Ann Hepatobiliary Pancreat Surg.
2024 Nov;28(4):500-507. 10.14701/ahbps.24-082.
Minimally invasive pancreatoduodenectomy with combined venous vascular resection: A comparative analysis with open approach
- Affiliations
-
- 1Department of Surgery, Yonsei University College of Medicine, Seoul, Korea
- 2Department of Surgery, Yongin Severance Hospital, Yonsei University College of Medicine, Yongin, Korea
- 3Division of Hepatobiliary and Pancreatic Surgery, Department of Surgery, Yonsei University College of Medicine, Seoul, Korea
- KMID: 2561583
- DOI: http://doi.org/10.14701/ahbps.24-082
Abstract
- Backgrounds/Aims
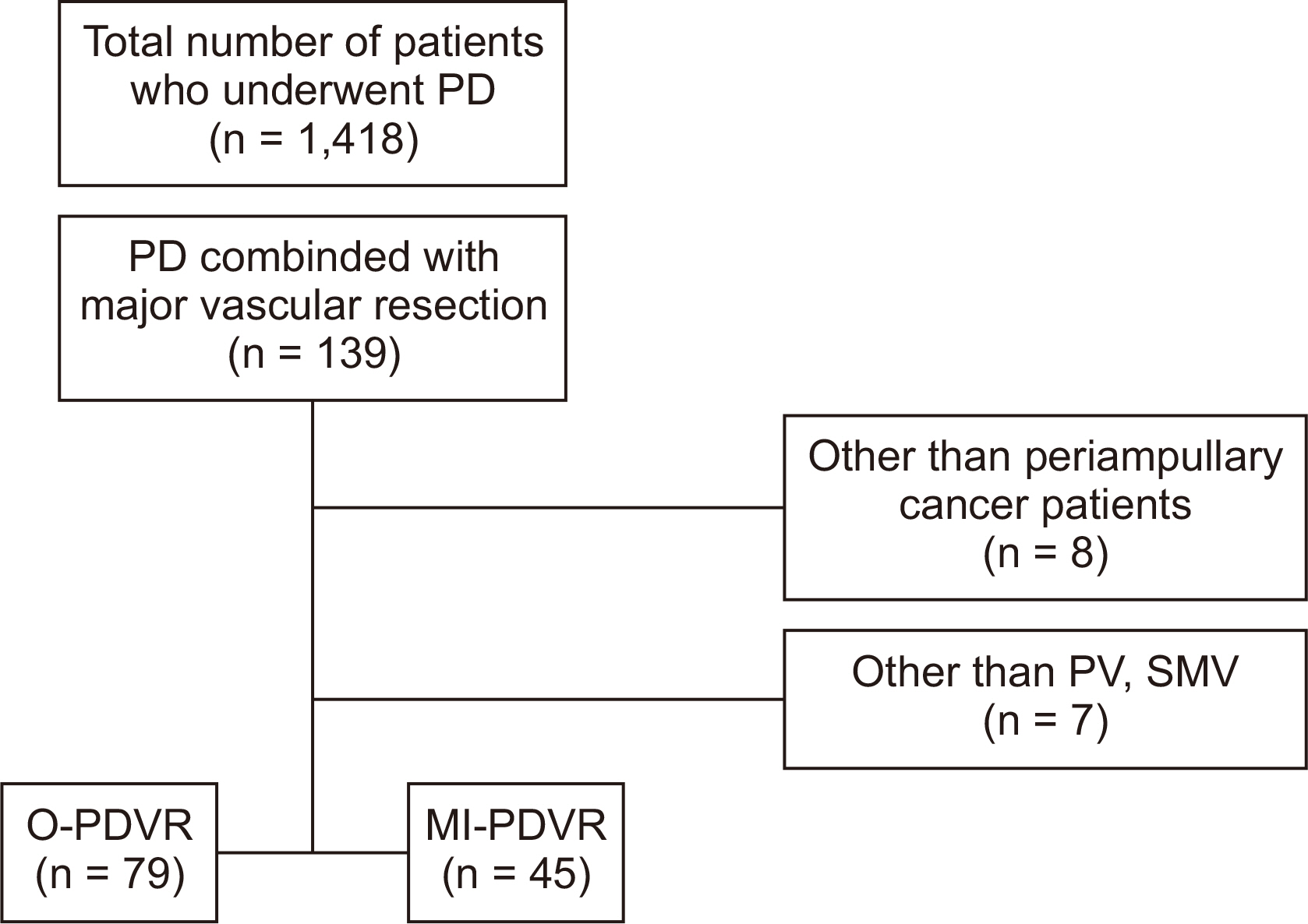
This study aimed to compare the minimally invasive pancreatoduodenectomy with venous vascular resection (MI-PDVR) and open pancreatoduodenectomy with venous vascular resection (O-PDVR) for periampullary cancer.
