Ann Hepatobiliary Pancreat Surg.
2024 Nov;28(4):483-493. 10.14701/ahbps.24-049.
Comparative accuracy of four guidelines to predict high-grade dysplasia or malignancy in surgically resected pancreatic intraductal papillary mucinous neoplasms: Small nuances between guidelines lead to vastly different results
- Affiliations
-
- 1Department of Internal Medicine, University of Virginia Health System, Charlottesville, VA, USA
- 2Division of Gastroenterology and Hepatology, University of Virginia Health System, Charlottesville, VA, USA
- 3Division of Surgical Oncology, University of Virginia Health System, Charlottesville, VA, USA
- KMID: 2561581
- DOI: http://doi.org/10.14701/ahbps.24-049
Abstract
- Backgrounds/Aims
The guidelines regarding the management of intraductal papillary mucinous neoplasms (IPMNs) all have slightly different surgical indications for high-risk lesions. We aim to retrospectively compare the accuracy of four guidelines in recommending surgery for high-risk IPMNs, and assess the accuracy of elevated CA-19-9 levels and imaging characteristics of IPMNs considered high-risk in predicting malignancy or high-grade dysplasia (HGD).
Methods
The final histopathological diagnosis of surgically resected high-risk IPMNs during 2013−2020 were compared to preoperative surgical indications, as enumerated in four guidelines: the 2015 American Gastroenterological Association (AGA), 2017 International Consensus, 2018 European Study Group, and 2018 American College of Gastroenterology (ACG). Surgery was considered “justified” if histopathology of the surgical specimen showed HGD/malignancy, or there was postoperative symptomatic improvement.
Results
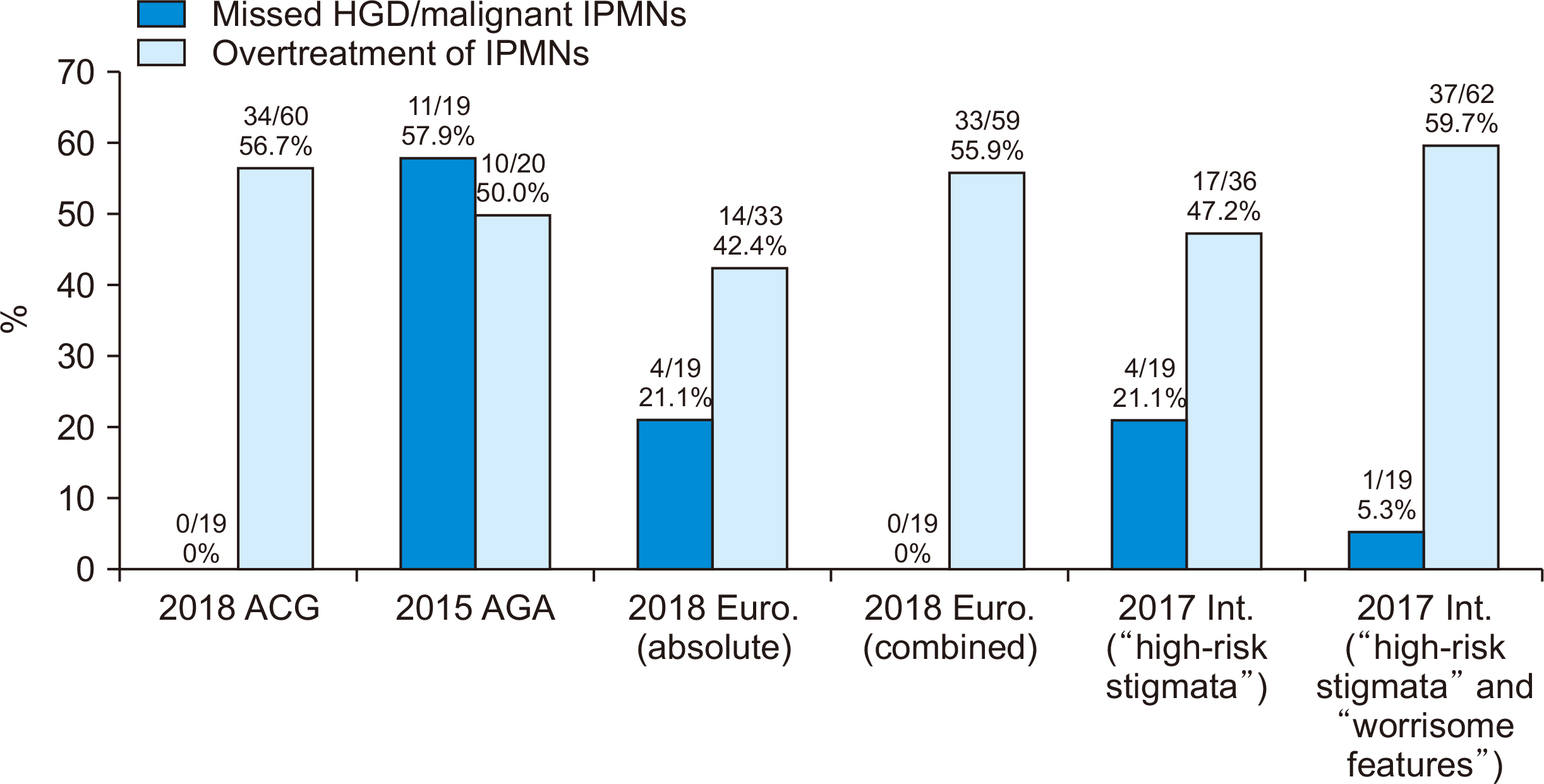
Surgery was postoperatively justified in 26/65 (40.0%) cases. All IPMNs with HGD/malignancy were detected by the 2018 ACG and the combined (absolute and relative criteria) 2018 European guidelines. The combined (“high-risk stigmata” and “worrisome features”) 2017 International guideline missed 1/19 (5.3%) IPMNs with HGD/malignancy. The 2015 AGA guideline missed the most cases (11/19, 57.9%) of IPMNs with HGD/malignancy. We found the features most-associated with HGD/malignancy were pancreatic ductal dilation, and elevated CA-19-9 levels.
Conclusions
Following the 2015 AGA guideline results in the highest rate of missed HGD/malignancy, but the lowest rate of operating on IPMNs without these features; meanwhile, the 2018 ACG and the combined (absolute and relative criteria) 2018 European guidelines result in more operations for IPMNs without HGD/malignancy, but the lowest rates of missed HGD/malignancy in IPMNs.
Figure
Reference
-
References
