Kosin Med J.
2024 Dec;39(4):229-237. 10.7180/kmj.24.140.
The ethics of using artificial intelligence in medical research
- Affiliations
-
- 1Department of Laboratory Medicine, Inje University Haeundae Paik Hospital, Busan, Korea
- 2Department of Psychiatry, Kosin University Gospel Hospital, Kosin University College of Medicine, Busan, Korea
- 3Department of Laboratory Medicine, Kosin University Gospel Hospital, Kosin University College of Medicine, Busan, Korea
- KMID: 2562805
- DOI: http://doi.org/10.7180/kmj.24.140
Abstract
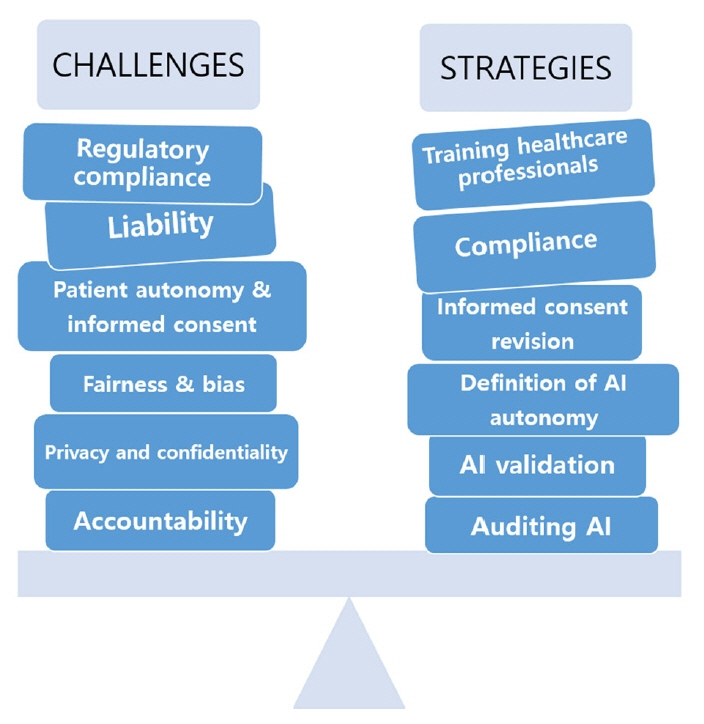
- The integration of artificial intelligence (AI) technologies into medical research introduces significant ethical challenges that necessitate the strengthening of ethical frameworks. This review highlights the issues of privacy, bias, accountability, informed consent, and regulatory compliance as central concerns. AI systems, particularly in medical research, may compromise patient data privacy, perpetuate biases if they are trained on nondiverse datasets, and obscure accountability owing to their “black box” nature. Furthermore, the complexity of the role of AI may affect patients’ informed consent, as they may not fully grasp the extent of AI involvement in their care. Compliance with regulations such as the Health Insurance Portability and Accountability Act and General Data Protection Regulation is essential, as they address liability in cases of AI errors. This review advocates a balanced approach to AI autonomy in clinical decisions, the rigorous validation of AI systems, ongoing monitoring, and robust data governance. Engaging diverse stakeholders is crucial for aligning AI development with ethical norms and addressing practical clinical needs. Ultimately, the proactive management of AI’s ethical implications is vital to ensure that its integration into healthcare improves patient outcomes without compromising ethical integrity.
Figure
Reference
-
References
1. Goirand M, Austin E, Clay-Williams R. Implementing ethics in healthcare AI-based applications: a scoping review. Sci Eng Ethics. 2021; 27:61.
Article2. Peterson M. The ethics of technology: response to critics. Sci Eng Ethics. 2018; 24:1645–52.
Article3. Rahimi F, Talebi Bezmin Abadi A. ChatGPT and publication ethics. Arch Med Res. 2023; 54:272–4.
Article4. Dave T, Athaluri SA, Singh S. ChatGPT in medicine: an overview of its applications, advantages, limitations, future prospects, and ethical considerations. Front Artif Intell. 2023; 6:1169595.
Article5. Kunstadter P. Medical ethics in cross-cultural and multi-cultural perspectives. Soc Sci Med Med Anthropol. 1980; 14B:289–96.
Article6. DeWane M, Grant-Kels JM. The ethics of volunteerism: whose cultural and ethical norms take precedence? J Am Acad Dermatol. 2018; 78:426–8.
Article7. Martinsons MG, Ma D. Sub-cultural differences in information ethics across China: focus on Chinese management generation gaps. J Assoc Inf Syst. 2009; 10:816–33.
