, Rice TW, Braunschweig C, et al. Guidelines for the provision of nutrition support therapy in the adult critically ill patient: the American Society for Parenteral and Enteral Nutrition. JPEN J Parenter Enteral Nutr. 46:12–41. 2022.
Article2. Fan M, Wang Q, Fang W, Jiang Y, Li L, Sun P, et al. Early enteral combined with parenteral nutrition treatment for severe traumatic brain injury: effects on immune function, nutritional status and outcomes. Chin Med Sci J. 31:213–220. 2016.
Article3. Ganesh S, Ibrahim NA. Nutrition therapy in critically ill patients with traumatic brain injury. Hum Nutr Metab. 34:200219. 2023.
Article4. Goiburu ME, Goiburu MM, Bianco H, Díaz JR, Alderete F, Palacios MC, et al. The impact of malnutrition on morbidity, mortality and length of hospital stay in trauma patients. Nutr Hosp. 21:604–610. 2006.5. Gunst M, Ghaemmaghami V, Gruszecki A, Urban J, Frankel H, Shafi S. Changing epidemiology of trauma deaths leads to a bimodal distribution. Proc (Bayl Univ Med Cent). 23:349–354. 2010.
Article6. Heo GJ, Lee J, Choi WS, Hyun SY, Cho JS. Analysis of aspiration risk factors in severe trauma patients: based on findings of aspiration lung disease in chest computed tomography. J Trauma Inj. 33:88–95. 2020.
Article7. Jakob DA, Lewis M, Benjamin ER, Demetriades D. Isolated traumatic brain injury: routine intubation for glasgow coma scale 7 or 8 may be harmful! J Trauma Acute Care Surg. 90:874–879. 2021.
Article8. Jeong DH, Hong SB, Lim CM, Koh Y, Seo J, Kim Y, et al. Relationship between nutrition intake and 28-day mortality using modified NUTRIC score in patients with sepsis. Nutrients. 11:1906. 2019.
Article9. Kim J, Shim Y, Choo YH, Kim HS, Kim YR, Ha EJ. Protein requirement changes according to the treatment application in neurocritical patients. J Korean Neurosurg Soc. 67:451–457. 2024.
Article10. Kompan L, Vidmar G, Spindler-Vesel A, Pecar J. Is early enteral nutrition a risk factor for gastric intolerance and pneumonia? Clin Nutr. 23:527–532. 2004.
Article11. Krakau K, Omne-Pontén M, Karlsson T, Borg J. Metabolism and nutrition in patients with moderate and severe traumatic brain injury: a systematic review. Brain Inj. 20:345–367. 2006.
Article12. Kwon J, Lee M, Kim Y, Moon J, Huh Y, Song S, et al. Trauma system establishment and outcome improvement: a retrospective national cohort study in South Korea. Int J Surg. 109:2293–2302. 2023.
Article13. Li Y, Liu C, Xiao W, Song T, Wang S. Incidence, risk factors, and outcomes of ventilator-associated pneumonia in traumatic brain injury: a meta-analysis. Neurocrit Care. 32:272–285. 2020.
Article14. Lin J, Chen W, Ye X, Lv C, Liu Y, Jiang X, et al. Trajectories of protein intake and 28-day mortality in critically ill patients: a secondary analysis of a cluster-randomized controlled trial. Clin Nutr. 41:1644–1650. 2022.
Article15. Luo HC, Fu YQ, You CY, Liu CJ, Xu F. Comparison of admission serum albumin and hemoglobin as predictors of outcome in children with moderate to severe traumatic brain injury: a retrospective study. Medicine (Baltimore). 98:e17806. 2019.16. Lv C, Jiang X, Long Y, Liu Z, Lin J, Wu C, et al. Association between caloric adequacy and short-term clinical outcomes in critically ill patients using a weight-based equation: secondary analysis of a cluster-randomized controlled trial. Front Nutr. 9:902986. 2022.
Article17. Maurer E, Wallmeier V, Reumann MK, Ehnert S, Ihle C, Schreiner AJ, et al. Risk of malnutrition in orthopedic trauma patients with surgical site infections is associated with increased morbidity and mortality - a 3-year follow-up study. Injury. 51:2219–2229. 2020.
Article18. Oh SY, Lee JM, Lee HY, Kwon J, Lee HJ, Choi NJ, et al. The status of protein supply to patients in the trauma and surgical intensive care units and the effects of feedback on protein supply: a multicenter study. J Acute Care Surg. 12:132–137. 2022.
Article19. Onuk S, Ozer NT, Savas N, Sipahioglu H, Temel S, Ergul SS, et al. Enteral nutrition interruptions in critically ill patients: a prospective study on reasons, frequency and duration of interruptions of nutritional support during ICU stay. Clin Nutr ESPEN. 52:178–183. 2022.
Article20. Quintard H, Ichai C. Nutritional and metabolic supplementation for the injured brain: an update. Curr Opin Crit Care. 25:126–131. 2019.
Article21. Singer P, Blaser AR, Berger MM, Calder PC, Casaer M, Hiesmayr M, et al. ESPEN practical and partially revised guideline: clinical nutrition in the intensive care unit. Clin Nutr. 42:1671–1689. 2023.
Article22. Turnagöl HH, Koşar ŞN, Güzel Y, Aktitiz S, Atakan MM. Nutritional considerations for injury prevention and recovery in combat sports. Nutrients. 14:53. 2021.
Article23. van Zanten ARH, De Waele E, Wischmeyer PE. Nutrition therapy and critical illness: practical guidance for the ICU, post-ICU, and long-term convalescence phases. Crit Care. 23:368. 2019.
Article24. Wang X, Yu Z, Zhou S, Shen S, Chen W. The effect of a compound protein on wound healing and nutritional status. Evid Based Complement Alternat Med. 2022:4231516. 2022.
Article25. Weijs PJM, Mogensen KM, Rawn JD, Christopher KB. Protein intake, nutritional status and outcomes in ICU survivors: a single center cohort study. J Clin Med. 8:43. 2019.
Article26. Zusman O, Theilla M, Cohen J, Kagan I, Bendavid I, Singer P. Resting energy expenditure, calorie and protein consumption in critically ill patients: a retrospective cohort study. Crit Care. 20:367. 2016.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Relationship of the Facial Injury Location and the Traumatic Brain Hemorrhage
- Investigation of the Cause of Readmission to the Intensive Care Unit for Patients with Lung Edema or Atelectasis
- Nutrition Therapy for Patients With Traumatic Brain Injury: A Narrative Review
- Early and Late Tracheostomy after Decompressive Craniectomy for Severe Traumatic Brain Injury
- Traumatic Brain injury and Sleep Disorder