1. Salvia R, Fernández-del Castillo C, Bassi C, Thayer SP, Falconi M, Mantovani W, et al. 2004; Main-duct intraductal papillary mucinous neoplasms of the pancreas: clinical predictors of malignancy and long-term survival following resection. Ann Surg. 239:678–685. discussion 685–687. DOI: 10.1097/01.sla.0000124386.54496.15. PMID: 15082972. PMCID: PMC1356276.2. Zaheer A, Pokharel SS, Wolfgang C, Fishman EK, Horton KM. 2013; Incidentally detected cystic lesions of the pancreas on CT: review of literature and management suggestions. Abdom Imaging. 38:331–341. DOI: 10.1007/s00261-012-9898-y. PMID: 22534872.3. Elta GH, Enestvedt BK, Sauer BG, Lennon AM. 2018; ACG clinical guideline: diagnosis and management of pancreatic cysts. Am J Gastroenterol. 113:464–479. DOI: 10.1038/ajg.2018.14. PMID: 29485131.4. Buerlein RCD, Shami VM. 2021; Management of pancreatic cysts and guidelines: what the gastroenterologist needs to know. Ther Adv Gastrointest Endosc. 14:26317745211045769. DOI: 10.1177/26317745211045769. PMID: 34589706. PMCID: PMC8474323.5. Scheiman JM, Hwang JH, Moayyedi P. 2015; American gastroenterological association technical review on the diagnosis and management of asymptomatic neoplastic pancreatic cysts. Gastroenterology. 148:824–848.e22. DOI: 10.1053/j.gastro.2015.01.014. PMID: 25805376.6. Ferrone CR, Correa-Gallego C, Warshaw AL, Brugge WR, Forcione DG, Thayer SP, et al. 2009; Current trends in pancreatic cystic neoplasms. Arch Surg. 144:448–454. DOI: 10.1001/archsurg.2009.36. PMID: 19451487. PMCID: PMC3806091.7. Pagliari D, Saviano A, Serricchio ML, Dal Lago AA, Brizi MG, Lanza F, et al. 2017; Uptodate in the assessment and management of intraductal papillary mucinous neoplasms of the pancreas. Eur Rev Med Pharmacol Sci. 21:2858–2874.8. Scheiman JM. 2017; Pancreatic cysts - part 1: using the American Gastroenterological Association guidelines for the management of pancreatic cysts-a practical approach. Pancreas. 46:742–744. DOI: 10.1097/MPA.0000000000000832. PMID: 28609360.9. Anand N, Sampath K, Wu BU. 2013; Cyst features and risk of malignancy in intraductal papillary mucinous neoplasms of the pancreas: a meta-analysis. Clin Gastroenterol Hepatol. 11:913–921. quiz e59–e60. DOI: 10.1016/j.cgh.2013.02.010. PMID: 23416279.10. Kolb JM, Argiriadi P, Lee K, Liu X, Bagiella E, Gupta S, et al. 2018; Higher growth rate of branch duct intraductal papillary mucinous neoplasms associates with worrisome features. Clin Gastroenterol Hepatol. 16:1481–1487. DOI: 10.1016/j.cgh.2018.02.050. PMID: 29535058.11. Pergolini I, Sahora K, Ferrone CR, Morales-Oyarvide V, Wolpin BM, Mucci LA, et al. 2017; Long-term risk of pancreatic malignancy in patients with branch duct intraductal papillary mucinous neoplasm in a referral center. Gastroenterology. 