Article8. Ess C. Ethical pluralism and global information ethics. Ethics Inf Technol. 2006; 8:215–26.
Article9. Yuan S, Li F, Browning MH, Bardhan M, Zhang K, McAnirlin O, et al. Leveraging and exercising caution with ChatGPT and other generative artificial intelligence tools in environmental psychology research. Front Psychol. 2024; 15:1295275.
Article10. Stenseke J. Interdisciplinary confusion and resolution in the context of moral machines. Sci Eng Ethics. 2022; 28:24.
Article11. Kazim E, Koshiyama AS. A high-level overview of AI ethics. Patterns (N Y). 2021; 2:100314.
Article12. Elendu C, Amaechi DC, Elendu TC, Jingwa KA, Okoye OK, John Okah M, et al. Ethical implications of AI and robotics in healthcare: a review. Medicine (Baltimore). 2023; 102:e36671.
Article13. Alhammad N, Alajlani M, Abd-Alrazaq A, Epiphaniou G, Arvanitis T. Patients’ perspectives on the data confidentiality, privacy, and security of mHealth apps: systematic review. J Med Internet Res. 2024; 26:e50715.
Article14. Stanfill MH, Marc DT. Health information management: implications of artificial intelligence on healthcare data and information management. Yearb Med Inform. 2019; 28:56–64.
Article15. Wang C, Liu S, Yang H, Guo J, Wu Y, Liu J. Ethical considerations of using ChatGPT in health care. J Med Internet Res. 2023; 25:e48009.
Article16. Jeyaraman M, Balaji S, Jeyaraman N, Yadav S. Unraveling the ethical enigma: artificial intelligence in healthcare. Cureus. 2023; 15:e43262.
Article17. Diaz-Rodriguez N, Del Ser J, Coeckelbergh M, de Prado ML, Herrera-Viedma E, Herrera F. Connecting the dots in trustworthy artificial intelligence: from AI principles, ethics, and key requirements to responsible AI systems and regulation. Inf Fusion. 2023; 99:101896.18. Chan B. Black-box assisted medical decisions: AI power vs. ethical physician care. Med Health Care Philos. 2023; 26:285–92.
Article19. Marcus E, Teuwen J. Artificial intelligence and explanation: how, why, and when to explain black boxes. Eur J Radiol. 2024; 173:111393.
Article20. Amann J, Blasimme A, Vayena E, Frey D, Madai VI; Precise4Q consortium. Explainability for artificial intelligence in healthcare: a multidisciplinary perspective. BMC Med Inform Decis Mak. 2020; 20:310.
Article21. Karim MR, Islam T, Shajalal M, Beyan O, Lange C, Cochez M, et al. Explainable AI for bioinformatics: methods, tools and applications. Brief Bioinform. 2023; 24:bbad236.
Article22. Plass M, Kargl M, Kiehl TR, Regitnig P, Geibler C, Evans T, et al. Explainability and causability in digital pathology. J Pathol Clin Res. 2023; 9:251–60.
Article23. Allareddy V, Oubaidin M, Rampa S, Venugopalan SR, Elnagar MH, Yadav S, et al. Call for algorithmic fairness to mitigate amplification of racial biases in artificial intelligence models used in orthodontics and craniofacial health. Orthod Craniofac Res. 2023; 26 Suppl 1:124–30.
Article24. Saint James Aquino Y. Making decisions: bias in artificial intelligence and data‑driven diagnostic tools. Aust J Gen Pract. 2023; 52:439–42.
Article25. Vicente L, Matute H. Humans inherit artificial intelligence biases. Sci Rep. 2023; 13:15737.
Article26. Sprung CL, Winick BJ. Informed consent in theory and practice: legal and medical perspectives on the informed consent doctrine and a proposed reconceptualization. Crit Care Med. 1989; 17:1346–54.27. Wang Y, Ma Z. Ethical and legal challenges of medical AI on informed consent: China as an example. Dev World Bioeth. 2024; Jan. 19. [Epub]. https://doi.org/10.1111/dewb.12442.
Article28. Neri E, Coppola F, Miele V, Bibbolino C, Grassi R. Artificial intelligence: who is responsible for the diagnosis? Radiol Med. 2020; 125:517–21.
Article29. Parchmann N, Hansen D, Orzechowski M, Steger F. An ethical assessment of professional opinions on concerns, chances, and limitations of the implementation of an artificial intelligence-based technology into the geriatric patient treatment and continuity of care. Geroscience. 2024; 46:6269–82.