Methods
Data of 124 patients who underwent PDVR (45 MI-PDVR, 79 O-PDVR) between January 1, 2016, and December 31, 2023, was retrospectively reviewed.
Results
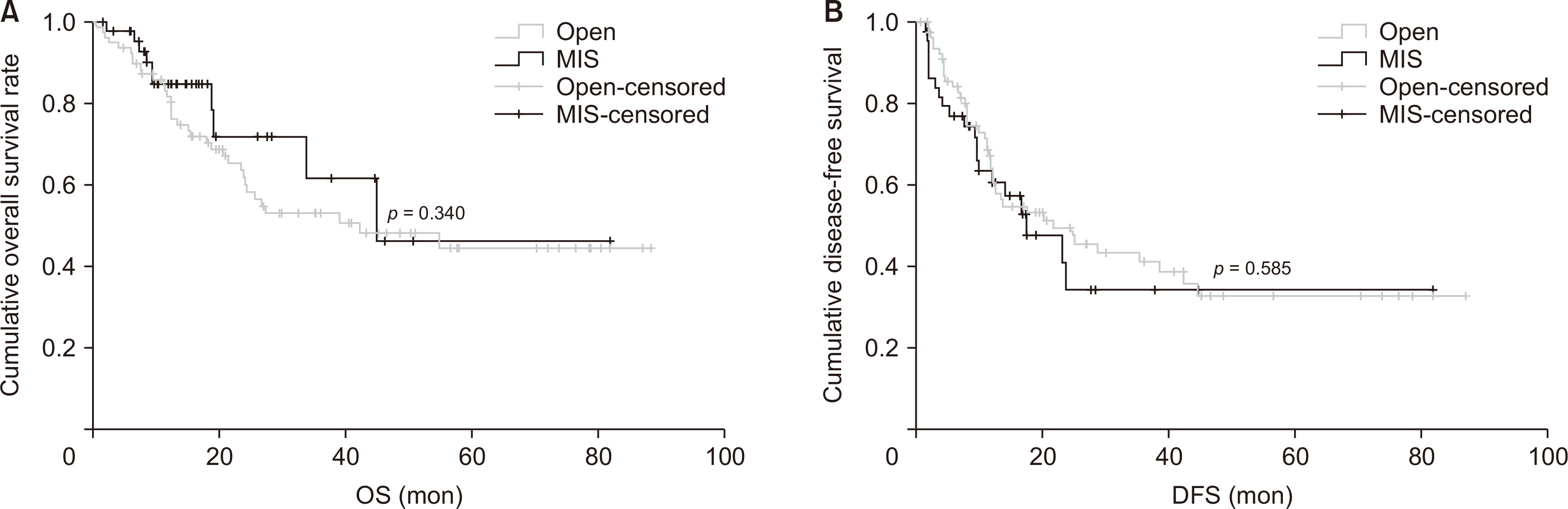
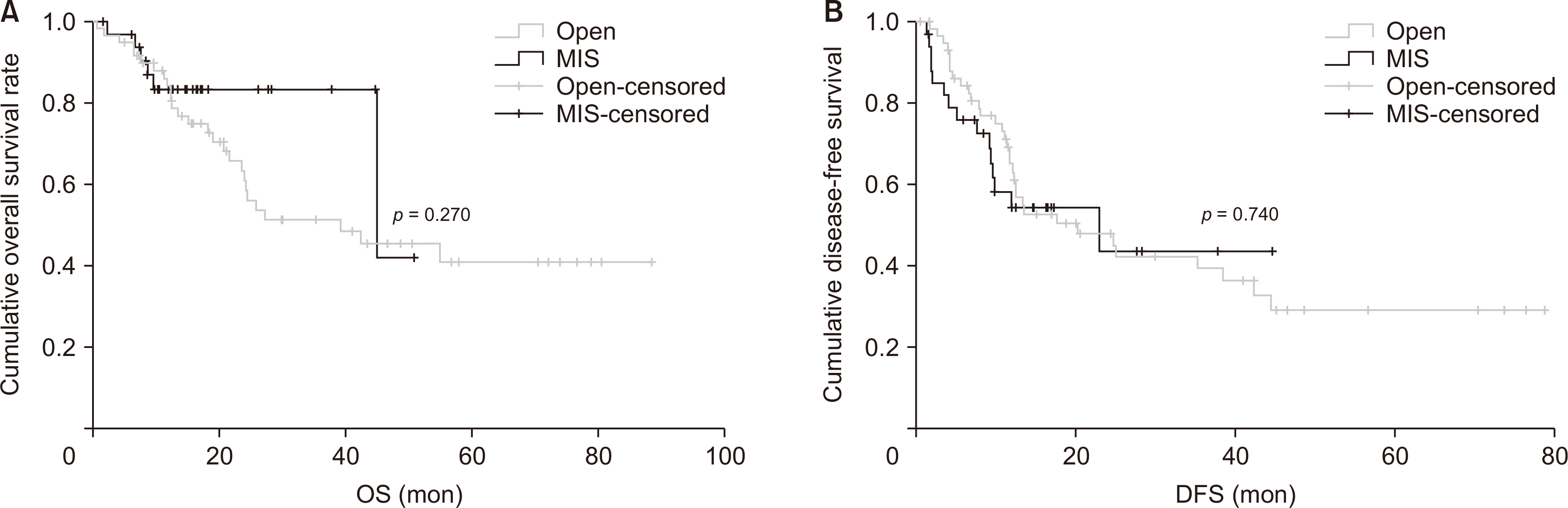
MI-PDVR is significantly better than O-PDVR in terms of perioperative outcomes (median operation time [452.69 minutes vs. 543.91 minutes; p = 0.004], estimated blood loss [410.44 mL vs. 747.59 mL; p < 0.01], intraoperative transfusion rate [2 cases vs. 18 cases; p = 0.01], and hospital stay [18.16 days vs. 23.91 days; p = 0.008]). The complications until the discharge day showed no significant difference between the two groups (Clavien–Dindo < 3, 84.4% vs. 82.3%; Clavien–Dindo ≥ 3, 15.6% vs. 17.7%; p = 0.809). In terms of long-term oncological outcomes, there was no statistical difference in overall survival (OS, 51.55 months [95% CI: 35.95–67.14] vs. median 49.92 months [95% CI: 40.97–58.87]; p = 0.340) and disease-free survival (DFS, median 35.06 months [95% CI: 21.47–48.65] vs. median 38.77 months [95% CI: 29.80–47.75]; p = 0.585), between the two groups. Long-term oncological outcomes for subgroup analysis focusing on pancreatic ductal adenocarcinoma also showed no statistical differences in OS (40.86 months [95% CI: 34.45–47.27] vs. 48.48 months [95% CI: 38.16–58.59]; p = 0.270) and DFS (24.42 months [95% CI: 17.03–31.85] vs. 34.35 months, [95% CI: 25.44–43.27]; p = 0.740).
Conclusions
MI-PDVR can provide better perioperative outcomes than O-PDVR, and has similar oncological impact.