153:1284–1294.e1. DOI: 10.1053/j.gastro.2017.07.019. PMID: 28739282.12. Ridtitid W, DeWitt JM, Schmidt CM, Roch A, Stuart JS, Sherman S, et al. 2016; Management of branch-duct intraductal papillary mucinous neoplasms: a large single-center study to assess predictors of malignancy and long-term outcomes. Gastrointest Endosc. 84:436–445. DOI: 10.1016/j.gie.2016.02.008. PMID: 26905937.13. Vege SS, Ziring B, Jain R, Scheiman JM, Hwang JH, Moayyedi P. 2017; Optimal strategies for pancreatic cyst surveillance: we need better comparative data, not more case series. Gastrointest Endosc. 85:685–686. DOI: 10.1016/j.gie.2016.09.007. PMID: 28215775.14. Marchegiani G, Pollini T, Andrianello S, Tomasoni G, Biancotto M, Javed AA, et al. 2021; Progression vs cyst stability of branch-duct intraductal papillary mucinous neoplasms after observation and surgery. JAMA Surg. 156:654–661. DOI: 10.1001/jamasurg.2021.1802. PMID: 34009303. PMCID: PMC8135059.15. Lobo JM, Scheiman JM, Zaydfudim VM, Shami VM, Sauer BG. 2020; Clinical and economic outcomes of patients undergoing guideline-directed management of pancreatic cysts. Am J Gastroenterol. 115:1689–1697. DOI: 10.14309/ajg.0000000000000730. PMID: 32558682.16. Hsiao CY, Yang CY, Wu JM, Kuo TC, Tien YW. 2016; Utility of the 2006 Sendai and 2012 Fukuoka guidelines for the management of intraductal papillary mucinous neoplasm of the pancreas: a single-center experience with 138 surgically treated patients. Medicine (Baltimore). 95:e4922. DOI: 10.1097/MD.0000000000004922. PMID: 27661043. PMCID: PMC5044913.17. Xu MM, Yin S, Siddiqui AA, Salem RR, Schrope B, Sethi A, et al. 2017; Comparison of the diagnostic accuracy of three current guidelines for the evaluation of asymptomatic pancreatic cystic neoplasms. Medicine (Baltimore). 96:e7900. DOI: 10.1097/MD.0000000000007900. PMID: 28858107. PMCID: PMC5585501.18. Vege SS, Ziring B, Jain R, Moayyedi P. Clinical Guidelines Committee; American Gastroenterology Association. 2015; American gastroenterological association institute guideline on the diagnosis and management of asymptomatic neoplastic pancreatic cysts. Gastroenterology. 148:819–822. quize12–13. DOI: 10.1053/j.gastro.2015.02.029.19. Tanaka M, Fernández-Del Castillo C, Kamisawa T, Jang JY, Levy P, Ohtsuka T, et al. 2017; Revisions of international consensus Fukuoka guidelines for the management of IPMN of the pancreas. Pancreatology. 17:738–753. DOI: 10.1016/j.pan.2017.07.007. PMID: 28735806.20. European Study Group on Cystic Tumours of the Pancreas. 