Article30. Panesar SS, Kliot M, Parrish R, Fernandez-Miranda J, Cagle Y, Britz GW. Promises and perils of artificial intelligence in neurosurgery. Neurosurgery. 2020; 87:33–44.
Article31. Bi WL, Hosny A, Schabath MB, Giger ML, Birkbak NJ, Mehrtash A, et al. Artificial intelligence in cancer imaging: clinical challenges and applications. CA Cancer J Clin. 2019; 69:127–57.
Article32. Choudhury A, Chaudhry Z. Large language models and user trust: consequence of self-referential learning loop and the deskilling of health care professionals. J Med Internet Res. 2024; 26:e56764.
Article33. Bottomley D, Thaldar D. Liability for harm caused by AI in healthcare: an overview of the core legal concepts. Front Pharmacol. 2023; 14:1297353.
Article34. Nolan P, Matulionyte R. Artificial intelligence in medicine: issues when determining negligence. J Law Med. 2023; 30:593–615.
Article35. Haftenberger A, Dierks C. Legal integration of artificial intelligence into internal medicine: data protection, regulatory, reimbursement and liability questions. Inn Med (Heidelb). 2023; 64:1044–50.36. Terranova C, Cestonaro C, Fava L, Cinquetti A. AI and professional liability assessment in healthcare: a revolution in legal medicine? Front Med (Lausanne). 2024; 10:1337335.
Article37. Shumway DO, Hartman HJ. Medical malpractice liability in large language model artificial intelligence: legal review and policy recommendations. J Osteopath Med. 2024; 124:287–90.
Article38. Mu’azzam K, Santos da Silva FV, Murtagh J, Sousa Gallagher MJ. A roadmap for model-based bioprocess development. Biotechnol Adv. 2024; 73:108378.39. Ross J, Hammouche S, Chen Y, Rockall AG; Royal College of Radiologists AI Working Group. Beyond regulatory compliance: evaluating radiology artificial intelligence applications in deployment. Clin Radiol. 2024; 79:338–45.
Article40. Rezaeikhonakdar D. AI chatbots and challenges of HIPAA compliance for AI developers and vendors. J Law Med Ethics. 2023; 51:988–95.
Article41. Siebelmann B, Grass G, Matthaei M, Cursiefen C, Gerhardt T, Koeberlein-Neu J, et al. Implementation and execution of big data-based studies in ophthalmology within the framework of the GDPR. Klin Monbl Augenheilkd. 2024; 241:758–67.42. van Kolfschooten HB. A health-conformant reading of the GDPR’s right not to be subject to automated decision-making. Med Law Rev. 2024; 32:373–91.
Article43. Kumar K, Kumar P, Deb D, Unguresan ML, Muresan V. Artificial intelligence and machine learning based intervention in medical infrastructure: a review and future trends. Healthcare (Basel). 2023; 11:207.
Article44. Sharif T, Bugo J. The anthropological approach challenges the conventional approach to bioethical dilemmas: a Kenyan Maasai perspective. Afr Health Sci. 2015; 15:628–33.
Article45. Orfali K. Parental role in medical decision-making: fact or fiction? A comparative study of ethical dilemmas in French and American neonatal intensive care units. Soc Sci Med. 2004; 58:2009–22.
Article46. Orfali K, Gordon EJ. Autonomy gone awry: a cross-cultural study of parents’ experiences in neonatal intensive care units. Theor Med Bioeth. 2004; 25:329–65.
Article47. Nie JB, Smith KL, Cong Y, Hu L, Tucker JD. Medical professionalism in China and the United States: a transcultural interpretation. J Clin Ethics. 2015; 26:48–60.
Article48. Yasin L, Stapleton GR, Sandlow LJ. Medical professionalism across cultures: a literature review. MedEdPublish (2016). 2019; 8:191.
Article49. Rieder TN, Hutler B, Mathews DJ. Artificial intelligence in service of human needs: pragmatic first steps toward an ethics for semi-autonomous agents. AJOB Neurosci. 2020; 11:120–7.
Article50. Laitinen A, Sahlgren O. AI systems and respect for human autonomy. Front Artif Intell. 2021; 4:705164.
Article51. Vasey B, Lippert KA, Khan DZ, Ibrahim M, Koh CH, Layard Horsfall H, et al. Intraoperative applications of artificial intelligence in robotic surgery: a scoping review of current development stages and levels of autonomy. Ann Surg. 2023; 278:896–903.
Article52. Youssef A, Abramoff M, Char D. Is the algorithm good in a bad world, or has it learned to be bad? The ethical challenges of “locked” versus “continuously learning” and “autonomous” versus “assistive” AI tools in healthcare. Am J Bioeth. 2023; 23:43–5.