Figure
Reference
-
References
1. Chiorean EG, Chiaro MD, Tempero MA, Malafa MP, Benson AB, Cardin DB, et al. 2023; Ampullary adenocarcinoma, version 1.2023, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw. 21:753–782. DOI: 10.6004/jnccn.2023.0034. PMID: 37433437.2. Ghaneh P, Palmer D, Cicconi S, Jackson R, Halloran CM, Rawcliffe C, et al. 2023; Immediate surgery compared with short-course neoadjuvant gemcitabine plus capecitabine, FOLFIRINOX, or chemoradiotherapy in patients with borderline resectable pancreatic cancer (ESPAC5): a four-arm, multicentre, randomised, phase 2 trial. Lancet Gastroenterol Hepatol. 8:157–168. DOI: 10.1016/S2468-1253(22)00348-X. PMID: 36521500.3. Jang JY, Han Y, Lee H, Kim SW, Kwon W, Lee KH, et al. 2018; Oncological benefits of neoadjuvant chemoradiation with gemcitabine versus upfront surgery in patients with borderline resectable pancreatic cancer: a prospective, randomized, open-label, multicenter phase 2/3 trial. Ann Surg. 268:215–222. DOI: 10.1097/SLA.0000000000002705. PMID: 29462005.4. Versteijne E, van Dam JL, Suker M, Janssen QP, Groothuis K, Akkermans-Vogelaar JM, et al. 2022; Neoadjuvant chemoradiotherapy versus upfront surgery for resectable and borderline resectable pancreatic cancer: long-term results of the dutch randomized PREOPANC trial. J Clin Oncol. 40:1220–1230. DOI: 10.1200/JCO.21.02233. PMID: 35084987.5. Versteijne E, Suker M, Groothuis K, Akkermans-Vogelaar JM, Besselink MG, Bonsing BA, et al. 2020; Preoperative chemoradiotherapy versus immediate surgery for resectable and borderline resectable pancreatic cancer: results of the dutch randomized phase III PREOPANC trial. J Clin Oncol. 38:1763–1773. DOI: 10.1200/JCO.19.02274. PMID: 32105518. PMCID: PMC8265386.6. Croome KP, Farnell MB, Que FG, Reid-Lombardo KM, Truty MJ, Nagorney DM, et al. 2015; Pancreaticoduodenectomy with major vascular resection: a comparison of laparoscopic versus open approaches. J Gastrointest Surg. 19:189–194. discussion 194DOI: 10.1007/s11605-014-2644-8. PMID: 25274069.7. Zwart ES, Yilmaz BS, Halimi A, Ahola R, Kurlinkus B, Laukkarinen J, et al. 2022; Venous resection for pancreatic cancer, a safe and feasible option? A systematic review and meta-analysis. Pancreatology. 22:803–809. DOI: 10.1016/j.pan.2022.05.001. PMID: 35697587.8. Fogliati A, Fiorentini G, Alva-Ruiz R, Abdelrahman AM, Zironda A, Lynch IT, et al. 2023; Technical outcomes of porto-mesenteric venous reconstruction in pancreatic resection using autologous left renal vein graft as conduit. J Am Coll Surg. 237:58–67. DOI: 10.1097/XCS.0000000000000744. PMID: 37158471.9. Lee JH, Kang CM, Bang SM, Choi JY, Seong JS, Hwang HK, et al. 2015; The role of neoadjuvant chemoradiation therapy in patients with borderline resectable pancreatic cancer with isolated venous vascular involvement. Medicine (Baltimore). 94:e1233. DOI: 10.1097/MD.0000000000001233. PMID: 26252282. PMCID: PMC4616587.10. Filho JELP, Tustumi F, Coelho FF, Júnior SS, Honório FCC, Henriques AC, et al. 2021; The impact of venous resection in pancreatoduodectomy: a systematic review and meta-analysis. Medicine (Baltimore). 