2018; European evidence-based guidelines on pancreatic cystic neoplasms. Gut. 67:789–804. DOI: 10.1136/gutjnl-2018-316027. PMID: 29574408. PMCID: PMC5890653.21. Moriya T, Hashimoto Y, Traverso LW. 2011; The duration of symptoms predicts the presence of malignancy in 210 resected cases of pancreatic intraductal papillary mucinous neoplasms. J Gastrointest Surg. 15:762–770. discussion 770–771. DOI: 10.1007/s11605-011-1437-6. PMID: 21380634.22. Shin SH, Han DJ, Park KT, Kim YH, Park JB, Kim SC. 2010; Validating a simple scoring system to predict malignancy and invasiveness of intraductal papillary mucinous neoplasms of the pancreas. World J Surg. 34:776–783. DOI: 10.1007/s00268-010-0416-5. PMID: 20127242.23. van Huijgevoort NCM, Hoogenboom SAM, Lekkerkerker SJ, Busch OR, Del Chiaro M, Fockens P, et al. 2023; Diagnostic accuracy of the AGA, IAP, and European guidelines for detecting advanced neoplasia in intraductal papillary mucinous neoplasm/neoplasia. Pancreatology. 23:251–257. DOI: 10.1016/j.pan.2023.01.011. PMID: 36805049.24. Park RHS, Lim GRS, Wu JJY, Koh YX, Teo JY, Cheow PC, et al. 2020; Validation of the clinical utility of 4 guidelines in the initial triage of mucinous cystic lesions of the pancreas based on cross-sectional imaging: experience with 188 surgically-treated patients. Eur J Surg Oncol. 46:2114–2121. DOI: 10.1016/j.ejso.2020.07.027. PMID: 32828582.25. Vanden Bulcke A, Jaekers J, Topal H, Vanbeckevoort D, Vandecaveye V, Roskams T, et al. 2021; Evaluating the accuracy of three international guidelines in identifying the risk of malignancy in pancreatic cysts: a retrospective analysis of a surgical treated population. Acta Gastroenterol Belg. 84:443–450. DOI: 10.51821/84.3.006. PMID: 34599569.26. Crippa S, Fogliati A, Valente R, Sadr-Azodi O, Arnelo U, Capurso G, et al. 2021; A tug-of-war in intraductal papillary mucinous neoplasms management: comparison between 2017 International and 2018 European guidelines. Dig Liver Dis. 53:998–1003. DOI: 10.1016/j.dld.2021.03.009. PMID: 33846103.27. Sharib JM, Fonseca AL, Swords DS, Jaradeh K, Bracci PM, Firpo MA, et al. 2018; Surgical overtreatment of pancreatic intraductal papillary mucinous neoplasms: do the 2017 International Consensus Guidelines improve clinical decision making? Surgery. 164:1178–1184. DOI: 10.1016/j.surg.2018.07.014. PMID: 30170819.28. Watanabe Y, Endo S, Nishihara K, Ueda K, Mine M, Tamiya S, et al. 2018; The validity of the surgical indication for intraductal papillary mucinous neoplasm of the pancreas advocated by the 2017 revised International Association of Pancreatology consensus guidelines. Surg Today. 48:1011–1019. DOI: 10.1007/s00595-018-1691-2. PMID: 29961172.29. Giannone F, Crippa S, Aleotti F, Palumbo D, Belfiori G, Partelli S, et al. 2022; Improving diagnostic accuracy and appropriate indications for surgery in pancreatic cystic neoplasms: the role of EUS. Gastrointest Endosc. 