Article53. Talyshinskii A, Naik N, Hameed BM, Juliebo-Jones P, Somani BK. Potential of AI-driven chatbots in urology: revolutionizing patient care through artificial intelligence. Curr Urol Rep. 2024; 25:9–18.
Article54. Kerasidou A. Artificial intelligence and the ongoing need for empathy, compassion and trust in healthcare. Bull World Health Organ. 2020; 98:245–50.
Article55. Perry A. AI will never convey the essence of human empathy. Nat Hum Behav. 2023; 7:1808–9.
Article56. Magrabi F, Ammenwerth E, McNair JB, De Keizer NF, Hypponen H, Nykanen P, et al. Artificial intelligence in clinical decision support: challenges for evaluating AI and practical implications. Yearb Med Inform. 2019; 28:128–34.
Article57. Reddy S, Rogers W, Makinen VP, Coiera E, Brown P, Wenzel M, et al. Evaluation framework to guide implementation of AI systems into healthcare settings. BMJ Health Care Inform. 2021; 28:e100444.
Article58. Allen B, Dreyer K, Stibolt R Jr, Agarwal S, Coombs L, Treml C, et al. Evaluation and real-world performance monitoring of artificial intelligence models in clinical practice: try it, buy it, check it. J Am Coll Radiol. 2021; 18:1489–96.
Article59. Feng J, Phillips RV, Malenica I, Bishara A, Hubbard AE, Celi LA, et al. Clinical artificial intelligence quality improvement: towards continual monitoring and updating of AI algorithms in healthcare. NPJ Digit Med. 2022; 5:66.
Article60. Myllyaho L, Raatikainen M, Mannisto T, Mikkonen T, Nurminen JK. Systematic literature review of validation methods for AI systems. J Syst Softw. 2021; 181:111050.
Article61. Mokander J. Auditing of AI: legal, ethical and technical approaches. Digit Soc. 2023; 2:49.62. Reddy S. Generative AI in healthcare: an implementation science informed translational path on application, integration and governance. Implement Sci. 2024; 19:27.
Article63. Lysaght T, Lim HY, Xafis V, Ngiam KY. AI-assisted decision-making in healthcare: the application of an ethics framework for big data in health and research. Asian Bioeth Rev. 2019; 11:299–314.64. Kotsenas AL, Balthazar P, Andrews D, Geis JR, Cook TS. Rethinking patient consent in the era of artificial intelligence and big data. J Am Coll Radiol. 2021; 18(1 Pt B):180–4.
Article65. Jobin A, Ienca M, Vayena E. The global landscape of AI ethics guidelines. Nat Mach Intell. 2019; 1:389–99.
Article66. Rueda J, Rodriguez JD, Jounou IP, Hortal-Carmona J, Ausin T, Rodriguez-Arias D. “Just” accuracy? Procedural fairness demands explainability in AI-based medical resource allocations. AI Soc. 2024; 39:1141–22.
Article67. Kiseleva A, Kotzinos D, De Hert P. Transparency of AI in healthcare as a multilayered system of accountabilities: between legal requirements and technical limitations. Front Artif Intell. 2022; 5:879603.
Article68. Lomis K, Jeffries P, Palatta A, Sage M, Sheikh J, Sheperis C, et al. Artificial intelligence for health professions educators. NAM Perspect. 2021; 2021:10.31478/202109a.
Article69. Majumder A, Sen D. Artificial intelligence in cancer diagnostics and therapy: current perspectives. Indian J Cancer. 2021; 58:481–92.
Article70. Altamimi I, Altamimi A, Alhumimidi AS, Altamimi A, Temsah MH. Artificial intelligence (AI) chatbots in medicine: a supplement, not a substitute. Cureus. 2023; 15:e40922.
Article71. Chen RY. A traceability chain algorithm for artificial neural networks using T-S fuzzy cognitive maps in blockchain. Future Gener Comput Syst. 2018; 80:198–210.
Article72. Narneg S, Dodde S, Adedoja A, Ayyalasomayajula MMT, Chintala S. AI-driven decision support systems in management: enhancing strategic planning and execution. IJRITCC. 2024; 12:268–76.73. Galbusera F, Cina A. Image annotation and curation in radiology: an overview for machine learning practitioners. Eur Radiol Exp. 2024; 8:11.
Article74. Jeong YU, Yoo S, Kim YH, Shim WH. De-identification of facial features in magnetic resonance images: software development using deep learning technology. J Med Internet Res. 2020; 22:e22739.