100:e27438. DOI: 10.1097/MD.0000000000027438. PMID: 34622858. PMCID: PMC8500612.11. Aiolfi A, Lombardo F, Bonitta G, Danelli P, Bona D. 2021; Systematic review and updated network meta-analysis comparing open, laparoscopic, and robotic pancreaticoduodenectomy. Updates Surg. 73:909–922. DOI: 10.1007/s13304-020-00916-1. PMID: 33315230. PMCID: PMC8184540.12. Kamarajah SK, Bundred JR, Marc OS, Jiao LR, Hilal MA, Manas DM, et al. 2020; A systematic review and network meta-analysis of different surgical approaches for pancreaticoduodenectomy. HPB (Oxford). 22:329–339. DOI: 10.1016/j.hpb.2019.09.016. PMID: 31676255.13. Vladimirov M, Bausch D, Stein HJ, Keck T, Wellner U. 2022; Hybrid laparoscopic versus open pancreatoduodenectomy. A meta-analysis. World J Surg. 46:901–915. DOI: 10.1007/s00268-021-06372-1. PMID: 35043246. PMCID: PMC8885482.14. van Hilst J, de Rooij T, Bosscha K, Brinkman DJ, van Dieren S, Dijkgraaf MG, et al. 2019; Laparoscopic versus open pancreatoduodenectomy for pancreatic or periampullary tumours (LEOPARD-2): a multicentre, patient-blinded, randomised controlled phase 2/3 trial. Lancet Gastroenterol Hepatol. 4:199–207. DOI: 10.1016/S2468-1253(19)30004-4. PMID: 30685489.15. Wang M, Li D, Chen R, Huang X, Li J, Liu Y, et al. 2021; Laparoscopic versus open pancreatoduodenectomy for pancreatic or periampullary tumours: a multicentre, open-label, randomised controlled trial. Lancet Gastroenterol Hepatol. 6:438–447. DOI: 10.1016/S2468-1253(21)00054-6. PMID: 33915091.16. Poves I, Burdío F, Morató O, Iglesias M, Radosevic A, Ilzarbe L, et al. 2018; Comparison of perioperative outcomes between laparoscopic and open approach for pancreatoduodenectomy: the PADULAP randomized controlled trial. Ann Surg. 268:731–739. DOI: 10.1097/SLA.0000000000002893. PMID: 30138162.17. Palanivelu C, Senthilnathan P, Sabnis SC, Babu NS, Srivatsan Gurumurthy S, Anand Vijai N, et al. 2017; Randomized clinical trial of laparoscopic versus open pancreatoduodenectomy for periampullary tumours. Br J Surg. 104:1443–1450. DOI: 10.1002/bjs.10662. PMID: 28895142.18. Vissers FL, van Hilst J, Burdío F, Sabnis SC, Busch OR, Dijkgraaf MG, et al. 2022; Laparoscopic versus open pancreatoduodenectomy: an individual participant data meta-analysis of randomized controlled trials. HPB (Oxford). 24:1592–1599. DOI: 10.1016/j.hpb.2022.02.005. PMID: 35641405.19. Kauffmann EF, Napoli N, Menonna F, Vistoli F, Amorese G, Campani D, et al. 2016; Robotic pancreatoduodenectomy with vascular resection. Langenbecks Arch Surg. 401:1111–1122. DOI: 10.1007/s00423-016-1499-8. PMID: 27553112.20. Cai Y, Gao P, Li Y, Wang X, Peng B. 2018; Laparoscopic pancreaticoduodenectomy with major venous resection and reconstruction: anterior superior mesenteric artery first approach. Surg Endosc. 32:4209–4215. DOI: 10.1007/s00464-018-6167-3. PMID: 29602996.21. Wang X, Cai Y, Zhao W, Gao P, Li Y, Liu X, et al. 2019; Laparoscopic pancreatoduodenectomy combined with portal-superior mesenteric vein resection and reconstruction with interposition graft: case series. Medicine (Baltimore). 98:e14204. DOI: 10.1097/MD.0000000000014204. PMID: 30653175. PMCID: PMC6370126.22. Ouyang G, Zhong X, Cai Z, Liu J, Zheng S, Hong D, et al. 2023; The short- and long-term outcomes of laparoscopic pancreaticoduodenectomy combining with different type of mesentericoportal vein resection and reconstruction for pancreatic head adenocarcinoma: a Chinese multicenter retrospective cohort study. Surg Endosc. 