96:648–656.e2. DOI: 10.1016/j.gie.2022.05.009. PMID: 35618030.30. Singhi AD, Zeh HJ, Brand RE, Nikiforova MN, Chennat JS, Fasanella KE, et al. 2016; American Gastroenterological Association guidelines are inaccurate in detecting pancreatic cysts with advanced neoplasia: a clinicopathologic study of 225 patients with supporting molecular data. Gastrointest Endosc. 83:1107–1117.e2. DOI: 10.1016/j.gie.2015.12.009. PMID: 26709110.31. Lekkerkerker SJ, Besselink MG, Busch OR, Verheij J, Engelbrecht MR, Rauws EA, et al. 2017; Comparing 3 guidelines on the management of surgically removed pancreatic cysts with regard to pathological outcome. Gastrointest Endosc. 85:1025–1031. DOI: 10.1016/j.gie.2016.09.027. PMID: 27693645.32. Tanaka M, Fernández-del Castillo C, Adsay V, Chari S, Falconi M, Jang JY, et al. 2012; International consensus guidelines 2012 for the management of IPMN and MCN of the pancreas. Pancreatology. 12:183–197. DOI: 10.1016/j.pan.2012.04.004. PMID: 22687371.33. Krishna S, Abdelbaki A, Hart PA, Machicado JD. 2024; Endoscopic ultrasound-guided needle-based confocal endomicroscopy as a diagnostic imaging biomarker for intraductal papillary mucinous neoplasms. Cancers (Basel). 16:1238. DOI: 10.3390/cancers16061238. PMID: 38539568. PMCID: PMC10969577.34. Singhi AD, McGrath K, Brand RE, Khalid A, Zeh HJ, Chennat JS, et al. 2018; Preoperative next-generation sequencing of pancreatic cyst fluid is highly accurate in cyst classification and detection of advanced neoplasia. Gut. 67:2131–2141. DOI: 10.1136/gutjnl-2016-313586. PMID: 28970292. PMCID: PMC6241612.35. Rosenbaum MW, Jones M, Dudley JC, Le LP, Iafrate AJ, Pitman MB. 2017; Next-generation sequencing adds value to the preoperative diagnosis of pancreatic cysts. Cancer Cytopathol. 125:41–47. DOI: 10.1002/cncy.21775. PMID: 27647802.36. Paniccia A, Polanco PM, Boone BA, Wald AI, McGrath K, Brand RE, et al. 2023; Prospective, multi-institutional, real-time next-generation sequencing of pancreatic cyst fluid reveals diverse genomic alterations that improve the clinical management of pancreatic cysts. Gastroenterology. 164:117–133.e7.37. Krishna SG, Hart PA, DeWitt JM, DiMaio CJ, Kongkam P, Napoleon B, et al. 2020; EUS-guided confocal laser endomicroscopy: prediction of dysplasia in intraductal papillary mucinous neoplasms (with video). Gastrointest Endosc. 91:551–563.e5. DOI: 10.1016/j.gie.2019.09.014. PMID: 31542380.38. Konda VJ, Meining A, Jamil LH, Giovannini M, Hwang JH, Wallace MB, et al. 2013; A pilot study of in vivo identification of pancreatic cystic neoplasms with needle-based confocal laser endomicroscopy under endosonographic guidance. Endoscopy. 