Article75. Kondylakis H, Catalan R, Alabart SM, Barelle C, Bizopoulos P, Bobowicz M, et al. Documenting the de-identification process of clinical and imaging data for AI for health imaging projects. Insights Imaging. 2024; 15:130.
Article76. Ueda D, Kakinuma T, Fujita S, Kamagata K, Fushimi Y, Ito R, et al. Fairness of artificial intelligence in healthcare: review and recommendations. Jpn J Radiol. 2024; 42:3–15.
Article77. Kahn CE Jr. Hitting the mark: reducing bias in AI systems. Radiol Artif Intell. 2022; 4:e220171.
Article78. Agarwal A, Agarwal H, Agarwal N. Fairness score and process standardization: framework for fairness certification in artificial intelligence systems. AI Ethics. 2023; 3:267–79.
Article79. Fellander-Tsai L. AI ethics, accountability, and sustainability: revisiting the Hippocratic oath. Acta Orthop. 2020; 91:1–2.
Article80. Oduro S, Moss E, Metcalf J. Obligations to assess: recent trends in AI accountability regulations. Patterns (N Y). 2022; 3:100608.
Article81. Hohma E, Boch A, Trauth R, Lutge C. Investigating accountability for artificial intelligence through risk governance: a workshop-based exploratory study. Front Psychol. 2023; 14:1073686.
Article82. Vo V, Chen G, Aquino YS, Carter SM, Do QN, Woode ME. Multi-stakeholder preferences for the use of artificial intelligence in healthcare: a systematic review and thematic analysis. Soc Sci Med. 2023; 338:116357.
Article83. World Health Organization (WHO). Ethics and governance of artificial intelligence for health [Internet]. WHO;c2021. [cited 2024 Sep 1]. https://www.who.int/publications/i/item/9789240029200.84. Gradellini C, Gomez-Cantarino S, Dominguez-Isabel P, Molina-Gallego B, Mecugni D, Ugarte-Gurrutxaga MI. Cultural competence and cultural sensitivity education in university nursing courses. a scoping review. Front Psychol. 2021; 12:682920.
Article85. Cabler KA. Exploring the impact of diversity training on the development and application of cultural competence skills in higher education professionals [Dissertation]. Virginia Commonwealth University;2019.86. Alper J, Sloan SS. Data matters: ethics, data, and international research collaboration in a changing world. Proceedings of a workshop. 1st ed. National Academies Press;2018.87. Newman SD, Andrews JO, Magwood GS, Jenkins C, Cox MJ, Williamson DC. Community advisory boards in community-based participatory research: a synthesis of best processes. Prev Chronic Dis. 2011; 8:A70.88. Davies A, Ormel I, Bernier A, Harriss E, Mumba N, Gobat N, et al. A rapid review of community engagement and informed consent processes for adaptive platform trials and alternative design trials for public health emergencies. Wellcome Open Res. 2023; 8:194.
Article89. Lee CP. Design, development, and deployment of context-adaptive AI systems for enhanced user adoption. In : In: CHI EA '24: Extended Abstracts of the CHI Conference on Human Factors in Computing Systems; 2024 May 11-16; Honolulu, USA. Association for Computing Machinery;2024. p. 429.
Article90. World Health Organization (WHO). WHO issues first global report on artificial intelligence (AI) in health and six guiding principles for its design and use [Internet]. WHO;c2021. [cited 2024 Sep 1]. https://www.who.int/news/item/28-06-2021-who-issues-first-global-report-on-ai-in-health-and-six-guiding-principles-for-its-design-and-use.91. Nyariro M, Emami E, Caidor P, Abbasgholizadeh Rahimi S. Integrating equity, diversity and inclusion throughout the lifecycle of AI within healthcare: a scoping review protocol. BMJ Open. 2023; 13:e072069.
Article92. Izadi S, Forouzanfar M. Error correction and adaptation in conversational AI: a review of techniques and applications in chatbots. AI. 2024; 5:803–41.
Article93. Rambach T, Gleim P, Mandelartz S, Heizmann C, Kunze C, Kellmeyer P. Challenges and facilitation approaches for the participatory design of AI-based clinical decision support systems: protocol for a scoping review. JMIR Res Protoc. 2024; 13:e58185.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Ethics for Artificial Intelligence: Focus on the Use of Radiology Images
- Publication Ethics in the Era of Artificial Intelligence
- Issues and Trends Related to Artificial Intelligence in Research Ethics
- Can an artificial intelligence chatbot be the author of a scholarly article?
- Artificial Intelligence in Pathology