37:4381–4395. DOI: 10.1007/s00464-023-09901-2. PMID: 36759356.23. Peng X, He Y, Tang Y, Yang X, Huang W, Li J, et al. 2022; Preliminary experience on laparoscopic pancreaticoduodenal combined with major venous resection and reconstruction anastomosis. Front Surg. 9:974214. DOI: 10.3389/fsurg.2022.974214. PMID: 36157401. PMCID: PMC9492958.24. Sung MK, Song KB, Hong S, Park Y, Kwak BJ, Jun E, et al. 2023; Laparoscopic versus open pancreaticoduodenectomy with major vein resection for pancreatic head cancer. J Hepatobiliary Pancreat Sci. 30:970–982. DOI: 10.1002/jhbp.1317. PMID: 36740999.25. Jie Z, Zhou X, Haibiao W, Ying D, Chen B, Li H. 2023; Major venous repair or reconstruction during laparoscopic pancreatic surgery: a single center's experience. J Laparoendosc Adv Surg Tech A. 33:890–896. DOI: 10.1089/lap.2022.0546. PMID: 37074117.26. Connie LCK, Hong SS, Kang I, Rho SY, Hwang HK, Lee WJ, et al. 2021; Adverse impact of intraoperative conversion on the postoperative course following laparoscopic pancreaticoduodenectomy. Yonsei Med J. 62:836–842. DOI: 10.3349/ymj.2021.62.9.836. PMID: 34427070. PMCID: PMC8382729.27. Lof S, Vissers FL, Klompmaker S, Berti S, Boggi U, Coratti A, et al. 2021; Risk of conversion to open surgery during robotic and laparoscopic pancreatoduodenectomy and effect on outcomes: international propensity score-matched comparison study. Br J Surg. 108:80–87. DOI: 10.1093/bjs/znaa026. PMID: 33640946.28. Li ZL, Li M, Xiong JJ, Lu HM. 2023; The impact of conversion during minimally invasive pancreatoduodenectomy: a meta-analysis. Asian J Surg. 46:1539–1540. DOI: 10.1016/j.asjsur.2022.09.074. PMID: 36253255.29. Yin T, Qin T, Wei K, Shen M, Zhang Z, Wen J, et al. 2022; Comparison of safety and effectiveness between laparoscopic and open pancreatoduodenectomy: a systematic review and meta-analysis. Int J Surg. 105:106799. DOI: 10.1016/j.ijsu.2022.106799. PMID: 35988720.30. Choi M, Hwang HK, Lee WJ, Kang CM. 2021; Total laparoscopic pancreaticoduodenectomy in patients with periampullary tumors: a learning curve analysis. Surg Endosc. 35:2636–2644. DOI: 10.1007/s00464-020-07684-4. PMID: 32495184.31. Navarro JG, Kang CM. 2019; Pitfalls for laparoscopic pancreaticoduodenectomy: need for a stepwise approach. Ann Gastroenterol Surg. 3:254–268. DOI: 10.1002/ags3.12242. PMID: 31131354. PMCID: PMC6524087.32. Kuroki T, Fujioka H. 2019; Training for laparoscopic pancreaticoduodenectomy. Surg Today. 49:103–107. DOI: 10.1007/s00595-018-1668-1. PMID: 29748825.33. Hogg ME, Besselink MG, Clavien PA, Fingerhut A, Jeyarajah DR, Kooby DA, et al. 2017; Training in minimally invasive pancreatic resections: a paradigm shift away from "see one, do one, teach one". HPB (Oxford). 19:234–245. DOI: 10.1016/j.hpb.2017.01.016. PMID: 28190709.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Minimally invasive versus open central pancreatectomy: A systematic review and meta-analysis
- Uniportal, Transforaminal Endoscopic Thoracic Discectomy: Review and Technical Note
- Laparoscopic Resection of Presacral Tumor: A New Approach in the Era of the Minimally Invasive Surgery
- Transient mesoportal shunt: An innovative technique for maintaining portal flow during pancreatoduodenectomy with portal vein resection
- Laparoscopic pancreaticoduodenectomy in pancreatic ductal adenocarcinoma