45:1006–1013. DOI: 10.1055/s-0033-1344714. PMID: 24163192.39. Nakai Y, Iwashita T, Park DH, Samarasena JB, Lee JG, Chang KJ. 2015; Diagnosis of pancreatic cysts: EUS-guided, through-the-needle confocal laser-induced endomicroscopy and cystoscopy trial: DETECT study. Gastrointest Endosc. 81:1204–1214. DOI: 10.1016/j.gie.2014.10.025. PMID: 25634486.40. Feng Y, Chang X, Zhao Y, Wu D, Meng Z, Wu X, et al. 2021; A new needle-based confocal laser endomicroscopy pattern of malignant pancreatic mucinous cystic lesions (with video). Endosc Ultrasound. 10:200–206. DOI: 10.4103/eus.eus_35_20. PMID: 32655084. PMCID: PMC8248307.41. Hata T, Dal Molin M, Hong SM, Tamura K, Suenaga M, Yu J, et al. 2017; Predicting the grade of dysplasia of pancreatic cystic neoplasms using cyst fluid DNA methylation markers. Clin Cancer Res. 23:3935–3944. DOI: 10.1158/1078-0432.CCR-16-2244. PMID: 28148542. PMCID: PMC5511555.42. Hong SM, Omura N, Vincent A, Li A, Knight S, Yu J, et al. 2012; Genome-wide CpG island profiling of intraductal papillary mucinous neoplasms of the pancreas. Clin Cancer Res. 18:700–712. DOI: 10.1158/1078-0432.CCR-11-1718. PMID: 22173550. PMCID: PMC3271174.43. Majumder S, Taylor WR, Yab TC, Berger CK, Dukek BA, Cao X, et al. 2019; Novel methylated DNA markers discriminate advanced neoplasia in pancreatic cysts: marker discovery, tissue validation, and cyst fluid testing. Am J Gastroenterol. 114:1539–1549. DOI: 10.14309/ajg.0000000000000284. PMID: 31306149. PMCID: PMC7294458.44. Shirakami Y, Iwashita T, Uemura S, Imai H, Murase K, Shimizu M. 2021; Micro-RNA analysis of pancreatic cyst fluid for diagnosing malignant transformation of intraductal papillary mucinous neoplasm by comparing intraductal papillary mucinous adenoma and carcinoma. J Clin Med. 10:2249. DOI: 10.3390/jcm10112249. PMID: 34067335. PMCID: PMC8196884.45. Sato Y, Suzuki R, Takagi T, Sugimoto M, Ohira H. 2020; Circulating extracellular vesicle-encapsulated microRNA as screening biomarkers for intraductal papillary mucinous neoplasm. Oncol Lett. 20:315. Erratum in: Oncol Lett 2021;22:611. DOI: 10.3892/ol.2021.12872. PMID: 34188713. PMCID: PMC8227474.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Successful Treated Intraductal Papillary Mucinous Neoplasm with Pancreatitis
- Management Strategy and Surveillance of Intraductal Papillary Mucinous Neoplasm–Gastroenterologist’s Viewpoint
- The Incidental Pancreatic Cyst: When to Worry About Cancer
- Intraductal Papillary Mucinous Tumor Simultaneously Involving the Liver and Pancreas: A Case Report
- Malignant Pancreatic Intraductal Papillary Mucinous Neoplasm with Splenic Invasion: A Case Report